Abstract
Study Design
Retrospective review of a prospectively collected multicenter database.
Objectives
To evaluate the evolution of surgical treatment strategies, complications, and patient-reported outcomes for adult spinal deformity (ASD) patients.
Summary of Background Data
ASD surgery is associated with high complication rates. Evolving treatment strategies may reduce these risks.
Methods
Adult patients undergoing ASD surgery from 2009 to 2016 were analyzed (n = 905). Preoperative and surgical parameters were compared across years. Subgroup analysis of 436 patients with minimum two-year follow-up was also performed.
Results
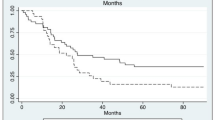
From 2009 to 2016, there was a significant increase in the mean preoperative age (52 to 63.1, p < .001), body mass index (26.3 to 32.2, p = .003), Charlson Comorbidity index (1.4 to 2.2, p < .001), rate of previous spine surgery (39.8% to 53.1%, p = .01), and baseline disability (visual analog scale [VAS] back and leg pain) scores (p < .01), Oswestry Disability Index, and 22–item Scoliosis Research Society Questionnaire scores (p < .001). Preoperative Schwab sagittal alignment modifiers and overall surgical invasiveness index were similar across time. Three-column osteotomy utilization decreased from 36% in 2011 to 16.7% in 2016. Lateral lumbar interbody fusion increased from 6.4% to 24.1% (p = .004), anterior lumbar interbody fusion decreased from 22.9% to 16.7% (p = .043), and transforaminal lumbar interbody fusion/posterior lumbar interbody fusion utilization remained similar (p = .448). Use of recombinant human bone morphogenetic protein-2 (rhBMP-2) in 2012 was 84.6%, declined to 58% in 2013, and rebounded to 76.3% in 2016 (p = .006). Tranexamic acid use increased rapidly from 2009 to 2016 (13.3% to 48.6%, p < .001). Two-year follow-up sagittal vertical axis, pelvic tilt, pelvic incidence—lumbar lordosis, and maximum Cobb angles were similar across years. Intraoperative complications decreased from 33% in 2010 to 9.3% in 2016 (p < .001). Perioperative ( < 30 days, < 90 days) complications peaked in 2010 (42.7%, 46%) and decreased by 2016 (24.1%, p < .001; 29.6%, p = .007). The overall complication rate decreased from 73.2% in 2008–2014 patients to 62.6% in 2015–2016 patients (p = .03). Two-year health-related quality of life outcomes did not significantly differ across the years (p > .05).
Conclusions
From 2009 to 2016, despite an increasingly elderly, medically compromised, and obese patient population, complication rates decreased. Evolving strategies may result in improved treatment of ASD patients.
Level of Evidence
Level IV.
Similar content being viewed by others
References
Reid DBC, Daniels AH, Ailon T, et al. Frailty and health-related quality of life improvement following adult spinal deformity surgery. World Neurosurg 2018;112:e548–54.
Smith JS, Lafage V, Shaffrey CI, et al. Outcomes of operative and nonoperative treatment for adult spinal deformity. Neurosurgery 2016;78:851–61.
Teles AR, Mattei TA, Righesso O, Falavigna A. Effectiveness of operative and nonoperative care for adult spinal deformity: systematic review of the literature. Glob Spine J 2017;7:170–8.
Sing DC, Berven SH, Burch S, Metz LN. Increase in spinal deformity surgery in patients age 60 and older is not associated with increased complications. Spine J 2017;17:627–35.
Passias PG, Poorman GW, Jalai CM, et al. Morbidity of adult spinal deformity surgery in, elderly has declined over time. Spine (Phila Pa 1976) 2017;42:E978–82.
Sing DC, Khanna R, Shaw JD, et al. Increasing rates of surgical management of multilevel spinal curvature in elderly patients. Spine Deform 2016;4:365–72.
Zygourakis CC, Liu CY, Keefe M, et al. Analysis of national rates, cost, and sources of cost variation in adult spinal deformity. Neurosurgery 2018;82:378–87.
McCarthy I, Hostin R, O’Brien M, et al. Health economic analysis of adult deformity surgery. Neurosurg Clin N Am 2013;24:293–304.
Miller E, Jain A, Daniels AH, et al. Assessment of a novel adult spinal deformity (ASD) Frailty Index (ASD-FI) to assist with risk stratification for ASD surgery. Spine J 2016;16:S365.
Miller E, Sciubba DM, Neuman BJ, et al. Development and external validation of the adult spine deformity (ASD) Frailty Index (ASD-FI). Spine J 2016;16:S310–1.
Scheer JK, Hostin R, Robinson C, et al; International Spine Study Group. Operative management of adult spinal deformity results in significant increases in QALYs gained compared to nonoperative management: analysis of 479 patients with minimum 2-year follow-up. Spine (Phila Pa 1976) 2018;43:339–47.
