Abstract
Gastric cancer (GC), a molecularly and phenotypically highly heterogeneous malignancy, is a leading cause of cancer-related deaths. The Cancer Genome Atlas (TCGA) project identifies the microsatellite instability (MSI) subtype of GC, which has garnered increasing attention due to its relatively favorable survival outcome and better response to immune checkpoint inhibitors (ICIs). The occurrence of MSI is closely associated with the defects in mismatch repair system, subsequently leading to the accumulation of mutations in cell genome, particularly in microsatellites. Based on the exclusive features of MSI GC, several detection methods like immunohistology have been developed to determine MSI status clinically, with novel detection methods developing. It is clinically observed that MSI GC tends to have a better response to ICIs treatment while its response to chemotherapy is controversial, necessitating further investigation into the underlying mechanisms. In this review, we systemically summarized the molecular features, detection method, clinico-pathological characteristics and prognosis of MSI GC, offering a comprehensive overview of this unique GC subtype.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Gastric cancer (GC) is the fifth most common type of cancer globally and the fourth-leading cause of cancer-related mortality [1]. Recent data has shown that gastric cancer is a heterogeneous malignant disease characterized by different molecular features and diverse phenotypes. The genomic profiling conducted by The Cancer Genome Atlas (TCGA) proposed a novel classification which classified gastric cancer into four subtypes: Epstein-Barr virus (EBV) positive, microsatellite instability (MSI), genomically stable (GS), and chromosomal instability (CIN) [2]. Among these subtypes, 22% of the untreated GCs were found to be MSI, which is predominantly hypermutated, intestinal-subtype and antrum-located in the stomach. Moreover, this subtype had the best overall prognosis and the lowest frequency of recurrence (22%) of the four subtypes [3].
The molecular feature of MSI GC is identified by the insertion or deletion of nucleotides in the microsatellite regions, which is believed to be a consequence of defects in the mismatch repair (MMR) system [4]. Hence, in clinical scenarios, MSI gastric cancer and dMMR gastric cancer are occasionally equated. Nevertheless, it is imperative to acknowledge that they are not entirely intrinsically synonymous. The MMR system, composed of a series of DNA mismatch repair enzymes, functions as an essential system for the identification and repair of the genetic mismatches generated during DNA replication. Hence expression loss or functional defects occurring in one or more MMR machinery elements can cause deficiency in the complex, and subsequently unsuccessful DNA repair. In December 1997, the American National Cancer Institute sponsored "The International Workshop on Microsatellite Instability and RER Phenotypes in Cancer Detection and Familial Predisposition" to review and standardize the field [5]. They recommended that the genomic instability associated with defective DNA mismatch repair in tumors to be referred to as microsatellite instability (MSI) [5]. A validated panel of five microsatellite markers was recommended to characterize MSI status of tumors based on the number of markers detected as instability. High-frequency MSI (MSI-H) was recognized if two or more of the five microsatellite markers displays instability, while low-frequency MSI (MSI-L) was recognized if only one of the five markers displays instability. Microsatellite stability (MSS) would be the case if none of the five markers exhibit instability. Since the distinction between MSS and MSI-L still remains subtle, clinical researchers tend to classify MSI-L and MSS as one type.
Despite that MSI GC has achieved the best overall prognosis among the four subtypes and tends to have a better response to ICIs, its response to chemotherapy is controversial[6, 7]. It is of great significance to explore the tumorigenesis and development of MSI GC to inspire clinical translations.
Microsatellite and the mismatch repair system
Microsatellite
Microsatellites (MSs), also known as Short Tandem Repeats (STRs) or Simple Sequence Repeats (SSRs), consist of repetitive DNA sequences of 1 to 6 nucleotides [8]. These DNA motifs are widely dispersed throughout the genome, whereas often located in close proximity to the coding region. MSs are highly polymorphic among populations but usually keep stable within individuals [9]. Each MS specific site consists of a central core surrounded by peripheral flanks. The counts of repeating units in the central core determines the specificity of the MS. When DNA polymerase slippage occurs, it triggers a cascade of insertion or deletion of nucleotides, directly leading to replication errors in MSs. Eventually, it generates mismatched DNA strands [4].
