Abstract
Study Design
Retrospective case-control study.
Objectives
To identify risk factors for early deep surgical site infections (SSIs; within three months of index procedure) following pediatric spinal deformity surgery.
Background
Deep surgical site infections (SSIs) following pediatric spinal deformity surgery are a source of significant morbidity. We sought to identify independent risk factors for early infection following primary, definitive single-stage pediatric posterior spinal fusion and instrumentation (PSFI).
Methods
A total of 616 consecutive patients (2001–2016) from an institutional prospectively maintained Pediatric Orthopaedic Spine database were identified that met inclusion criteria of definitive single-stage PSFI. Early deep SSI was defined as infection within three months of index procedure requiring surgical intervention. A multivariate analysis of demographics, comorbidities, and perioperative factors was performed and independent risk factors were identified.
Results
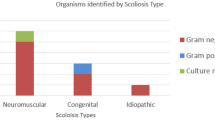
Eleven patients (1.6%) developed an early deep SSI. Independent risk factors for SSI identified were nonidiopathic (neuromuscular, syndromic, and congenital) etiologies of scoliosis (adjusted odds ratio [aOR]: 8.384, 95% confidence interval [CI]: 1.784–39.386, p = .007) and amount of intraoperative crystalloids (aOR: 1.547 per additional liter of fluid, 95% CI: 1.057–2.263, p = .025). Mean crystalloid administered in the SSI group was 3.3 ± 1.2 L versus 2.4 ± 1.0 L in the noninfected group (p = .019). On univariate analysis, there was no significant difference in weight of patients between cohorts (p = .869) or surgery time (p = .089). There was also no significant difference in infection rates from redosing of antibiotics intraoperatively after 3 hours of surgery (p = .231).
Conclusions
Nonidiopathic scoliosis and amount of intraoperative crystalloids were independently associated with early postoperative SSI. Further investigation into intraoperative fluid management may identify modifiable risk factors for early postoperative SSI in primary pediatric spinal deformity posterior spinal fusion patients.
Level of Evidence
Level III, case-control study.
Similar content being viewed by others
References
Cahill PJ, Warnick DE, Lee MJ, et al. Infection after spinal fusion for pediatric spinal deformity: thirty years of experience at a single institution. Spine (Phila Pa 1976) 2010;35:1211–7.
Kabirian N, Akbarnia BA, Pawelek JB, et al. Deep surgical site infection following 2344 growing-rod procedures for early-onset scoliosis: risk factors and clinical consequences. J Bone Joint Surg Am 2014;96:e128.
Jain A, Puvanesarajah V, Menga EN, Sponseller PD. Unplanned hospital readmissions and reoperations after pediatric spinal fusion surgery. Spine (Phila Pa 1976) 2015;40:856–62.
Patient Protection and Affordable Care Act, HR 3590. 111th Cong (2009–2010). Available at: https://www.gpo.gov/fdsys/pkg/BILLS-111hr3590enr/pdf/BILLS-111hr3590enr.pdf. Accessed October 22, 2016.
Axon RN, Williams MV. Hospital readmission as an accountability measure. JAMA 2011;305:504–5.
Subramanyam R, Schaffzin J, Cudilo EM, et al. Systematic review of risk factors for surgical site infection in pediatric scoliosis surgery. Spine J 2015;15:1422–31.
Croft LD, Pottinger JM, Chiang HY, et al. Risk factors for surgical site infections after pediatric spine operations. Spine (Phila Pa 1976) 2015;40:E112–9.
Mistovich RJ, Jacobs LJ, Campbell RM, et al. Infection control in pediatric spinal deformity surgery: a systematic and critical analysis review. JBJS Rev 2017;5:e3.
Glotzbecker MP, Riedel MD, Vitale MG, et al. What’s the evidence? Systematic literature review of risk factors and preventive strategies for surgical site infection following pediatric spine surgery. J Pediatr Orthop 2013;33:479–87.
Centers for Disease Control and Prevention. Surgical site infection event. Available at: http://www.cdc.gov/nhsn/PDFs/pscManual/9pscSSIcurrent.pdf. Accessed November 13, 2016.
Lentner, C, ed. Geigy Scientific Tables. 7th ed. Basel: Ciba-Geigy, 1970.
Reames DL, Smith JS, Fu KM, et al. Complications in the surgical treatment of 19,360 cases of pediatric scoliosis: a review of the Scoliosis Research Society Morbidity and Mortality database. Spine (Phila Pa 1976) 2011;36:1484–91.
