Abstract
Purpose
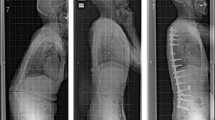
This study aimed to compare the functional and radiographic outcomes of two surgical interventions for adult spinal deformity (ASD): anterior lumbar interbody fusion with anterior column realignment (ALIF-ACR) and posterior approach using Smith–Peterson osteotomy with transforaminal lumbar interbody fusion and pedicle screw fixation (TLIF-Schwab2).
Methods
A retrospective cohort study included 61 ASD patients treated surgically between 2019 and 2020 at a single tertiary orthopedic specialty hospital. Patients were divided into two groups: Group 1 (ALIF-ACR, 29 patients) and Group 2 (TLIF-Schwab2, 32 patients). Spinopelvic radiographic parameters and functional outcomes were evaluated at 3, 6, and 12 months postsurgery.
Results
Perioperative outcomes favored the ALIF-ACR group, with significantly smaller blood loss, shorter hospital stay, and operative time. Radiographic and functional outcomes were similar for both groups; however, the ALIF-ACR group did have a greater degree of correction in lumbar lordosis at 12 months. Complication profiles varied, with the ALIF-ACR group experiencing mostly hardware-related complications, while the TLIF-Schwab2 group faced dural tears, wound dehiscence, and proximal junctional kyphosis. Both groups had similar revision rates.
Conclusion
Both ALIF-ACR and TLIF-Schwab2 achieved similar radiographic and functional outcomes in ASD patients with moderate sagittal plane deformity at 1-year follow-up. However, the safety profiles of the two techniques differed. Further research is required to optimize patient selection for each surgical approach, aiming to minimize perioperative complications and reoperation rates in this challenging patient population.






Similar content being viewed by others
References
Bess S, Line B, Fu KM et al (2016) The health impact of symptomatic adult spinal deformity: comparison of deformity types to united states population norms and chronic diseases. Spine 41(3):224–233. https://doi.org/10.1097/brs.0000000000001202
Passias PG, Jalai CM, Line BG et al (2018) Patient profiling can identify patients with adult spinal deformity (ASD) at risk for conversion from nonoperative to surgical treatment: initial steps to reduce ineffective ASD management. Spine J 18(2):234–244. https://doi.org/10.1016/j.spinee.2017.06.044
Schwab F, Blondel B, Chay E et al (2014) The comprehensive anatomical spinal osteotomy classification. Neurosurgery 74(1):112–120. https://doi.org/10.1227/NEU.0000000000000182o
Uribe JS, Schwab F, Mundis GM et al (2018) The comprehensive anatomical spinal osteotomy and anterior column realignment classification: presented at the 2018 AANS/CNS joint section on disorders of the spine and peripheral nerves. J Neurosurg Spine 29(5):565–575. https://doi.org/10.3171/2018.4.SPINE171206
Hills JM, Yoon ST, Rhee JM et al (2019) Anterior column realignment (ACR) with and without Pre-ACR posterior release for fixed sagittal deformity. Int J Spine Surg 13(2):192–198. https://doi.org/10.14444/6026
Schwab FJ, Patel A, Shaffrey CI et al (2012) Sagittal realignment failures following pedicle subtraction osteotomy surgery: are we doing enough? J Neurosurg Spine 16(6):539–546. https://doi.org/10.3171/2012.2.Spine11120
Mummaneni PVM, Shaffrey CI, Lenke LG et al (2014) The minimally invasive spinal deformity surgery algorithm: a reproducible rational framework for decision making in minimally invasive spinal deformity surgery. Neurosurg Focus 36(5):E6. https://doi.org/10.3171/2014.3.FOCUS1413
Lee YC, Lee R (2019) Minimal invasive surgical algorithm for revision lumbar spinal surgery. J Spine Surg 5(4):413–424. https://doi.org/10.21037/jss.2019.09.08
Mummaneni PV, Hussain I, Shaffrey CI et al (2021) The minimally invasive interbody selection algorithm for spinal deformity. J Neurosurg Spine 34(5):741–748. https://doi.org/10.3171/2020.9.SPINE20230