The mismatch repair system
The mismatch repair (MMR) system, which comprises several functional proteins, is responsible for the rapid response to errors in replication. It is indispensable for providing an exact coping strategy for the replication errors of MSs. MutS protein homologue 2 (MSH2), MutS protein homologue 3 (MSH3), MutS protein homologue 6 (MSH6), MutL protein homologue 1 (MLH1), post-meiotic segregation increased homologue 1 (PMS1), and PMS1 homologue 2 (PMS2) are the main proteins involved in the MMR system. These proteins interact as heterodimers. MSH2 couples with either MSH3 or MSH6 forming MutS complex, meanwhile MLH1 couples with either PMS2 or MLH3 forming MutL complex [4, 9]. During normal DNA replication, the heterodimeric complexes MSH2/MSH6 recognize and bind to DNA mismatch errors and insertion-deletion loops, while MLH1/PMS2 heterodimers are responsible for excising and re-synthesizing the corrected DNA bases in the mismatch sites (Fig. 1). Expression loss or functional defects in one or more MMR machinery elements can transform the tumor into "mutator phenotype" with numerous frameshift mutations in coding and non-coding MSs and other genetic loci beyond the MSs [10]. Previous studies have elucidated MSI cancers were associated with 100- to 1000-fold increase in mutation rates compared to MSS cancers [11]. Owing to the repetitive sequences of MSs that are particularly prone to replication errors, they are gradually considered as the valuable marker for assessing the integrity of the MMR system. In summary, MSI can be identified as a hypermutated phenotype of genomic MS in the presence of dMMR machinery [12].
In spite of limited knowledge about the contribution of MSI to the development and behavior of gastric cancer, other diseases featured with MSI like the Lynch syndrome have been well explored. Lynch syndrome is an autosomal dominant disorder, primarily caused by germline mutations in five vital DNA MMR genes—MLH1, MSH2, MSH6, PMS2 and rarely PMS1. However, accumulating evidence has demonstrated epigenetic modification occupied an important position in the molecular mechanism of Lynch syndrome. For instance, a constitutional 3’-end deletion of EPCAM, which is the upstream of MSH2, may contribute to Lynch syndrome through epigenetic silencing of MSH2. Similar patterns have also been observed in MSI GC. Recent study has shown that it was the hypermethylation of MLH1, rather than germline mutations in MMR genes, that leads to MSI GC [13]. More than 50% of MSI GCs in sporadic GCs exhibit epigenetic hypermethylation of the hMLH1 promoter [14, 15]. Furthermore, there were no statistical differences observed in the frequencies of MSI phenotype and MLH1 hypermethylation between familial and sporadic GCs [16]. Inactivation of other MSI-related genes has been proposed to be responsible for the remaining cases of MSI GCs. This may provide a clue to follow up in deeper investigation of pathogenesis of MSI GCs.
The molecular characteristics of MSI GC
In recent years, numerous studies have significantly advanced our understanding of the molecular features of MSI GC by identifying key genes that are prominently altered in this malignancy. The MutSigCV analysis performed by the TCGA has reported 37 significantly mutated genes in MSI GC such as RNF43 and NF1[2]. Based on these mutated genes in MSI GC, various cellular functions or pathways that are strongly linked to tumor growth and adaption were enriched such as DNA repair (MSH3 and MSH6), cell signaling (TGFBR2 and ACVR2A), apoptosis (BAX), epigenetic regulation (HDAC2 and ARID1A), and miRNA processing (TARBP2 and XPO5) [9].
Mutations in genes such as KRAS, PI3K, EGFR and MLK3, found in MSI GCs, have been systematically researched in other malignancies characterized by MSI like colorectal cancers [14, 17]. KRAS is one of the most frequently mutated gene in colorectal tumors, but its frequency of mutation in GCs, particularly in MSI GCs, is still unclear. A research conducted by Brennetot. C, et al. indicated that the presence of Ki-ras mutations in MSI GCs showed a similar frequency of 28% (about 4% in total GCs) to those in colorectal tumors. Notably, Ki-ras mutations appeared to be absent in gastric MSS tumors but present in colorectal MSS tumors [18]. On the contrary, BRAF V600E mutation, which were frequently reported in sporadic MSI colon cancers, has never been described in MSI GCs [19]. These suggested MSI GC may possess unique genetic qualities that can easily distinguish them from other MSI cancers. Meanwhile, the role of common MSI-cancer-related gene mutations in MSI GCs should be reconsidered carefully. Substantial evidence has confirmed the crucial role of the phosphoinositide3-kinase (PI3K)/AKT/mammalian target of the rapamycin (mTOR) pathway in MSI GC patients. The prognosis of MSI patients were negatively associated with the number of mutated genes in the PI3K-AKT-mTOR pathway (NMP). A latest study, included four independent cohorts of MSI-H GCs with a total sample size of 316, reported that NMP-high (NMP ≥ 2) patients exhibited a poorer objective response rate (ORR, 29.4% vs. 85.7%, P < 0.001), progression-free survival (PFS, HR = 3.40, P = 0.019), and overall survival (OS, HR = 3.59, P = 0.048) than NMP-low (NMP = 0/1) ones upon immune checkpoint inhibitors (ICIs) treatment [20].
Another team identified a cell intrinsic MSI signature which can distinguish between MSI and MSS GCs by transcriptomic analysis of gastric cancer patient-derived xenografts (PDXs)[21]. The signature, composed of 123 genes with strong differential regulation, can recognize a subset of MSS patients endowed with MSI transcriptional traits, surprisingly achieving a better prognosis than other MSS patients. This may help in developing a better stratification for patients with MSI GC to further optimize the therapeutic strategies.
