Abstract
Study Design
Retrospective clinical and radiographic review.
Objective
The purpose of this study was to evaluate the characteristics of deep wound infection, as well as the potential factors that correlate to surgical site infection (SSI) in spine deformity surgery.
Summary of Background Data
Preventing SSIs in pediatric spinal deformity surgery is a crucial task. Recent data have shown that antibiotic-loaded allograft and properly timed preoperative antibiotic administration decrease SSIs. However, there remain controversies over the appropriate preoperative antibiotic selection.
Methods
We reviewed 851 spinal deformity surgeries that took place at a single institution from 2006 to 2010. In particular, preoperative and postoperative characteristics of the deep wound infections were evaluated.
Results
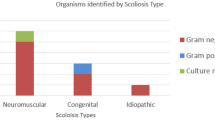
Twenty-four patients had SSIs. The mean age at surgery in the infected cohort was 14 years, mean length of surgery was 8 hours, and median estimated blood loss was 2,482 mL (%EBV: 66%). Approximately 67% of the infected patients had bowel/bladder incontinence, and 71% had prolonged intravenous access perioperatively. According to culture results, the most effective antibiotic to treat the infections was vancomycin. Preoperative antibiotics were administered within 30 minutes of incision (hospital protocol) in only 12.5% (p =.001) and within 1 hour of incision in 54% of the cases. The wound status within 3 days of surgery is as follows: 38% intact, 29% significant wound drainage, and 33% wound dehiscence. Methicillin-resistant Staphylococcus aureus (MRSA) and oxacillin-resistant Staphylococcus epidermidis were associated with intact wounds, whereas gram-negative pathogens were seen in dehisced or draining wounds (p <.001).
Conclusions
The authors showed that their cohort of patients with infection had a high rate of draining wounds, MRSA infections, administration of antibiotics more than 1 hour ahead of incision, and prolonged need for intravenous access after surgery. Efforts to mitigate these associations by using vancomycin prophylactically, doing meticulous wound closure to prevent drainage or dehiscence, and delivering antibiotics at an optimal time ahead of incision may lead to a decrease in infection rates in pediatric spinal surgery. Future prospective studies will be needed to validate this. © 2015 Scoliosis Research Society.
Similar content being viewed by others
References
Massie JB, Heller JG, Abitbol JJ, et al. Postoperative posterior spinal wound infections. Clin Orthop Relat Res 1992;284: 99e108.
Dietz FR, Koontz FP, Found EM, Marsh JL. The importance of positive bacterial cultures of specimens obtained during clean orthopaedic operations. J Bone Joint Surg Am 1991;73: 1200e7.
Sasso RC, Garrido BJ. Postoperative spinal wound infections. J Am Acad Orthop Surg 2008;16: 330e7.
Casanova JF, Herruzo R, Diez J. Risk factors for surgical site infection in children. Infect Control Hosp Epidemiol 2006;27: 709e15.
Bucher BT, Warner BW, Dillon PA. Antibiotic prophylaxis and the prevention of surgical site infection. Curr Opin Pediatr 2011;23: 334e8.
Pull ter Gunne AF, Mohamed AS, Skolasky RL, et al. The presentation, incidence, etiology, and treatment of surgical site infections after spinal surgery. Spine (Phila Pa 1976) 2010;35: 1323e8.
Krizek TJ, Robson MC. Evolution of quantitative bacteriology in wound management. Am J Surg 1975;130: 579e84.
Noble WC. The production of subcutaneous staphylococcal skin lesions in mice. Br J Exp Pathol 1965;46: 254e62.
Elek SD, Conen PE. The virulence of Staphylococcus pyogenes for man; a study of the problems of wound infection. Br J Exp Pathol 1957;38: 573e86.
James RC, Macleod CJ. Induction of staphylococcal infections in mice with small inocula introduced on sutures. Br J Exp Pathol 1961;42: 266e77.
Mangram AJ, Horan TC, Pearson ML, et al. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol 1999;20: 250e78. quiz 279e80.
