Abstract
Study Design
Retrospective case series.
Objectives
To describe the indications, operative course, and outcomes in eight pediatric patients who underwent occiput-to-pelvis (O-P) spinal arthrodesis.
Summary
Spinal arthrodesis from the occiput to pelvis is needed for some children with extensive spine deformity. There are few reports of patients with O-P arthrodesis.
Methods
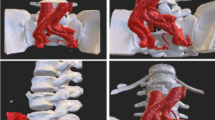
We reviewed records of pediatric patients who underwent spinal arthrodesis to treat spine deformity between 1987 and 2017 at one institution. Eight patients (six girls) who underwent staged O-P arthrodesis were identified. Underlying conditions, indications for surgery, medical comorbidities, operative courses, complications, and imaging of these patients were recorded.
Results
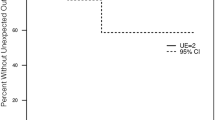
Diagnoses were neuromuscular disorders in five patients and syndromic disorders in three patients. Mean ages were 9.7 ± 4.1 years at index surgery and 16.8 ± 4.6 years at completion of O-P arthrodesis. Patients underwent a mean of three operations (range, two to five). Occipitocervical arthrodesis was the final operation in six of eight patients (all but the two patients with Loeys-Dietz syndrome). Mean follow-up after the last procedure was 8.5 ± 7.1 years. Two patients underwent revision for protruding occipital implants, and one patient underwent revision for thoracic pseudarthrosis. No patients developed postoperative infections or new neurologic deficits. At final follow-up, Scoliosis Research Society–22r questionnaire scores were lowest for Function (2.6 ± 1.0 of 5 possible points) and highest for Satisfaction (4.1 ± 1.4).
Conclusions
O-P arthrodesis can benefit patients with extensive spine deformity from neuromuscular or syndromic causes. Patients were young at first operation, which may suggest that younger patients are at higher risk than older patients of major progression of deformity in other spinal regions after deformity correction. Health-related quality of life and radiographic outcomes suggest that patients who underwent O-P arthrodesis had satisfactory outcomes and maintenance of correction during a mean of 8.5 years of follow-up.
Level of Evidence
Level IV, therapeutic study.
Similar content being viewed by others
References
Agabegi SS, Kazemi N, Sturm PF, et al. Natural history of adolescent idiopathic scoliosis in skeletally mature patients: a critical review. J Am Acad Orthop Surg 2015;23:714–23.
Trobisch PD, Ducoffe AR, Lonner BS, et al. Choosing fusion levels in adolescent idiopathic scoliosis. J Am Acad Orthop Surg 2013;21:519–28.
Balioglu MB, Albayrak A, Atici Y, et al. Scoliosis-associated cervical spine pathologies. Spine Deform 2014;2:131–42.
Martinez-Del-Campo E, Turner JD, Kalb S, et al. Occipitocervical fixation: a single surgeon’s experience with 120 patients. Neurosurgery 2016;79:549–60.
McKay SD, Al-Omari A, Tomlinson LA, et al. Review of cervical spine anomalies in genetic syndromes. Spine (Phila Pa 1976) 2012;37:E269–77.
Odent T, Bou Ghosn R, Dusabe JP, et al. Internal fixation with occipital hooks construct for occipito-cervical arthrodesis. Results in 14 young or small children. Eur Spine J 2015;24:94–100.
Vialle R, Thevenin-Lemoine C, Mary P. Neuromuscular scoliosis. Orthop Traumatol Surg Res 2013;99:S124–39.
Jain A, Sullivan BT, Kuwabara A, et al. Sacral-alar-iliac fixation in children with neuromuscular scoliosis: minimum 5-year follow-up. World Neurosurg 2017;108:474–8.
Gjolaj JP, Sponseller PD, Shah SA, et al. Spinal deformity correction in Marfan syndrome versus adolescent idiopathic scoliosis: learning from the differences. Spine (Phila Pa 1976) 2012;37:1558–65.
Sponseller PD, Yang JS, Thompson GH, et al. Pelvic fixation of growing rods: comparison of constructs. Spine (Phila Pa 1976) 2009;34:1706–10.
Jain A, Hassanzadeh H, Strike SA, et al. Pelvic fixation in adult and pediatric spine surgery: historical perspective, indications, and techniques. AAOS Exhibit Selection. J Bone Joint Surg Am 2015;97:1521–8.
Reames DL, Smith JS, Fu KMG, et al. Complications in the surgical treatment of 19,360 cases of pediatric scoliosis: a review of the Scoliosis Research Society Morbidity and Mortality database. Spine (Phila Pa 1976) 2011;36:1484–91.
Zang L, Hai Y, Yuan S, et al. Distal adding-on and risk factors in severe and rigid scoliosis. Spine (Phila Pa 1976) 2017;42:160–8.
Haidar RK, Kassak K, Masrouha K, et al. Reliability and validity of an adapted Arabic version of the Scoliosis Research Society-22r Questionnaire. Spine (Phila Pa 1976) 2015;40:E971–7.
Monticone M, Baiardi P, Calabro D, et al. Development of the Italian version of the revised Scoliosis Research Society-22 Patient Questionnaire, SRS-22r-I: cross-cultural adaptation, factor analysis, reliability, and validity. Spine (Phila Pa 1976) 2010;35:E1412–7.
Angelliaume A, Harper L, Lalioui A, et al. Tailor-made management of thoracic scoliosis with cervical hyperextension in muscular dystrophy. Eur Spine J 2018;27:264–9.
Liu BP, Aghaei Lasboo A, Rozenfeld M, et al. Percutaneous transosseous translaminar approach for thecal sac access in advanced ankylosing spondylitis with instrumented posterior spinal fusion. AJNR Am J Neuroradiol 2010;31:193–5.
Sponseller PD, Takenaga RK, Newton P, et al. The use of traction in the treatment of severe spinal deformity. Spine (Phila Pa 1976) 2008;33:2305–9.
Erkula G, Sponseller PD, Paulsen LC, et al. Musculoskeletal findings of Loeys-Dietz syndrome. J Bone Joint Surg Am 2010;92:1876–83.
Suk KS, Baek JH, Park JO, et al. Postoperative quality of life in patients with progressive neuromuscular scoliosis and their parents. Spine J 2015;15:446–53.
Lai SM, Asher M, Burton D. Estimating SRS-22 quality of life measures with SF-36: application in idiopathic scoliosis. Spine (Phila Pa 1976) 2006;31:473–8.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author disclosures: MJH (other from Charles E. Silberstein Research Fellowship, during the conduct of the study), OA (none), BTS (none), PDS (grants and personal fees from Johnson & Johnson, USA; personal fees from the Journal of Bone and Joint Surgery, Globus, and Orthopediatrics, outside the submitted work).
This study was approved by the Johns Hopkins Institutional Review Board (IRB00145796).
Funding statement: Matthew J. Hadad received salary support from the Charles E. Silberstein Research Fellowship. No other authors received funding for this study.
Rights and permissions
About this article
Cite this article
Hadad, M.J., Abousamra, O., Sullivan, B.T. et al. Occiput-to-Pelvis Spinal Arthrodesis: A Case Series. Spine Deform 7, 992–1002 (2019). https://doi.org/10.1016/j.jspd.2019.04.006
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2019.04.006