Detection methods of MSI
At present, the frequently used detection methods for MSI GC in clinical practice are MSI polymerase chain reaction (PCR) and MMR immunohistochemistry (IHC). Besides these traditional molecular biological techniques, novel technologies are emerging, which may have enormous potential to precisely and comprehensively detect and predict the MSI status of gastric cancer patients.
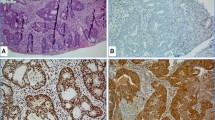
MSI detection by immunohistochemistry
The initial approach for MSI detection is immunohistochemistry (IHC), applying the principle of antigen-antibody binding reaction. This method requires antibodies that have affinity to four key MMR proteins: MLH1, MSH2, MSH6, and PMS2 [22]. The negative staining of one or more of these proteins indicates MMR deficiency [23]. Some studies brought up a concept that IHC could be used as a “standalone” screening method for MSI detection for its simplicity and applicability in most pathology laboratories with moderate cost [24]. However, it should be noticed that IHC yield false-positive results in rare cases. For example, missense mutations in hMLH1 or hMSH6 genes can generate abnormal proteins whose enzymatic activity is suppressed, yet still with normal affinity to antibodies [25].
MSI detection by polymerase chain reaction
PCR is a confirmatory molecular analysis used for MSI detection, which could be briefly described as a comparison of the length of nucleotide repeats between tumor tissue and adjacent normal tissue. Two available panels, the Bethesda and Pentaplex, are generally applied for this method so far [24]. The Bethesda panel contains five predetermined genomic regions: two single-nucleotide (BAT25, BAT-26) and three dinucleotides (D2S123, D5S346, and D17S250). The Pentaplex panel includes five single-nucleotide loci, including BAT-25, BAT-26, NR-21, NR-24, and NR-27.
Three different MSI statuses are established based on different allelic size patterns detected by PCR in the tumor tissue compared to the adjacent normal tissue: MSI-H, MSI-L and MSS. The MSI-H status is determined if shift in size is found in at least two of the five microsatellite loci. The MSI-L is determined if shift in size is found in only one locus out of five. MSS can be identified as no shift in tumor tissue compared to the normal tissue [16]. As MSI-L tumors follow a similar behavioral pattern to MSS tumors, it is always categorized into the MSS type with no need of further testing [4].
Certainly, pros and cons are inherent to either method. The advantages of PCR are undeniable for its extremely high accuracy, establishing it as the gold standard for identifying MSI status by far. Nevertheless, PCR is relatively expensive and time-consuming, posing a main obstacle for its widespread adoption in clinical practice. On the other hand, the strengths of IHC such as its convenience and cheapness make it a more favorable choice in real clinical settings currently.
MMR heterogeneity presents diagnostic challenges in assessing MSI-H/dMMR status. IHC and PCR, as the primary methods for detecting MSI, despite the MMR heterogeneity, showed minimal inconsistency. A study involving 3,228 cases of CRC confirmed the high degree of concordance between PCR and IHC tests, with only 1.6% discordance rate [26]. As of present, considering both clinical utility and technical maturity, IHC and PCR remain our preferred choices.
Novel approaches
Next Generation Sequencing (NGS) was suggested by a recent study as a potentially alternative approach to test MSI status [27]. It achieved to be both diagnostically sensitive (range from 96.4% to 100% across 3 panels) and specific (range from 97.2% to 100%) compared to PCR. Unfortunately, the expensiveness of NGS has limited its clinical feasibility.
Liquid biopsy stands at the forefront of detection methods. It has been proven that liquid biopsy could contribute to the accurate identification and dynamic monitoring of MSI status in a minimally invasive way. A latest study showed tissue-based MSI results were concordant with plasma-based results in 83% (5 out of 6) patients with available tissue sample. Additionally, plasma-based method successfully identified one more patient with MSI-H than tissue-based method [28]. However, due to the limited sample size, further validation is still required.
Moreover, with the application of new technologies such as deep learning and artificial intelligence (AI) in combination with tumor histomorphology in oncological research, the accuracy and objectivity of MSI status determination will be elevated to a higher level [29, 30].
Clinico-pathological and prognostic features of MSI GC
MSI GC is a distinct subtype of gastric cancer that exhibits heterogeneity in genetics and molecular phenotypes as mentioned above, thus determining its unique clinico-pathological and prognostic features. The reported incidence of MSI GC varies from study to study. Hause R, et al. showed that MSI-H GC accounted for 19% of all gastric cancers, ranking third only to endometrial cancer (30%) and colon cancer (19%) in terms of prevalence [31]. Other studies have reported that MSI GC represented only 8% of all gastric cancers [32].
A meta-analysis of 48 studies with 18,612 patients enrolled, of whom 9.2% (n=1,718) were MSI-H GC patients, revealed that MSI-H GC was associated with female sex, older age (> 65 years old), intestinal type of Lauren classification, onset in the middle or distal stomach, lack of lymph node metastases, and TNM stage I-II [33]. By contrast, a multinational meta-analysis that included 121 MSI-H GC patients of 1,556 GC patients, displayed no significant preponderance of female in MSI-H GC [34]. They also found a significant benefit of OS and PFS in MSI-H patients compared to MSS/MSI-L patients with the same T stage.
