Abstract
Study Design
Surgeon survey.
Objectives
To determine if magnetic resonance imaging (MRI) following implantation of magnetically controlled growing rods (MCGRs) is associated with any adverse events.
Summary of Background Data
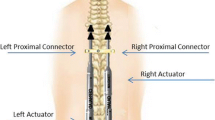
Magnetically controlled growing rods have been shown to reduce the need for repeated surgical procedures and improve costs when compared to traditional growing rods, but concerns about MRI compatibility exist. MRIs are often clinically indicated in the EOS population.
Methods
Pediatric spine surgeons who are members of the Growing Spine Study Group, Children’s Spine Study Group, and early international users of this technology were surveyed regarding MRI use after performing MCGR surgery.
Results
A total of 118 surgeons were surveyed. Four surgeons reported that 10 patients had an MRI with an implanted MCGR. Loss of fixation (0%, 0/10), movement of implants (0%, 0/10), unintended lengthening/shortening (0%, 0/10), or noticeable heating of MCGR (0%, 0/10) were not observed. No problems were observed with function of the MCGR following MRI, and a mean of 2.1 mm was obtained at the next lengthening (range, 0.5-3.0 mm). Two patients had brain MRIs, both of which could be interpreted. All cervical spine MRIs could be interpreted without excessive artifact (100%, 7/7). Six patients had MRIs of the thoracic or lumbar spine, but these were considered uninterpretable as a result of artifact from the MCGR device (0%, 0/6).
Conclusion
These are the first reported cases of MRI use in humans with MCGR. There were no adverse events observed. MCGR rods lengthened as expected following MRI. MRIs of the brain and cervical spine were able to be interpreted, but MRIs of the thoracolumbar spine could not be interpreted because of MCGR artifact. MRIs can be safely performed in patients with MCGRs; however, MRIs of thoracic and thoracolumbar spine may be of limited clinical benefit because of artifact.
Level of Evidence
Level IV, case series.
Similar content being viewed by others
References
Thompson W, Thakar C, Rolton D, et al. The use of magneticallycontrolled growing rods to treat children with early-onset scoliosis. Bone Joint J 2016;98:1240–7.
Choi E, Yazsay B, Mundis G, et al. Implant complications after magnetically controlled growing rods for early onset scoliosis: a multicenter retrospective review. J Pediatr Orthop 2017;37: e588–92.
Ridderbusch K, Rupprecht M, Kunkel P, et al. Preliminary results of magnetically controlled growing rods for early onset scoliosis. J Pediatr Orthop 2017;37:e575–80.
Charroin C, Abelin-Genevois K, Cunin V, et al. Direct costs associated with the management of progressive early onset scoliosis: estimations based on gold standard technique or with magnetically controlled growing rods. Orthop Traumatol Surg Res 2014; 100: 469–74.
Rolton D, Richards J, Nnadi C. Magnetic controlled growth rods versus conventional growing rod systems in the treatment of early onset scoliosis: a cost comparison. Eur Spine J 2015;24: 1457–61.
Akbarnia BA, Pawelek JB, Cheung KM, et al. Traditional growing rods versus magnetically controlled growing rods for the surgical treatment of early-onset scoliosis: a case-matched 2-year study. Spine Deform 2014;2:493–7.
Jayaswal A, Kandwal P, Goswami A, et al. Early onset scoliosis with intraspinal anomalies: management with growing rod. Eur Spine J 2016;25:3301–7.
McMaster MJ. Occult intraspinal anomalies and congenital scoliosis. J Bone Joint Surg Am 1984;66:588–601.
Bradford DS, Heithoff KB, Cohen M. Intraspinal abnormalities and congenital spine deformities: a radiographic and MRI study. J Pediatr Orthop 1991;11:36–41.
Basu PS, Elsebaie H, Noordeen MH. Congenital spinal deformity: a comprehensive assessment at presentation. Spine 2002;27: 2255–9.
Shen J, Wang Z, Liu J, et al. Abnormalities associated with congenital scoliosis: a retrospective study of 226 Chinese surgical cases. Spine 2013;38:814–8.
Budd HR, Stokes OM, Meakin J, et al. Safety and compatibility of magnetic-controlled growing rods and magnetic resonance imaging. Eur Spine J 2016;25:578–82.
Poon S, Graver A, Wendolowski S, et al. A pilot cadaveric study of the safety and efficacy of magnetic-controlled growing rods after exposure to magnetic resonance imaging. Presented at American Academy of Pediatrics National Conference 2016.
Nurre A. NuVasive Secures Magnetic Resonance (MR) FDA Conditional Clearance for MAGEC System. 2016. Available at: https://www.nuvasive.com/nuvasive-secures-magnetic-resonance-mr-fda-conditional-clearance-for-magec-system/. Accessed October 27, 2016.
Hosseini P, Pawelek J, Mundis GM, et al. Magnetically controlled growing rods for early-onset scoliosis: a multicenter study of 23 cases with minimum 2 years follow-up. Spine 2016;41:1456–62.
Poon S, Nixon R, Wendolowski S, et al. A pilot cadaveric study of temperature and adjacent tissue changes after exposure of magnetic-controlled growing rods to MRI. Eur Spine J 2017;26: 1618–23.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Author disclosures: RPW (none); LMA (personal fees from Biomet; Medtronic, other from Eli Lilly, other from Orthobullets, other from Journal of Pediatric Orthopaedics, other from Pediatric Orthopaedic Society of North America and the Scoliosis Research Society, outside the submitted work); HN (personal fees from BAXTER, personal fees from K2M, personal fees from ELLIPSE TECHNOLOGIES, personal fees from KSPINE, non-financial support from Spine, non-financial support from Spine Deformity, personal fees from Stryker, outside the submitted work); SM (none); JH (none); SAS (grants from Setting Scoliosis Straight Foundation, personal fees from DePuy Synthes Spine, personal fees from NuVasive, outside the submitted work); JP (other from San Diego Spine Foundation, outside the submitted work); CEJ (other from Medtronic, other from Elsevier, outside the submitted work); DLS (other from Growing Spine Study Group; Scoliosis Research Society; Growing Spine Foundation, personal fees from ZimmerBiomet; Medtronic; Zipline Medical, Inc.; Orthobullets; Grand Rounds [a healthcare navigation company], Greensunmedical, grants from Pediatric Orthopaedic Society of North America & Scoliosis Research Society, Paid to Columbia University; Elipse [co–principal investigator, paid to GSF], other from Zipline Medical, Inc. Green Sun Medical, Orthobullets, personal fees from ZimmerBiomet; Medtronic; Johnson & Johnson, other from Medtronic & ZimmerBiomet, non-financial support from Wolters Kluwer Health - Lippincott Williams & Wilkins; Biomet Spine, other from Orthobullets, Co-Editor in Chief, outside the submitted work); Children’s Spine Study Group (none); Growing Spine Study Group (grants from Nuvasive, grants from Growing Spine Foundation, grants from US Food and Drug Administration, during the conduct of the study; and the Growing Spine Foundation financially supports the Growing Spine Study Group which provided the research data for this study. The GSF receives donations from the study group’s surgeon members, medical device industry, grateful patients and other donors).
This study has been carried out with approval from the Committee on Clinical Investigations at Children’s Hospital Los Angeles.
Rights and permissions
About this article
Cite this article
Woon, R.P., Andras, L.M., Noordeen, H. et al. Surgeon Survey Shows No Adverse Events With MRI in Patients With Magnetically Controlled Growing Rods (MCGRs). Spine Deform 6, 299–302 (2018). https://doi.org/10.1016/j.jspd.2017.10.004
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2017.10.004