Abstract
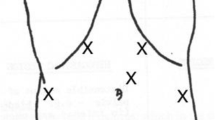
Laparoscopic Heller myotomy (LHM) has become the standard treatment option for achalasia. The incidence of esophageal perforation reported is about 5%–10%. Robotically assisted Heller myotomy (RAHM) is emerging as a safe alternative to LHM. Data comparing the two approaches are scant. The aim of this study was to compare RAHM with LHM in terms of efficacy and safety for treatment of achalasia. A total of 121 patients underwent surgical treatment of achalasia at three institutions. A retrospective review of prospectively collected perioperative data was performed. Patients were divided into two groups: group A (RAHM), 59 patients, and group B (LHM), 62 patients. All the operations were completed using minimally invasive techniques. There were 63 women and 58 men, with a mean age of 45 ±19 years (14–82 years). Fifty-one percent of patients in group A and 95% of patients in group B reported weight loss. Duration of symptoms was equal for both groups. Dysphagia was the main complaint in both groups (P = NS). There was no difference in preoperative endoscopic treatment in both groups (44% versus 27%, P = NS). Operative time was significantly shorter for LHM in the first half of the experience (141 ± 49 versus 122 ± 44 minutes, P < .05). However, in the last 30 cases there was no difference in operative time between the groups (P = NS). Intraoperative complications (esophageal perforation) were more frequent in group B (16% versus 0%). The incidence of postoperative heartburn did not differ by group. There were no deaths. At 18 and 22 months, 92% and 90% of patients had relief of their dysphagia. This study suggests that RAHM is safer than LHM, because it decreases the incidence of esophageal perforation to 0%, even in patients who had previous treatment. At short-term follow-up, relief of dysphagia was equally achieved in both groups.
Similar content being viewed by others
References
Brewer 3rd LA. History of surgery of the esophagus. Am J Surg 1980;139:730–743.
Pellegrini C, Wetter LA, Patti M, et al. Thoracoscopic esophagomyotomy. Initial experience with a new approach for the treatment of achalasia. Ann Surg 1992;216:291–296; discussion 296–299.
Shimi S, Nathanson LK, Cuschieri A. Laparoscopic cardiomyotomy for achalasia. J R Coll Surg Edinb 1991;36:152–154.
Melvin WS, Needleman BJ, Krause KR, Schneider C, Ellison EC. Computer-enhanced vs. standard laparoscopic antireflux surgery. J Gastrointest Surg 2002;6:11–15; discussion 15–6.
Moonka R, Patti MG, Feo CV, et al. Malignant pseudoachalasia. Surg Endosc 1999;13:273–275.
Chaer RA, Jacobsen G, Elli F, Harris J, Goldstein A, Horgan S. Robotic-assisted laparoscopic pediatric Heller’s cardiomyotomy: initial case report. J Laparoendosc Adv Surg Tech A 2004;14:270–273.
Donahue PE, Horgan S, Liu KJ, Madura JA. Floppy Dor fundoplication after esophagocardiomyotomy for achalasia. Surgery 2002;132:716–722; discussion 722–723.
Csendes A, Braghetto I, Burdiles P, Csendes P. Comparison of forceful dilatation and esophagomyotomy in patients with achalasia of the esophagus. Hepatogastroenterology 1991;38:502–505.
Csendes A, Velasco N, Braghetto I, Henriquez A. A prospective randomized study comparing forceful dilatation and esophagomyotomy in patients with achalasia of the esophagus. Gastroenterology 1981;80:789–795.
Patti MG, Pellegrini CA, Horgan S, et al. Minimally invasive surgery for achalasia: an 8-year experience with 168 patients. Ann Surg 1999;230:587–593; discussion 593–594.
Patti MG, Fisichella PM, Perretta S, et al. Impact of minimally invasive surgery on the treatment of esophageal achalasia: a decade of change. J Am Coll Surg 2003;196:698–703; discussion 703–705.
Oelschlager BK, Chang L, Pellegrini CA. Improved outcome after extended gastric myotomy for achalasia. Arch Surg 2003;138:490–495; discussion 495–497.
Horgan S, Hudda K, Eubanks T, McAllister J, Pellegrini CA. Does botulinum toxin injection make esophagomyotomy a more difficult operation? Surg Endosc 1999;13:576–579.
Patti MG, Feo CV, Arcerito M, et al. Effects of previous treatment on results of laparoscopic Heller myotomy for achalasia. Dig Dis Sci 1999;44:2270–2276.
Melvin WS, Dundon JM, Talamini M, Gorodner MV, Galvani C, Horgan S. Computed enhanced telesurgery minimizes esophageal perforation during Heller myotomy. In press.
Chang L, Satava RM, Pellegrini CA, Sinanan MN. Robotic surgery: identifying the learning curve through objective measurement of skill. Surg Endosc 2003;17:1744–1748.
Hunter JG, Trus TL, Branum GD, et al. Laparoscopic Heller myotomy and fundoplication for achalasia. Ann Surg 1997; 225:655–664; discussion 664–665.
Finley RJ, Clifton JC, Stewart KC, et al. Laparoscopic Heller myotomy improves esophageal emptying and the symptoms of achalasia. Arch Surg 2001;136:892–896.
Zaninotto G, Costantini M, Molena D, et al. Minimally invasive surgery for esophageal achalasia. J Laparoendosc Adv Surg Tech A 2001;11:351–359.
Bloomston M, Serafini F, Rosemurgy AS. Videoscopic Heller myotomy as first-line therapy for severe achalasia. Am Surg 2001;67:1105–1109.
Sharp KW, Khaitan L, Scholz S, Holzman MD, Richards WO. 100 Consecutive minimally invasive Heller myotomies: lessons learned. Ann Surg 2002;235:631–638; discussion 638–639.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was supported in part by a grant provided by Intuitive Surgical, Inc. and Ethicon Endo-Surgery, Inc.
Rights and permissions
About this article
Cite this article
Horgan, S., Galvani, C., Gorodner, M.V. et al. Robotic-assisted heller myotomy versus laparoscopic heller myotomy for the treatment of esophageal achalasia: multicenter study. J Gastrointest Surg 9, 1020–1030 (2005). https://doi.org/10.1016/j.gassur.2005.06.026
Issue Date:
DOI: https://doi.org/10.1016/j.gassur.2005.06.026