Several studies have consistently explained that patients with MSI-H GC had better prognosis than those with MSI-L/MSS. For instance, in a secondary post hoc analysis of the MAGIC trial, participants were assigned into two groups based on whether they received surgery alone or perioperative chemotherapy plus surgery [35]. They found that dMMR or MSI-H was associated with a positive prognostic effect in patients who underwent surgery alone but a differentially negative prognostic effect in those who received chemotherapy. Likewise, in the meta-analysis mentioned above, which included patients with resectable GC from four large clinical trials (MAGIC, CLASSIC, ARTIST, and ITACA-S), illustrated the MSI-H group displayed superior 5-year disease-free survival (DFS) and 5-year OS [34]. One underlying mechanism to the satisfactory prognostic outcome in MSI-H GC is probably the presence of immunosurveillance. MSI-H tumors tend to display an enhanced infiltration of CD8 positive-T cell, as well as CD3 [36]. It was also discovered that high level of CD3 and CD8 presentation, along with PD-L1 positivity, were identified as independent prognostic factors for both disease-free survival and overall survival, indicating that these factors may contribute to the better prognosis observed in MSI-H GC.
Response to chemotherapy in MSI GC
In general, patients with MSI-H GC are more likely to be resistant to various chemotherapeutic agents such as 6-thioguanine, temozolomide, platinum-based agents, 5-FU and topoisomerase II inhibitors like etoposide and doxorubicin. [37]. This is probably due to the increasing mutation rate, leaded by dMMR system, in the coding or regulatory sequences of resistance-determined genes, whose products are usually responsible for increasing sensitivity to cytotoxic agents [37]. Furthermore, it has been demonstrated that tolerance to acquired DNA damage and toxic effects of chemotherapeutic agents were conferred upon tumor by the dMMR system. The intact MMR system is able to capture specific DNA adducts induced by cytotoxic agents, while dMMR fails to do so [38]. A large-scale study from Asia reached a similar conclusion that in stage II and III gastric cancer patients, 5-FU-based adjuvant chemotherapy improved DFS in the MSS/MSI-L group, but not in the MSI-H group [39]. Pietrantonio F, et al. investigated the association between MSI status and the efficacy of multimodal treatment strategies to determine whether MSI-H patients could benefit from perioperative or adjuvant chemotherapy [34]. Patients were divided into four groups based on their MSI status as well as their treatment strategy (surgery alone or chemotherapy plus surgery). MSI-L/MSS group showed benefit from chemotherapy plus surgery in comparison with surgery alone. Conversely, no benefit was observed in MSI-H group receiving chemotherapy. Similar findings were corroborated in a post hoc analysis of CLASSIC initiated by Choi, et al. [40]. Among the 592 patients included in the study, MSI-H tumors were identified in 40 patients (6.8%). While adjuvant chemotherapy led to an enhancement in DFS among the MSS group (5-year DFS: 66.8% vs 54.1%; P = 0.002), it did not confer any advantage in the MSI-H group (5-year DFS: 83.9% vs 85.7%; P = 0.931). Although MSI-H esophagogastric cancers only share a small portion of gastric cancer, patients with this type of cancer represent a chemotherapy-refractory subgroup with a significantly shorter PFS on first-line chemotherapy [41].
In summary, MSI status could be regarded as a negative predictor of the effectiveness of chemotherapy. Whereas, limited by the small sample size of MSI-detectable GC patients in most existing studies, more evidence is needed to draw a solid conclusion.