Li B, Hawryluk G, Mummaneni PV et al (2021) Utility of the MISDEF2 algorithm and extent of fusion in open adult spinal deformity surgery with minimum 2-year follow-up. Neurospine 18(4):824–832. https://doi.org/10.14245/ns.2142508.254
Junker R, Dimakis A, Thoneick M, Jansen JA (2009) Effects of implant surface coatings and composition on bone integration: a systematic review. Clin Oral Implants Res 20:185–206
Wennerberg A, Albrektsson T (2009) Effects of titanium surface topography on bone integration: a systematic review. Clin Oral Implant Res 20:172–184. https://doi.org/10.1111/j.1600-0501.2009.01775.x
Ponte A, Orlando G, Siccardi GL (2018) The true ponte osteotomy: by the one who developed it. Spine Deform 6(1):2–11. https://doi.org/10.1016/j.jspd.2017.06.006
Gum JL, Reddy D, Glassman S (2016) Transforaminal lumbar interbody fusion (TLIF). JBJS Essent Surg Tech 6(2):e22–e22. https://doi.org/10.2106/jbjs.st.15.00003
Schwab FJ, Hawkinson N, Lafage V et al (2012) Risk factors for major peri-operative complications in adult spinal deformity surgery: a multi-center review of 953 consecutive patients. Eur Spine J. https://doi.org/10.1007/s00586-012-2370-4
Carlson BB, Saville P, Dowdell J et al (2019) Restoration of lumbar lordosis after minimally invasive transforaminal lumbar interbody fusion: a systematic review. Spine J 19(5):951–958. https://doi.org/10.1016/j.spinee.2018.10.017
Godzik J, Pereira BdA, Hemphill C et al (2020) Minimally invasive anterior longitudinal ligament release for anterior column realignment. Global Spine J 10(2):101S-110S. https://doi.org/10.1177/2192568219880178
Bokov A, Kalinina S, Leontev A, Mlyavykh S (2022) Circumferential fusion employing transforaminal versus direct lateral lumbar interbody fusion—a potential impact on implants stability. Front Surg 9:827999. https://doi.org/10.3389/fsurg.2022.827999
Olivares-Navarrete R, Hyzy SL, Slosar PJ, Schneider JM, Schwartz Z, Boyan BD (2015) Implant materials generate different peri-implant inflammatory factors. Spine 40(6):399–404. https://doi.org/10.1097/brs.0000000000000778
Gimble JM, Polini A, Pisignano D, Parodi M, Quarto R, Scaglione S (2011) Osteoinduction of human mesenchymal stem cells by bioactive composite scaffolds without supplemental osteogenic growth factors. PLoS ONE 6(10):e26211. https://doi.org/10.1371/journal.pone.0026211
Fujibayashi S, Takemoto M, Neo M et al (2011) A novel synthetic material for spinal fusion: a prospective clinical trial of porous bioactive titanium metal for lumbar interbody fusion. Eur Spine J 20(9):1486–1495. https://doi.org/10.1007/s00586-011-1728-3
Ham DW, Jung CW, Chang DG, Yang JJ, Song KS (2023) Feasibility of non-window three-dimensional–printed porous titanium cage in posterior lumbar interbody fusion: a pilot trial. Clin Orthop Surg 09(15):e66. https://doi.org/10.4055/cios22404
Woodfield T, Shum J, Linkhorn W et al (2023) Going low: low modulus graft-free 3d-printed titanium interbody cages show comparable bone formation to peek with graft. Orthop Proc 105(SUPP_3):99–99. https://doi.org/10.1302/1358-992X.2023.3.099
Akbarnia BA, Mundis GM, Moazzaz P et al (2014) Anterior column realignment (ACR) for focal kyphotic spinal deformity using a lateral transpsoas approach and all release. J Spinal Disord Tech 27(1):29–39. https://doi.org/10.1097/BSD.0b013e318287bdc1
Berjano P, Cecchinato R, Sinigaglia A et al (2015) Anterior column realignment from a lateral approach for the treatment of severe sagittal imbalance: a retrospective radiographic study. Eur Spine J 24:433–438. https://doi.org/10.1007/s00586-015-3930-1
Hosseini P, Mundis GM, Eastlack RK et al (2017) Preliminary results of anterior lumbar interbody fusion, anterior column realignment for the treatment of sagittal malalignment. Neurosurg Focus 43(6):E6. https://doi.org/10.3171/2017.8.FOCUS17423
