Abstract
Study Design
Retrospective radiographic review.
Objectives
To understand the effect of variability in sacral endplate selection in transitional lumbosacral vertebrae (TLSV) and its impact on pelvic, regional, and global spinal alignment parameters.
Background
TLSV can have the characteristics of both lumbar and sacral vertebrae. Difficulties in identification of the S1 endplate may come from nomenclature, number of lumbar vertebrae, sacra, and morphology and may influence the interpretation and consistency of spinal alignment parameters.
Methods
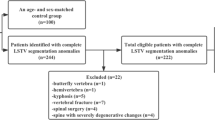
Patients with TLSV were identified and radiographic measurements including pelvic incidence (PI), pelvic tilt (PT), sacral slope (SS), lumbar lordosis (LL), sagittal vertical axis (SVA), T1-pelvic angle (TPA), pelvic incidence-lumbar lordosis (PI-LL) mismatch, thoracic kyphosis (TK), and spinal inclination (T1SPi) were obtained. Radiographic measurements were performed twice with the sacral endplate at the cephalad and caudal options. Paired t tests assessed the difference between different selection groups.
Results
Of 1,869 patients, 70 (3.7%) were found to have TLSV on radiographic imaging. Fifty-eight (82.9%) had lumbarized sacral segments whereas 12 (17.1%) had sacralized lumbar segments. T1-SPi (mean: −1.77°) and TK (mean: 34.86°) did not vary from altering sacral endplate selection. Selection of the caudal TLSV as the sacral endplate resulted in an increase in all pelvic parameters (PI: 66.8° vs. 44.3°, PT: 25.1° vs. 12.7°, and SS: 41.6° vs. 31.6°), regional lumbar parameters (LL: −54.1° vs. 44.0°, PI-LL: 12.7° vs. 0.3°), and global parameters (SVA: 46.1 mm vs. 28.3 mm, TPA: 23.3° vs. 10.8°) as compared to selecting the cephalad TLSV. All mean differences between radiographic parameters were found to be statistically significant (p < .001).
Conclusions
Variation in sacral endplate selection in TLSV significantly affects spinal alignment parameter measurements. A standardized method for measuring TLSV is needed to reduce measurement error and ultimately allow more accurate understanding of alignment targets in patients with TLSV.
Level of Evidence
Level III.
Similar content being viewed by others
References
Castellvi AE, Goldsteinn LA, Chan DPK. Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine (Phila Pa 1976) 1984;9:493–5.
Spinal Deformity Study Group In: O’Brien MF, Kuklo TR, Blanke KM, et al., editors. Radiographic Measurement Manual. Memphis, TN: Medtronic Sofamor Danek USA; 2004.
Lowe T, Berven S, Schwab FJ, et al. The SRS classification for adult spinal deformity: building on the King/Moe and Lenke classification systems. Spine (Phila Pa 1976) 2006;31:S119–25.
Farshad-Amacker NA, Aichmair A, Herzog RJ, et al. Merits of different anatomical landmarks for correct numbering of the lumbar vertebrae in lumbosacral transitional anomalies. Eur Spine J 2015;24:600–8.
Price R, Okamoto M, Le Huec J, et al. Normative spino-pelvic parameters in patients with the lumbarization of S1 compared to a normal asymptomatic population. Eur Spine J 2016;25:3694–8.
Dominguez D, Faundez A, Demezon H, et al. Normative values for the L5 incidence in a subgroup of transitional anomalies extracted from 147 asymptomatic subjects. Eur Spine J 2016;25:3602–7.
Tang M, Yang XF, Yang SW, et al. Lumbosacral transitional vertebra in a population-based study of 5860 individuals: prevalence and relationship to low back pain. Eur J Radiol 2014;83:1679–82.
Apazidis A, Ricart PA, Diefenbach CM, et al. The prevalence of transitional vertebrae in the lumbar spine. Spine J 2011;11:858–62.
Tins BJ, Balain B. Incidence of numerical variants and transitional lumbosacral vertebrae on whole-spine MRI. Insights Imaging 2016;7:199–203.
Coskun Benlidayi I, Cuzdan Coskun N, Basaran S. Does lumbosacral transitional vertebra have any influence on sacral tilt? Spine (Phila Pa 1976) 2015;40:1.
French HD, Schaefer NR, Laherty RW. Lumbosacral transitional vertebrae and its prevalence in the Australian Population. Glob Spine J 2014;4:229–32.
Josiah DT, Boo S, Tarabishy A, et al. Anatomical differences in patients with lumbosacral transitional vertebrae and implications for minimally invasive spine surgery. J Neurosurg Spine 2017;26:137–43.
Jancuska JM, Spivak JM, Bendo JA. A review of symptomatic lumbosacral transitional vertebrae: Bertolotti’s syndrome. Int J Spine Surg 2015;9:42.
Hu Z, Zhang Z, Zhao Z, et al. A neglected point in surgical treatment of adolescent idiopathic scoliosis: variations in the number of vertebrae. Medicine (Baltimore) 2016;95:e4682.
Illeez OG, Atici A, Ulger EB, et al. The transitional vertebra and sacroiliac joint dysfunction association. Eur Spine J 2018;27:187–93.
Nardo L, Alizai H, Virayavanich W, et al. Lumbosacral transitional vertebrae: association with low back pain. Radiology 2012;265: 497–503.
Legaye J, Duval-Beaupère G, Hecquet J, et al. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 1998;7:99–103.
Crawford CHI, Glassman SD, Gum JL, et al. Conflicting calculations of pelvic incidence and pelvic tilt secondary to transitional lumbosacral anatomy (lumbarization of S-1): case report. J Neurosurg Spine 2017;26:45–9.
Protopsaltis TS, Schwab FJ, Bronsard N, et al. The T1 pelvic angle, a novel radiographic measure of global sagittal deformity, accounts for both spinal inclination and pelvic tilt and correlates with health-related quality of life. J Bone Joint Surg Am 2014;96:1631–40.
Schwab FJ, Patel A, Ungar B, et al. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976) 2010;35:2224–31.
Schwab FJ, Blondel B, Bess S, et al. Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976) 2013;38: E803–12.
Farshad-Amacker NA, Lurie B, Herzog RJ, et al. Is the iliolumbar ligament a reliable identifier of the L5 vertebra in lumbosacral transitional anomalies? Eur Radiol 2014;24:2623–30.
Farshad-Amacker NA, Herzog RJ, Hughes AP, et al. Associations between lumbosacral transitional anatomy types and degeneration at the transitional and adjacent segments. Spine J 2015;15:1210–6.
Luoma K, Vehmas T, Raininko R, et al. Lumbosacral transitional vertebra: relation to disc degeneration and low back pain. Spine (Phila Pa 1976) 2004;29:200–5.
Konin GP, Walz DM. Lumbosacral transitional vertebrae: classification, imaging findings, and clinical relevance. Am J Neuroradiol 2010;31:1778–86.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author disclosures: PLZ (none), JYM (none), JCT (none), TJE (none), TSP (grants from DePuy Synthes Spine, during the conduct of the study; personal fees from Medicrea International, grants from Zimmer Spine, outside the submitted work), PGP (personal fees from SpineWave, personal fees Zimmer-Biomet, grants from CSRS, outside the submitted work), AJB (none).
Rights and permissions
About this article
Cite this article
Zhou, P.L., Moon, J.Y., Tishelman, J.C. et al. Interpretation of Spinal Radiographic Parameters in Patients With Transitional Lumbosacral Vertebrae. Spine Deform 6, 587–592 (2018). https://doi.org/10.1016/j.jspd.2018.01.004
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2018.01.004