Response to ICIs in MSI GC
Unlike chemotherapy, it has been widely reported that immune checkpoint inhibitors (ICIs) are effective against dMMR cancers [42, 43]. A phase 2 study was performed to evaluate the clinical efficacy of neoadjuvant nivolumab plus ipilimumab and adjuvant nivolumab in 32 patients with dMMR/MSI-H gastric/GEJ adenocarcinoma [7]. Twenty-nine patients underwent surgery with an R0 resection and 58.6% (n=17) patients had pathologic complete response. Moreover, this neoadjuvant therapy based on nivolumab and ipilimumab is viable and does not show any unexpected toxicity. A recent post-hoc analysis of KEYNOTE-059, KEYNOTE-061, and KEYNOTE-062 clinical trials included patients with advanced G/GEJ cancer also drew the similar conclusion [44]. In the KEYNOTE-059 study, pembrolizumab was used as third-line monotherapy, and the ORR of MSI-H patients was 57.1%. In the KEYNOTE-061 study, pembrolizumab monotherapy was compared with paclitaxel as second-line chemotherapy, and the ORR for pembrolizumab was 46.7% vs 16.7% for chemotherapy. In the KEYNOTE-062 study, MSI-H patients were randomized to receive pembrolizumab, pembrolizumab plus chemotherapy (cisplatin and fluoropyrimidine), or chemotherapy alone. The ORR was statistically highest in the group of MSI-H patients receiving both pembrolizumab and chemotherapy compared to pembrolizumab alone (64.7% vs 57.1%) and chemotherapy alone (64.7% vs 36.8%). The research above strongly supported the moderately clinical application of anti-PD-1 therapies for patients with dMMR cancers. Since less attention has been paid to the ICI treatment for dMMR cancers in previous studies, there is an urgent need to refine the standard and indication of immunotherapy for MSI GC [45]. Reporting from the phase III KEYNOTE-859 trial studying perioperative chemoimmunotherapy in patients with HER2-negative advanced gastric cancer was recently presented. Interestingly, in the subgroup analysis of overall survival for patients, pembrolizumab plus chemotherapy consistently exhibited favorable hazard ratios (HRs) compared to placebo plus chemotherapy, especially in patients with MSI-H tumors [46].Researchers have attempted to elucidate the mechanism behind the efficacy of ICIs on MSI cancers. A higher degree of infiltration with activated CD8(+) cytotoxic T lymphocyte (CTL) and activated Th1 cells was observed in MSI colorectal cancers [47]. In response to the microenvironment with active CTL/Th1 cells, MSI tumors selectively upregulated expression of multiple immune checkpoints, including PD-1, PD-L1, CTLA-4, LAG-3, and IDO [47]. This may explain why MSI tumors cannot naturally be eliminated in spite of a hostile microenvironment with active CTL/Th1 cells, but are sensitive to immune checkpoint inhibitors.
Nonetheless, a subset of patients with MSI-H GC may still not benefit from ICIs. Across tumor types, the objective response rate to ICIs in MSI-H tumors appears to peak just above 50%, indicating inherent resistance in nearly half of these tumors [44, 45]. Hence, identifying predictive biomarkers associated with resistance to anti-PD-1 therapies is crucial. Keigo, et al. analyzed 36 patients with MSI-H/dMMR gastrointestinal tumors being treated with PD-1 blockade. Notably, high expression of VEGF-A might predict a negative response to ICIs in MSI-H/dMMR patients, with significantly shorter PFS and OS [48]. Moreover, in a phase II trial of pembrolizumab in patients with advanced MSI-H gastric cancer, the investigators found response heterogeneity within the patients. Diverse T-cell receptor repertoire, as well as increased PD-1+ CD8+ T cells were associated with durable clinical benefit to pembrolizumab, respectively [49]. These findings underscore that dMMR/MSI-H heterogeneity may have clinical implications for response to ICIs.
In addition to heterogeneity in dMMR/MSI-H GC, genetic changes may be another critical factor to explain the encoring results of ICIs efficacy on MSI cancers. Researchers have focused on the role of gene mutations in immunotherapy. A recent study, which analyzed 45 patients with MSI-H/dMMR gastrointestinal (GI) tumors who received PD-1 blockade, found that patients with low tumor mutational burdens (TMBs) had lower ORR and significantly shorter PFS [50]. Especially, PTEN mutations, which were mutually exclusive with a low TMB, were significantly associated with lower ORRs. These suggested that low TMBs and PTEN mutations are promising predictors of a negative response to PD-1 blockade in MSI-H GI tumors. Another study provided by Wang, et al. identified AKT1 and CDH1 mutations as independent predictors of poor PFS and primary resistance to ICIs in dMMR/MSI-H GI cancer [51].
In summary, incorporating immunotherapy into the perioperative management strategy has shown tremendous potential in the treatment for MSI GC. Research encompassing the mechanism of how immunotherapy effect MSI-H GC will facilitate us to better stratify patients for customized treatment.
Discussion
In conclusion, gastric cancer with microsatellite instability, which makes up only a small proportion of total gastric cancers, is a noteworthy subtype characterized by its unique molecular features and diverse phenotypes. MSI GC is considered a typically hypermutated subtype with higher TMBs. It is literally caused by the dMMR system, resulting from mutational inactivation and epigenetic silencing of MMR machinery elements, which subsequently leads to mutations in microsatellite regions or other genetic loci beyond microsatellites. MSI cancers can be classified into three categories: MSI-H, MSI-L and MSS. Several genes have been confirmed to display significantly differential expression in MSI-H GC such as RNF43, B2M and NF1. Genes such as KRAS and PI3K that have been previously reported in other MSI-related malignancies have also been found in MSI-H GC yet with different patterns of expression. Utilizing biological techniques like IHC and PCR can help to identify dMMR system and determine the status of MSI in clinical practice. Novel techniques such as NGS, liquid biopsy, deep learning classifier and AI, that can significantly improve the specificity and sensitivity of detection, may be widely applied in clinical settings in the near future. MSI GCs show exclusive clinico-pathological characteristics and are particularly associated with female sex, older age, intestinal type of Lauren classification, middle or distal location, no lymph node involvement and TNM stage I-II. As for the treatment, MSI-H GC presents a satisfactory response to ICIs, while not to chemotherapeutic agents. Possible explanations for this could be owing to the enhanced immune response in the microenvironment and genetic changes in crucial genes like AKT1 and CDH1. Clinical trials such as KEYNOTE-059, KEYNOTE-061, and KEYNOTE-062 all reached a similarly encouraging result that anti-PD-1 therapy could help MSI GC patients to have better prognosis. Plenty of attempts have been made to identify predictive markers of the efficacy of immunotherapy in MSI-H patients. Due to the increased mutation rate in resistance-related genes leaded by dMMR system, a majority of MSI-H GC patients exhibit resistance to the standard chemotherapy. However, the application value of cytotoxic agents on MSI-H cancer is still unclear due to varying efficacy results ranging from detrimental to beneficial effects. Further research is required to gain deeper insights into the tumorigenesis, growth and response to microenvironmental stimulus of MSI GC, in order to define the best treatment strategy tailored to the individual.
