Abstract
Introduction
Recent healthcare reforms have raised the importance of cost and value in the management of disease. Value is a function of benefit and cost. Understanding variability in resources utilized by individual surgeons to achieve similar outcomes may provide an opportunity for cutting costs though greater standardization. The purpose of this study is to evaluate differences in use of implants and hospital resources among surgeons performing adolescent idiopathic scoliosis (AIS) surgery.
Methods
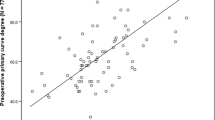
A multicenter prospective AIS operative database was queried. Patients were matched for Lenke curve type and curve magnitude, resulting in 5 surgeons and 35 matched groups (N = 175). Mean patient age was 14.9 years and curve magnitude 50°. Parameters of interest were compared between surgeons via ANOVA and Bonferroni pairwise comparison.
Results
There was no significant difference in percentage curve correction or levels fused between surgeons. Significant differences between surgeons were found for percentage posterior approach, operative time, length of stay (LOS), estimated blood loss (EBL), cell saver transfused, rod material, screw density, number of screws, use of antifibrinolytics, and cessation of intravenous analgesics. Despite differences in EBL and cell saver transfused, there were no differences in allogenic blood (blood bank) use.
Conclusion
Significant variability in resource utilization was noted between surgeons performing AIS operations, although radiographic results were uniform. Standardization of resource utilization and cost containment opportunities include implant usage, rod material, LOS, and transition to oral analgesics, as these factors are the largest contributors to cost in AIS surgery.
Similar content being viewed by others
References
Kepler CK, Wilkinson SM, Radcliff KE, et al. Cost-utility analysis in spine care: a systematic review. Spine J 2012;12:676–90.
Al-Khouja LT, Baron EM, Johnson JP, et al. Cost-effectiveness analysis in minimally invasive spine surgery. Neurosurg Focus 2014;36:E4.
Walid MS, Robinson Jr JS. Economic impact of comorbidities in spine surgery: clinical article. J Neurosurg Spine 2011;14:318–21.
Glassman SD, Polly DW, Dimar JR, Carreon LY. The cost effectiveness of single-level instrumented posterolateral lumbar fusion at 5 years after surgery. Spine 2012;37:769–74.
Carreon LY, Anderson PA, Traynelis VC, et al. Cost-effectiveness of single-level anterior cervical discectomy and fusion five years after surgery. Spine 2013;38:471–5.
Sanders JO, Haynes R, Lighter D, et al. Variation in care among spinal deformity surgeons: results of a survey of the Shriners hospitals for children. Spine 2007;32:1444–9.
Kamerlink JR, Quirno M, Auerbach JD, et al. Hospital cost analysis of adolescent idiopathic scoliosis correction surgery in 125 consecutive cases. J Bone Joint Surg 2010;92:1097–104.
Chu T, Chandhoke RA, Smith PC, Schwaitzberg SD. The impact of surgeon choice on the cost of performing laparoscopic appendectomy. Surg Endosc 2010;25:1187–91.
Kassin MT, Owen RM, Perez SD, et al. Risk factors for 30-day hospital readmission among general surgery patients. J Am Coll Surg 2012;215:322–30.
Rowe CK, Pierce MW, Tecci KC, et al. A comparative direct cost analysis of pediatric urologic robot-assisted laparoscopic surgery versus open surgery: could robot-assisted surgery be less expensive? J Endourol 2012;26:871–7.
Wick EC, Shore AD, Hirose K, et al. Readmission rates and cost following colorectal surgery. Dis Colon Rectum 2011;54:1475–9.
Miller DC, Gust C, Dimick JB, et al. Large variations in Medicare payments for surgery highlight savings potential from bundled payment programs. Health Aff 2011;30:2107–15.
Cutler DM, Ghosh K. The potential for cost savings through bundled episode payments. N Engl J Med 2012;366:1075–7.
Bozic KJ, Ward L, Vail TP, Maze M. Bundled payments in total joint arthroplasty: targeting opportunities for quality improvement and cost reduction. Clin Orthop Relat Res 2014;472:188–93.
Birkmeyer JD, Sharp SM, Finlayson SR, et al. Variation profiles of common surgical procedures. Surgery 1998;124:917–23.
Larson AN, Polly Jr DW, Ackerman SJ, et al. What would be the annual cost savings if fewer screws were used in adolescent idiopathic scoliosis treatment in the US? J Neurosurg Spine 2016;24:116–23.
Bharucha NJ, Lonner BS, Auerbach JD, et al. Low-density versus high-density thoracic pedicle screw constructs in adolescent idiopathic scoliosis: do more screws lead to a better outcome? Spine J 2013;13:375–81.