Sponseller PD, Shah SA, Abel MF, et al. Infection rate after spine surgery in cerebral palsy is high and impairs results: multicenter analysis of risk factors and treatment. Clin Orthop Relat Res 2010;468: 711–6.
Sponseller PD, Jain A, Shah SA, et al. Deep wound infections after spinal fusion in children with cerebral palsy: a prospective cohort study. Spine (Phila Pa 1976) 2013;38:2023–7.
Sponseller PD, LaPorte DM, Hungerford MW, et al. Deep wound infections after neuromuscular scoliosis surgery: a multicenter study of risk factors and treatment outcomes. Spine (Phila Pa 1976) 2000;25: 2461–6.
Chappell D, Jacob M, Hofmann-Kiefer K, et al. A rational approach to perioperative fluid management. Anesthesiology 2008; 109: 723–40.
Inanmaz ME, Kose KC, Isik C, et al. Can hyperbaric oxygen be used to prevent deep infections in neuro-muscular scoliosis surgery? BMC Surg 2014;14:85.
Greif R, Akça O, Horn EP, et al. Supplemental perioperative oxygen to reduce the incidence of surgical-wound infection. N Engl J Med 2000;342:161–7.
Holte K, Kristensen BB, Valentiner L, et al. Liberal versus restrictive fluid management in knee arthroplasty: a randomized, double-blind study. Anesth Analg 2007;105:465–74.
Bennett-Guerrero E, Feierman DE, Barclay GR, et al. Preoperative and intraoperative predictors of postoperative morbidity, poor graft function, and early rejection in 190 patients undergoing liver transplantation. Arch Surg 2001;136:1177–83.
Møller AM, Pedersen T, Svendsen PE, Engquist A. Perioperative risk factors in elective pneumonectomy: the impact of excess fluid balance. Eur J Anaesthesiol 2002;19:57–62.
Brandstrup B, Tønnesen H, Beier-Holgersen R, et al. Effects of intravenous fluid restriction on postoperative complications: comparison of two perioperative fluid regimens: a randomized assessor-blinded multicenter trial. Ann Surg 2003;238:641–8.
Di Silvestre M, Bakaloudis G, Lolli F, Giacomini S. Late-developing infection following posterior fusion for adolescent idiopathic scoliosis. Eur Spine J 2011;20(suppl 1):S121–7.
Soultanis KC, Pyrovolou N, Zahos KA. Late postoperative infection following spinal instrumentation: stainless steel versus titanium implants. J Surg Orthop Adv 2008;17:193–9.
Ramo BA, Roberts DW, Tuason D, et al. Surgical site infections after posterior spinal fusion for neuromuscular scoliosis: a thirty-year experience at a single institution. J Bone Joint Surg Am 2014;96: 2038–48.
Devin CJ, Chotai S, McGirt MJ, et al. Intrawound vancomycin decreases the risk of surgical site infection after posterior spine surgery—a multicenter analysis. Spine (Phila Pa 1976) 2018;43: 65–71.
Salsgiver E, Crotty J, LaRussa SJ, et al. Surgical site infections following spine surgery for non-idiopathic scoliosis. J Pediatr Orthop 2017;37:e476–83.
Garg S, Cyr M, St Hilaire T, et al. Variability of surgical site infection with VEPTR at eight centers: a retrospective cohort analysis. Spine Deform 2016;4:59–64.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author disclosures: JYD (none), CPK (none), GHT (personal fees from Wolters Kluwer; personal fees and other from OrthoPediatrics and Shriner’s Hospital for Children, other from Scoliosis Research Society and NuVasive; from SpineForm [nonpaid consultant], outside the submitted work), JPSH (other from OrthoPediatrics, outside the submitted work), CKH (personal fees from Medtronic, Inc., and OrthoPediatrics, outside the submitted work), RJM (other from Right Mechanics, Inc., and OrthoPediatrics, outside the submitted work).
IRB Approval: This study was approved by the Rainbow Babies & Children’s Hospitals/University Hospitals Cleveland Medical Center institutional review board.
Rights and permissions
About this article
Cite this article
Du, J.Y., Poe-Kochert, C., Thompson, G.H. et al. Risk Factors for Early Infection in Pediatric Spinal Deformity Surgery: A Multivariate Analysis. Spine Deform 7, 410–416 (2019). https://doi.org/10.1016/j.jspd.2018.09.011
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2018.09.011