Passias PG, Klineberg EO, Jalai CM, et al. Hospital readmission within 2 years following adult thoracolumbar spinal deformity surgery. Spine (Phila Pa 1976) 2016;41:1355–64.
Gomez JA, Lafage V, Scuibba DM, et al. Adult scoliosis deformity surgery. Spine (Phila Pa 1976) 2017;42:992–8.
Passias PG, Horn SR, Jalai CM, et al. Comparative analysis of perioperative complications between a multicenter prospective cervical deformity database and the Nationwide Inpatient Sample database. Spine J 2017;17:1633–40.
Mundis GM, Turner JD, Deverin V, et al. A critical analysis of sagittal plane deformity correction with minimally invasive adult spinal deformity surgery: a 2-year follow-up study. Spine Deform 2017;5:265–71.
Gum JL, Carreon LY, Kelly MP, et al. Cell saver for adult spinal deformity surgery reduces cost. Spine Deform 2017;5:272–6.
Bridwell KH, Lenke LG, McEnery KW, et al. Anterior fresh frozen structural allografts in the thoracic and lumbar spine. Do they work if combined with posterior fusion and instrumentation in adult patients with kyphosis or anterior column defects? Spine (Phila Pa 1976) 1995;20:1410–8.
Schwab FJ, Blondel B, Bess S, et al. Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity. Spine (Phila Pa 1976) 2013;38:E803–12.
Glassman SD, Bridwell K, Dimar JR, et al. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 2005;30(18):2024–9.
Glassman SD, Berven S, Bridwell K, et al. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976) 2005;30:682–8.
Gum JL, Carreon LY, Buchowski JM, et al. Utilization trends of pedicle subtraction osteotomies compared to posterior spinal fusion for deformity: a national database analysis between 2008–2011. Scoliosis Spinal Disord 2016;11:25.
Auerbach JD, Lenke LG, Bridwell KH, et al. Major complications and comparison between 3–column osteotomy techniques in 105 consecutive spinal deformity procedures. Spine (Phila Pa 1976) 2012;37:1198–210.
Mobbs RJ, Phan K, Malham G, et al. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg (Hong Kong) 2015;1:2–18.
Theologis AA, Mundis GM, Nguyen S, et al. Utility of multilevel lateral interbody fusion of the thoracolumbar coronal curve apex in adult deformity surgery in combination with open posterior instrumentation and L5—S1 interbody fusion: a case-matched evaluation of 32 patients. J Neurosurg Spine 2017;26:208–19.
De la Garza Ramos R, Nakhla J, Nasser R, et al. Volume-outcome relationship after 1 and 2 level anterior cervical discectomy and fusion. World Neurosurg 2017;105:543–8.
Cole T, Veeravagu A, Zhang M, Ratliff JK. Surgeon procedure volume and complication rates in anterior cervical discectomy and fusions. J Spinal Disord Tech 2014;30:1.
Lador R, Bandiera S, Gasbarrini A, et al. Treatment of spinal tumors in a high volume center has direct impact on local recurrence, morbidity, and mortality. Clin Spine Surg 2017;30: E1074–81.
Schoenfeld AJ, Sturgeon DJ, Burns CB, et al. Establishing benchmarks for the volume-outcome relationship for common lumbar spine surgical procedures. Spine J 2018;18:22–8.
Paul JC, Lonner BS, Goz V, et al. Complication rates are reduced for revision adult spine deformity surgery among high-volume hospitals and surgeons. Spine J 2015;15:1963–72.
Van Hal M, Lee J, Laudermilch D, et al. Vancomycin powder regimen for prevention of surgical site infection in complex spine surgeries. Clin Spine Surg 2017;30:E1062–5.
Kang DG, Holekamp TF, Wagner SC, Lehman RA. Intrasite vancomycin powder for the prevention of surgical site infection in spine surgery: a systematic literature review. Spine J 2015;15:762–70.
Winter SF, Santaguida C, Wong J, Fehlings MG. Systemic and topical use of tranexamic acid in spinal surgery: a systematic review. Glob Spine J 2016;6:284–95.
Yuan QM, Zhao ZH, Xu BS. Efficacy and safety of tranexamic acid in reducing blood loss in scoliosis surgery: a systematic review and meta-analysis. Eur Spine J 2017;26:131–9.
Colomina MJ, Koo M, Basora M, et al. Intraoperative tranexamic acid use in major spine surgery in adults: a multicentre, randomized, placebo-controlled trial. Br J Anaesth 2017;118:380–90.