Moe JH. Complications of scoliosis treatment. Clin Orthop Relat Res 1967;53: 21e30.
Klein JD, Garfin SR. Nutritional status in the patient with spinal infection. Orthop Clin North Am 1996;27: 33e6.
Esses SI, Sachs BL, Dreyzin V. Complications associated with the technique of pedicle screw fixation. A selected survey of ABS members. Spine (Phila Pa 1976) 1993;18: 2231e8; discussion 2238e9.
Hodges SD, Humphreys SC, Eck JC, et al. Low postoperative infection rates with instrumented lumbar fusion. South Med J 1998;91: 1132e6.
Arens S, Schlegel U, Printzen G, et al. Influence of materials for fixation implants on local infection. An experimental study of steel versus titanium DCP in rabbits. J Bone Joint Surg Br 1996;78: 647e51.
Fry DE, Fry RV, Borzotta AP. Nosocomial blood-borne infection secondary to intravascular devices. Am J Surg 1994;167: 268e72.
Centers for Disease Control and Prevention. National Nosocomial Infections Surveillance (NNIS) report, data summary from October 1986-April 1996. A report from the National Nosocomial Infections Surveillance (NNIS) system. Am J Infect Control 1996;24: 380e8.
Nooyen SM, Overbeek BP, Brutel de la Riviere A, et al. Prospective randomised comparison of single-dose versus multiple-dose cefuroxime for prophylaxis in coronary artery bypass grafting. Eur J Clin Microbiol Infect Dis 1994;13:1033–7.
Weigelt JA, Lipsky BA, Tabak YP, et al. Surgical site infections: causative pathogens and associated outcomes. Am J Infect Control 2010;38: 112e20.
Jernigan JA. Is the burden of Staphylococcus aureus among patients with surgical-site infections growing? Infect Control Hosp Epidemiol 2004;25: 457e60.
Kim DH, Spencer M, Davidson SM, et al. Institutional prescreening for detection and eradication of methicillin-resistant Staphylococcus aureus in patients undergoing elective orthopaedic surgery. J Bone Joint Surg Am 2010;92: 1820e6.
Page CP, Bohnen JM, Fletcher JR, et al. Antimicrobial prophylaxis for surgical wounds. Guidelines for clinical care. Arch Surg 1993;128: 79e88.
Bratzler DW, Hunt DR. The surgical infection prevention and surgical care improvement projects: national initiatives to improve outcomes for patients having surgery. Clin Infect Dis 2006;43: 322e30.
Dellinger EP, Gross PA, Barrett TL, et al. Quality standard for antimicrobial prophylaxis in surgical procedures. Infectious Diseases Society of America. Clin Infect Dis 1994;18: 422e7.
ASHP Therapeutic Guidelines on Antimicrobial Prophylaxis in Surgery. American Society of Health-System Pharmacists. Am J Health Syst Pharm 1999;56: 1839e88.
Classen DC, Evans RS, Pestotnik SL, et al. The timing of prophylactic administration of antibiotics and the risk of surgical-wound infection. N Engl J Med 1992;326: 281e6.
Milstone AM, Maragakis LL, Townsend T, et al. Timing of preoper-ative antibiotic prophylaxis: a modifiable risk factor for deep surgical site infections after pediatric spinal fusion. Pediatr Infect Dis J 2008;27: 704e8.
Steinberg JP, Braun BI, Hellinger WC, et al. Timing of antimicrobial prophylaxis and the risk of surgical site infections: results from the Trial to Reduce Antimicrobial Prophylaxis Errors. Ann Surg 2009;250: 10e6.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author disclosures: None declared for authors SP (none); FM (none); SD (none); LH (none); KD (personal fees from DePuy Spine); SAS (patent filed for DePuy Synthes Spine, Inc.).
Rights and permissions
About this article
Cite this article
Pourtaheri, S., Miller, F., Dabney, K. et al. Deep Wound Infections After Pediatric Scoliosis Surgery. Spine Deform 3, 533–540 (2015). https://doi.org/10.1016/j.jspd.2015.04.003
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2015.04.003