Formica M, Quarto E, Zanirato A et al (2020) Lateral lumbar interbody fusion: what is the evidence of indirect neural decompression? A systematic review of the literature. HSS J 16(2):143–154. https://doi.org/10.1007/s11420-019-09734-7
Tung K-K, Tseng W-C, Wu Y-C et al (2023) Comparison of radiographic and clinical outcomes between ALIF, OLIF, and TLIF over 2-year follow-up: a comparative study. J Orthop Surg Res 18(1):1–12. https://doi.org/10.1186/s13018-023-03652-5
Tohmeh AG, Jabbouri SS, Vesselle A, Howell KM (2021) Short-segment minimally disruptive anterior column release for focal sagittal deformity correction of the thoracolumbar spine. N Am Spine Soc J (NASSJ) 6:100068. https://doi.org/10.1016/j.xnsj.2021.100068
Mundis GM, Turner JD, Kabirian N et al (2017) anterior column realignment has similar results to pedicle subtraction osteotomy in treating adults with sagittal plane deformity. World Neurosurg 105:249–256. https://doi.org/10.1016/j.wneu.2017.05.122
Lak AM, Lamba N, Pompilus F et al (2021) Minimally invasive versus open surgery for the correction of adult degenerative scoliosis: a systematic review. Springer, pp 659–668
Uribe JS, Deukmedjian AR, Mummaneni PV et al (2014) Complications in adult spinal deformity surgery: an analysis of minimally invasive, hybrid, and open surgical techniques. Neurosurg Focus 36(5):E15. https://doi.org/10.3171/2014.3.FOCUS13534
Bassani R, Gregori F, Peretti G (2019) Evolution of the anterior approach in lumbar spine fusion. World Neurosurg 131:391–398. https://doi.org/10.1016/j.wneu.2019.07.023
Ogura Y, Ogura K, Kobayashi Y et al (2020) Minimum clinically important difference of major patient-reported outcome measures in patients undergoing decompression surgery for lumbar spinal stenosis. Clin Neurol Neurosurg 196:105966. https://doi.org/10.1016/j.clineuro.2020.105966
Staartjes VE, Siccoli A, de Wispelaere MP, Schröder ML (2019) Patient-reported outcomes unbiased by length of follow-up after lumbar degenerative spine surgery: do we need 2 years of follow-up? Spine J 19(4):637–644. https://doi.org/10.1016/j.spinee.2018.10.004
Asher AL, Kerezoudis P, Mummaneni PV et al (2018) Defining the minimum clinically important difference for grade I degenerative lumbar spondylolisthesis: insights from the quality outcomes database. Neurosurg Focus 44(1):E2. https://doi.org/10.3171/2017.10.Focus17554
Bae J, Theologis AA, Strom R et al (2018) Comparative analysis of 3 surgical strategies for adult spinal deformity with mild to moderate sagittal imbalance. J Neurosurg Spine 28(1):40–49. https://doi.org/10.3171/2017.5.SPINE161370
Crawford CH, Glassman SD, Bridwell KH, Berven SH, Carreon LY (2015) The minimum clinically important difference in srs-22r total score, appearance, activity and pain domains after surgical treatment of adult spinal deformity. Spine 40(6):377–381. https://doi.org/10.1097/brs.0000000000000761
Liu S, Schwab F, Smith JS et al (2014) Likelihood of reaching minimal clinically important difference in adult spinal deformity: a comparison of operative and nonoperative treatment. Ochsner J Spring 14(1):67–77
Yuan L, Zeng Y, Chen Z, Li W, Zhang X, Ni J (2020) Risk factors associated with failure to reach minimal clinically important difference after correction surgery in patients with degenerative lumbar scoliosis. Spine 45(24):E1669–E1676. https://doi.org/10.1097/brs.0000000000003713
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
DK is a consultant for Spineart and SI Bone and receives royalties from Spineart that are not related to this study. Other authors do not have conflicts of interest to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Denisov, A., Rowland, A., Zaborovskii, N. et al. Moderate sagittal plane deformity patients have similar radiographic and functional outcomes with either anterior or posterior surgery. Eur Spine J 33, 620–629 (2024). https://doi.org/10.1007/s00586-023-08075-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-08075-8