Palumbo MA, Shah KN, Eberson CP, et al. Outrigger rod technique for supplemental support of posterior spinal arthrodesis. Spine J 2015;15:1409–14.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Author disclosures: AHD (grants and personal fees from Orthofix; personal fees from Stryker and SpineArt; other from Springer, outside the submitted work), DBCR (none), SNT (none), RAH (other from American Orthopaedic Association; other from Cervical Spine Research Society [CSRS] ; personal fees and other from DePuy, Globus Medical, SeaSpine, and ISSLS Textbook of the Lumbar Spine; personal fees from Medtronic; grants from Misonix; other from North America Spine Society, personal fees from Orthofix, Inc.; other from Scoliosis Research Society, Western Ortho Association, and International Spine Study Group [ISSG], outside the submitted work; in addition, RAH has a patent DePuy with royalties paid, a patent Globus Medical with royalties paid, and a patent SeaSpine with royalties paid), EOK (grants and personal fees from AO Spine and DePuy; grants from OREF; personal fees from K2M, Springer, Stryker, and Trevena, outside the submitted work), SB (grants from DePuy Synthes, during the conduct of the study; grants and personal fees from K2 Medical; personal fees from Pioneer and Allosource; grants from DePuy Synthes, Medtronic, and NuVasive, outside the submitted work), DB (grants from Bioventis; personal fees and other from DePuy; grants from Pfizer; other from Scoliosis Research Society and Spine Deformity, outside the submitted work; in addition, SB has a patent DePuy with royalties paid), 1SS (grants from DePuy Synthes/ISSG, during the conduct of the study; personal fees from Zimmer Biomet, NuVasive, K2M, and Allosource; grants from DePuy Synthes/ISSG, Neurosurgery Research and Education Foundation, and AOSpine, outside the submitted work), CS (other from American Association of Neurological Surgeons and American Board of Neurological Surgery; personal fees from Biomet; other from CSRS; grants from DePuy; personal fees from K2M and Medtronic; personal fees and other from Medtronic Sofamor Danek and NuVasive; other from Scoliosis Research Society, Spinal Deformity, and Spine; personal fees from Stryker and Zimmer, outside the submitted work; in addition, CS has a patent Zimmer with royalties paid), MG (personal fees and other from DePuy; other from European Spine lournal, Global Spine lournal, lohnson & lohnson, Proctor and Gamble, and Spine Deformity, outside the submitted work), CPA (grants and personal fees from NuVasive; personal fees from K2M, DePuy Synthes, and NociMed; grants from SeaSpine, outside the submitted work), DKH (none), VLF (grants and personal fees from DePuy; other from ISSG; personal fees from Medtronic, other from Nemaris INC and Scoliosis Research Society, outside the submitted work), FS (grants from DePuy; personal fees and other from K2M; personal fees from Medicrea, NuVasive, and Medtronic; other from Medtronic Sofamor Danek, Nemaris, Scoliosis Research Society, Spine Deformity, and ISSG; personal fees and other from Zimmer, outside the submitted work; in addition, FS has a patent K2M with royalties paid, a patent Medtronic Sofamor Danek with royalties paid, and a patent Zimmer with royalties paid), RE (other from Alphatec; grants, personal fees, nonfinancial support, and other from NuVasive; personal fees from Globus Medical and K2M; personal fees and nonfinancial support from SeaSpine; personal fees from Titan and SI Bone; other from Spine Innovation and NuTech, personal fees from Eli Lilly, outside the submitted work), BA (grants and personal fees from NuVasive; personal fees from K2M, DePuy Synthes, and NociMed; grants from SeaSpine, outside the submitted work), H1K (other from AO spine, ISSG Foundation, Scoliosis Research Society, HSS lournal, and Asian Spine lournal; personal fees from K2M and Zimmer Biomet, outside the submitted work), MK (grants from DePuy Synthes Spine, outside the submitted work), PGP (grants from DePuy Synthes, during the conduct of the study; personal fees from Medicrea, SpineWave, Zimmer Biomet, Globus, Allosource, and Aesculap; grants from CSRS, outside the submitted work), TP (grants from CSRS; personal fees from Globus Medical, Innovasis, Medicrea International, and NuVasive; grants from Zimmer, outside the submitted work), GMM (personal fees from DePuy; other from ISSG Foundation and K2M; grants, personal fees, and other from NuVasive, outside the submitted work; in addition, GMM has a patent K2M with royalties paid), ISSG (grants from DePuy Synthes Spine, K2M, NuVasive, Biomet, and Orthofix, during the conduct of the study; grants from Medtronic and Stryker, outside the submitted work).This study was funded by the International Spine Study Group Foundation (ISSGF).
IRB approval: Institutional review board approval was obtained at all participating institutions for collection and analysis of patient data.
Rights and permissions
About this article
Cite this article
Daniels, A.H., Reid, D.B.C., Tran, S.N. et al. Evolution in Surgical Approach, Complications, and Outcomes in an Adult Spinal Deformity Surgery Multicenter Study Group Patient Population. Spine Deform 7, 481–488 (2019). https://doi.org/10.1016/j.jspd.2018.09.013
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2018.09.013