Epstein NE, Schwall G, Reillly T, et al. Surgeon choices, and the choice of surgeons, affect total hospital charges for single-level anterior cervical surgery. Spine 2011;36:905–9.
Larson AN, Aubin CE, Polly DW, et al. Minimize Implants Maximize Outcomes Study Group. Are more screws better? A systematic review of anchor density and curve correction in adolescent idiopathic scoliosis. Spine Deform 2013;1:237–47.
Roach JW, Mehlman CT, Sanders JO. Does the outcome of adolescent idiopathic scoliosis surgery justify the rising cost of the procedures? J Pediatr Orthop 2011;31:S77–80.
Lonner BS, Auerbach JD, Levin R, et al. Thoracoscopic anterior instrumented fusion for adolescent idiopathic scoliosis with emphasis on the sagittal plane. Spine J 2009;9:523–9.
Arlet V. Anterior thoracoscopic spine release in deformity surgery: a meta-analysis and review. Eur Spine J 2000;9:S017–23.
Newton PO, Upasani VV, Lhamby J, et al. Surgical treatment of main thoracic scoliosis with thoracoscopic anterior instrumentation. J Bone Joint Surg 2008;90:2077–89.
Lonner BS, Lazar-Antman MA, Sponseller PD, et al. Multivariate analysis of factors associated with kyphosis maintenance in adolescent idiopathic scoliosis. Spine 2012;37:1297–302.
Lonner BS, Auerbach JD, Estreicher M, et al. Video-assisted thoracoscopic spinal fusion compared with posterior spinal fusion with thoracic pedicle screws for thoracic adolescent idiopathic scoliosis. J Bone Joint Surg 2009;91:398–408.
Lonner BS, Kondrachov D, Siddiqi F, et al. Thoracoscopic spinal fusion compared with posterior spinal fusion for the treatment of thoracic adolescent idiopathic scoliosis. J Bone Joint Surg Am 2006;88:1022–34.
Lowenstein JE, Matsumoto H, Vitale MG, et al. Coronal and sagittal plane correction in adolescent idiopathic scoliosis: a comparison between all pedicle screw versus hybrid thoracic hook lumbar screw constructs. Spine 2007;32:448–52.
Kim YJ, Lenke LG, Kim J, et al. Comparative analysis of pedicle screw versus hybrid instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine 2006;31:291–8.
Di Silvestre M, Bakaloudis G, Lolli F, et al. Posterior fusion only for thoracic adolescent idiopathic scoliosis of more than 80: pedicle screws versus hybrid instrumentation. Eur Spine J 2008;17:1336–49.
Liljenqvist U, Lepsien U, Hackenberg L, et al. Comparative analysis of pedicle screw and hook instrumentation in posterior correction and fusion of idiopathic thoracic scoliosis. Eur Spine J 2002;11:336–43.
Yilmaz G, Borkhuu B, Dhawale AA, et al. Comparative analysis of hook, hybrid, and pedicle screw instrumentation in the posterior treatment of adolescent idiopathic scoliosis. J Pediatr Orthop 2012;32:490–9.
Dalal A, Upasani VV, Bastrom TP, et al. Apical vertebral rotation in adolescent idiopathic scoliosis: comparison of uniplanar and polyaxial pedicle screws. J Spinal Disord Tech 2011;24:251–7.
Shah SA, Dhawale AA, Oda JE, et al. Ponte osteotomies with pedicle screw instrumentation in the treatment of adolescent idiopathic scoliosis. Spine Deform 2013;1:196–204.
Monazzam S, Newton PO, Bastrom TP, Yaszay B. Harms Study Group. Multicenter comparison of the factors important in restoring thoracic kyphosis during posterior instrumentation for adolescent idiopathic scoliosis. Spine Deform 2013;1:359–64.
Holland DE, Hemann MA. Standardizing hospital discharge planning at the Mayo Clinic. Jt Comm J Qual Patient Saf 2011;37:29–36.
Ortiga B, Salazar A, Jovell A, et al. Standardizing admission and discharge processes to improve patient flow: a cross sectional study BMC Health Serv Res 2012;12:180.
Zheng F, Cammisa Jr FP, Sandhu HS, et al. Factors predicting hospital stay, operative time, blood loss, and transfusion in patients undergoing revision posterior lumbar spine decompression, fusion, and segmental instrumentation. Spine 2002;27:818–24.
Gora-Harper ML, Record KE, Darkow T, Tibbs PA. Opioid analgesics versus ketorolac in spine and joint procedures: impact on healthcare resources. Ann Pharmacother 2001;35:1320–6.
Neilipovitz DT, Murto K, Hall L, et al. A randomized trial of tranexamic acid to reduce blood transfusion for scoliosis surgery. Anesth Analg 2001;93:82–7.