An increasing number of studies have revealed that the percentage of MSI-H patients who could gain prognostic benefits or symptom alleviation from ICIs treatment was less than 50%. The heterogeneity of MSI-H malignancy is highly suspected to be the reason of the distinct efficacy of ICIs treatment among different MSI-H patients. To deal with this, an accurate and comprehensive stratification for MSI GCs, based on the intrinsic properties of the tumor in genetic, epigenetic, metabolic and immunological levels, need to be developed to aid the precise treatment for patients with MSI GCs. In 2015, researchers from the Asian Cancer Research Group (ACRG) integrated clinical follow-up data and gene expression profiles to derive a molecular classification scheme for gastric tumors, mainly based on the MSI status, which is composed by four subtypes: MSI-H, MSS/TP53+, MSS/TP53- and MSS/EMT. Survival analysis illustrated a substantial difference in OS among four subtypes, in which the MSI-H subtype achieved the best prognosis, followed by MSS/TP53+ and MSS/TP53-, with the MSS/EMT subtype presenting the worst prognosis (p=0.0004). This was then validated by three more independent cohorts: Samsung Medical Center cohort 2 (SMC-2, n=277), Singapore cohort (n=200) and TCGA gastric cohort (n=205) [3]. Another study utilized the non-negative matrix factorization (non-nMF)-based consensus clustering to divide stomach adenocarcinoma (STAD) with MSI-H status into two subtypes: MSI-H1 and MSI-H2. Although there was no significant difference in clinical characteristics between two groups, MSI-H1 had a much poorer prognosis than MSI-H2 subtype with a shorter DFS and OS. They further elaborated the worse prognosis observed in MSI-H1subgroup might be related to the enrichment of inhibitory immune receptors and chemokines, manifesting as a bulk of suppressive immune signatures detected in differential expression analysis [52]. Moreover, the role of heterogeneity in MSI tumors remains to be investigated, as it has been reported that dMMR fraction in MMR heterogeneous tumors could act as an endogenous cancer vaccine by promoting immune surveillance [53]. These findings established a consistent and unified framework for later clinical and pre-clinical translational research in this field, and at the same time they reminded us that the underlying heterogeneity in MSI GC patients urgently needs to be further explored and better interpreted for the development of rational therapeutic regimens and the amelioration of side effects for these patients.
As previously mentioned, the epigenetic silencing of MLH1 rather than germline mutation was highly suspected to be responsible for MSI GC. It highlighted a perspective that epigenetic regulation might play a vital role in the occurrence of MSI GC. A latest study has demonstrated gastrointestinal (GI) tract adenocarcinomas displayed a relatively high frequency of CpG island methylator phenotype (CIMP), thus could be categorized into two subgroups based on CIMP status: CIMP-Low (CIMP-L) and CIMP-High (CIMP-H) [54]. In this study, although upper GI tract and proximal colon were both affected by CIMP-H, the epigenetic silencing of MLH1 was mainly observed in the distal stomach and proximal colon. Additionally, within the proximal stomach and esophagus, only 14% (4 out of 29) CIMP-H tumors showed MLH1 epigenetic silencing and MSI, yet 79% (23 out of 29) were MSS and CIN. This provided a clue that the epigenetically related occurrence of MSI might have its “favorable” location in the stomach. Even though there is a growing body of research focusing on MSI GCs from multidimensional aspects, the knowledge about the molecular mechanism of MSI GC development is still superficial and incomprehensive. Further studies are desperately needed to fill in the blanks.
Availability of data and materials
Not applicable.
References
Sung H, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–49.
Comprehensive molecular characterization of gastric adenocarcinoma. Nature. 2014;513(7517):202–9.
Cristescu R, et al. Molecular analysis of gastric cancer identifies subtypes associated with distinct clinical outcomes. Nat Med. 2015;21(5):449–56.
Baretti M, Le DT. DNA mismatch repair in cancer. Pharmacol Ther. 2018;189:45–62.