Sethna NF, Zurakowski D, Brustowicz RM, et al. Tranexamic acid reduces intraoperative blood loss in pediatric patients undergoing scoliosis surgery. Anesthesiology 2005;102:727–32.
Tzortzopoulou A, Cepeda MS, Schumann R, Carr DB. Antifibrinolytic agents for reducing blood loss in scoliosis surgery in children. Cochrane Database Syst Rev 2008;3:CD006883.
Verma K, Errico TJ, Vaz KM, Lonner BS. A prospective, randomized, double-blinded single-site control study comparing blood loss prevention of tranexamic acid (TXA) to epsilon aminocaproic acid (EACA) for corrective spinal surgery. BMC Surg 2010;10:13.
Verma K, Errico T, Diefenbach C, et al. The relative efficacy of antifibrinolytics in adolescent idiopathic scoliosis. J Bone Joint Surg 2014;96:e80.
Nuttall GA, Horlocker TT, Santrach PJ, et al. Predictors of blood transfusions in spinal instrumentation and fusion surgery. Spine 2000;25:596–601.
Shapiro F, Sethna N. Blood loss in pediatric spine surgery. Eur Spine J 2004;13:S6–17.
Auerbach JD, Lonner BS, Antonacci MD, Kean KE. Perioperative outcomes and complications related to teaching residents and fellows in scoliosis surgery. Spine 2008;33:1113–8.
Hoashi JS, Samdani AF, Betz RR, et al. Is there a “July effect” in surgery for adolescent idiopathic scoliosis? J Bone Joint Surg 2014;96:e55.
Lehman RA, Shufflebarger HL, Marks MC, et al. Three-year dashboard reporting and Performance Improvement Modules (PIMs) significantly improved blood loss and operative time in adolescent idiopathic scoliosis. Paper presented at: Scoliosis Research Society (SRS) 50th Annual Meeting and Course; September 30-October 3, 2015; Minneapolis, Minnesota. Paper 31.
Miyanji F, Slobogean GP, Samdani AF, et al. Is larger scoliosis curve magnitude associated with increased perioperative healthcare resource utilization? J Bone Joint Surg 2012;94:809–13.
Ho DM, Huo MH. Are critical pathways and implant standardization programs effective in reducing costs in total knee replacement operations? J Am Coll Surg 2007;205:97–100.
Penn E, Yasso SF, Wei JL. Reducing disposable equipment waste for tonsillectomy and adenotonsillectomy cases. Otolaryngol Head Neck Surg 2012;147:615–8.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author disclosures
BSL (grants from Setting Scoliosis Straight Foundation, during the conduct of the study; grants from Setting Scoliosis Straight Foundation; personal fees from DePuy Synthes Spine, K2M, Paradigm Spine, Spine Search, and Ethicon; nonfinancial support from Spine Deformity Journal; grants from AO Spine, John and Marcella Fox Fund Grant, and OREF, outside the submitted work); CST (none); JCP (none); SAS (reports grants from Setting Scoliosis Straight Foundation, during the conduct of the study; grants from Setting Scoliosis Straight Foundation; personal fees from DePuy Synthes Spine, outside the submitted work); HLS (none); JMF (reports other from Biomet, other from LWW, outside the submitted work); PON (reports grants from Setting Scoliosis Straight Foundation, during the conduct of the study; grants and other from Setting Scoliosis Straight Foundation, other from Rady Children’s Specialists, grants and personal fees from DePuy Synthes Spine, personal fees from Law firm of Carroll, Kelly, Trotter, Franzen & McKenna, and the Law firm of Smith, Haughey, Rice & Roegge; grants from NIH and OREF, grants and other from SRS; grants from EOS imaging; personal fees from Thieme Publishing; other from NuVasive; personal fees from Ethicon Endosurgery; other from Electrocore; personal fees from Cubist; other from International Orthopedic Think Tank; other from Orthopediatrics Institutional Support, and personal fees from K2M, outside the submitted work; in addition, PON has a patent “Anchoring systems and methods for correcting spinal deformities” (8540754) with royalties paid to DePuy Synthes Spine, a patent “Low profile spinal tethering systems” (8123749) issued to DePuy Spine, Inc.; a patent “Screw placement guide” (7981117) issued to DePuy Spine, Inc.; and a patent “Compressor for use in minimally invasive surgery” (7189244) issued to DePuy Spine, Inc.).
Rights and permissions
About this article
Cite this article
Lonner, B.S., Toombs, C.S., Paul, J.C. et al. Resource Utilization in Adolescent Idiopathic Scoliosis Surgery: Is There Opportunity for Standardization?. Spine Deform 5, 166–171 (2017). https://doi.org/10.1016/j.jspd.2017.01.002
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2017.01.002