Boland CR, et al. A National Cancer Institute Workshop on Microsatellite Instability for cancer detection and familial predisposition: development of international criteria for the determination of microsatellite instability in colorectal cancer. Cancer Res. 1998;58(22):5248–57.
Joshi SS, Badgwell BD. Current treatment and recent progress in gastric cancer. CA Cancer J Clin. 2021;71(3):264–79.
André T, et al. Neoadjuvant Nivolumab Plus Ipilimumab and Adjuvant Nivolumab in Localized Deficient Mismatch Repair/Microsatellite Instability-High Gastric or Esophagogastric Junction Adenocarcinoma: The GERCOR NEONIPIGA Phase II Study. J Clin Oncol. 2023;41(2):255–65.
Garrido-Ramos MA. Satellite DNA: An Evolving Topic. Genes (Basel). 2017;8(9):230.
Yamamoto H, Imai K. Microsatellite instability: an update. Arch Toxicol. 2015;89(6):899–921.
Puliga E, et al. Microsatellite instability in Gastric Cancer: Between lights and shadows. Cancer Treat Rev. 2021;95:102175.
Dudley JC, et al. Microsatellite Instability as a Biomarker for PD-1 Blockade. Clin Cancer Res. 2016;22(4):813–20.
Li K, et al. Microsatellite instability: a review of what the oncologist should know. Cancer Cell Int. 2020;20:16.
Seo HM, et al. Clinicopathologic characteristics and outcomes of gastric cancers with the MSI-H phenotype. J Surg Oncol. 2009;99(3):143–7.
Corso G, et al. Oncogenic mutations in gastric cancer with microsatellite instability. Eur J Cancer. 2011;47(3):443–51.
Ottini L, et al. Patterns of genomic instability in gastric cancer: clinical implications and perspectives. Ann Oncol. 2006;17(Suppl 7):vii97-102.
Leite M, et al. MSI phenotype and MMR alterations in familial and sporadic gastric cancer. Int J Cancer. 2011;128(7):1606–13.
van Grieken NC, et al. KRAS and BRAF mutations are rare and related to DNA mismatch repair deficiency in gastric cancer from the East and the West: results from a large international multicentre study. Br J Cancer. 2013;108(7):1495–501.
Brennetot C, et al. Frequent Ki-ras mutations in gastric tumors of the MSI phenotype. Gastroenterology. 2003;125(4):1282.
Normanno N, et al. Heterogeneity of KRAS, NRAS, BRAF and PIK3CA mutations in metastatic colorectal cancer and potential effects on therapy in the CAPRI GOIM trial. Ann Oncol. 2015;26(8):1710–4.
Wang Z, et al. Mutations of PI3K-AKT-mTOR pathway as predictors for immune cell infiltration and immunotherapy efficacy in dMMR/MSI-H gastric adenocarcinoma. BMC Med. 2022;20(1):133.
Corso S, et al. A Comprehensive PDX Gastric Cancer Collection Captures Cancer Cell-Intrinsic Transcriptional MSI Traits. Cancer Res. 2019;79(22):5884–96.
Luchini C, et al. ESMO recommendations on microsatellite instability testing for immunotherapy in cancer, and its relationship with PD-1/PD-L1 expression and tumour mutational burden: a systematic review-based approach. Ann Oncol. 2019;30(8):1232–43.
Vilar E, Gruber SB. Microsatellite instability in colorectal cancer-the stable evidence. Nat Rev Clin Oncol. 2010;7(3):153–62.
Amato M, et al. Microsatellite Instability: From the Implementation of the Detection to a Prognostic and Predictive Role in Cancers. Int J Mol Sci. 2022;23(15):8726.
Murphy KM, et al. Comparison of the microsatellite instability analysis system and the Bethesda panel for the determination of microsatellite instability in colorectal cancers. J Mol Diagn. 2006;8(3):305–11.
De Guyot D’Asnières Salins A, et al. Discordance between immunochemistry of mismatch repair proteins and molecular testing of microsatellite instability in colorectal cancer. ESMO Open. 2021;6(3):100120.
Salipante SJ, et al. Microsatellite instability detection by next generation sequencing. Clin Chem. 2014;60(9):1192–9.
Chakrabarti S, et al. Detection of microsatellite instability-high (MSI-H) by liquid biopsy predicts robust and durable response to immunotherapy in patients with pancreatic cancer. J Immunother Cancer. 2022;10(6):e004485.
Muti HS, et al. Development and validation of deep learning classifiers to detect Epstein-Barr virus and microsatellite instability status in gastric cancer: a retrospective multicentre cohort study. Lancet Digit Health. 2021;3(10):e654–64.
Park JH, et al. Artificial Intelligence for Predicting Microsatellite Instability Based on Tumor Histomorphology: A Systematic Review. Int J Mol Sci. 2022;23(5):2462.
Hause RJ, et al. Classification and characterization of microsatellite instability across 18 cancer types. Nat Med. 2016;22(11):1342–50.
Le DT, et al. Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science. 2017;357(6349):409–13.
Polom K, et al. Meta-analysis of microsatellite instability in relation to clinicopathological characteristics and overall survival in gastric cancer. Br J Surg. 2018;105(3):159–67.
Pietrantonio F, et al. Individual Patient Data Meta-Analysis of the Value of Microsatellite Instability As a Biomarker in Gastric Cancer. J Clin Oncol. 2019;37(35):3392–400.
Smyth EC, et al. Mismatch Repair Deficiency, Microsatellite Instability, and Survival: An Exploratory Analysis of the Medical Research Council Adjuvant Gastric Infusional Chemotherapy (MAGIC) Trial. JAMA Oncol. 2017;3(9):1197–203.
Angell HK, et al. PD-L1 and immune infiltrates are differentially expressed in distinct subgroups of gastric cancer. Oncoimmunology. 2019;8(2):e1544442.
Fink D, et al. The effect of different chemotherapeutic agents on the enrichment of DNA mismatch repair-deficient tumour cells. Br J Cancer. 1998;77(5):703–8.
Carethers JM, et al. Mismatch repair proficiency and in vitro response to 5-fluorouracil. Gastroenterology. 1999;117(1):123–31.
An JY, et al. Microsatellite instability in sporadic gastric cancer: its prognostic role and guidance for 5-FU based chemotherapy after R0 resection. Int J Cancer. 2012;131(2):505–11.
Choi YY, et al. Microsatellite Instability and Programmed Cell Death-Ligand 1 Expression in Stage II/III Gastric Cancer: Post Hoc Analysis of the CLASSIC Randomized Controlled study. Ann Surg. 2019;270(2):309–16.
Janjigian YY, et al. Genetic Predictors of Response to Systemic Therapy in Esophagogastric Cancer. Cancer Discov. 2018;8(1):49–58.
Kim ST, et al. Comprehensive molecular characterization of clinical responses to PD-1 inhibition in metastatic gastric cancer. Nat Med. 2018;24(9):1449–58.
Ludford K, et al. Neoadjuvant Pembrolizumab in Localized Microsatellite Instability High/Deficient Mismatch Repair Solid Tumors. J Clin Oncol. 2023;41(12):2181–90.
Chao J, et al. Assessment of Pembrolizumab Therapy for the Treatment of Microsatellite Instability-High Gastric or Gastroesophageal Junction Cancer Among Patients in the KEYNOTE-059, KEYNOTE-061, and KEYNOTE-062 Clinical Trials. JAMA Oncol. 2021;7(6):895–902.
Jain R, Denlinger CS, Dotan E. Refining Immunotherapy for the Treatment of Gastric Cancer With High Microsatellite Instability. JAMA Oncol. 2021;7(6):902–3.
Rha SY, et al. Pembrolizumab plus chemotherapy versus placebo plus chemotherapy for HER2-negative advanced gastric cancer (KEYNOTE-859): a multicentre, randomised, double-blind, phase 3 trial. Lancet Oncol. 2023;24(11):1181–95.
Llosa NJ, et al. The vigorous immune microenvironment of microsatellite instable colon cancer is balanced by multiple counter-inhibitory checkpoints. Cancer Discov. 2015;5(1):43–51.
Chida K, et al. Transcriptomic Profiling of MSI-H/dMMR Gastrointestinal Tumors to Identify Determinants of Responsiveness to Anti-PD-1 Therapy. Clin Cancer Res. 2022;28(10):2110–7.
Kwon M, et al. Determinants of Response and Intrinsic Resistance to PD-1 Blockade in Microsatellite Instability-High Gastric Cancer. Cancer Discov. 2021;11(9):2168–85.
Chida K, et al. A Low Tumor Mutational Burden and PTEN Mutations Are Predictors of a Negative Response to PD-1 Blockade in MSI-H/dMMR Gastrointestinal Tumors. Clin Cancer Res. 2021;27(13):3714–24.
Wang Z, et al. Combination of AKT1 and CDH1 mutations predicts primary resistance to immunotherapy in dMMR/MSI-H gastrointestinal cancer. J Immunother Cancer. 2022;10(6):e004703.
Yang Y, et al. Heterogeneity of MSI-H gastric cancer identifies a subtype with worse survival. J Med Genet. 2021;58(1):12–9.
Amodio V, et al. Genetic and pharmacological modulation of DNA mismatch repair heterogeneous tumors promotes immune surveillance. Cancer Cell. 2023;41(1):196-209.e5.
Liu Y. Comparative Molecular Analysis of Gastrointestinal Adenocarcinomas. Cancer Cell. 2018;33(4):721–735.e8.
Acknowledgments
Not applicable.
Funding
National Natural Science Foundation of China 81972228 (XW).
Author information
Authors and Affiliations
Contributions
ZZ, ZL, and XW collected studies and integrated information; ZT, YG, and YS supervised the authenticity of articles; ZZ, ZL, and XW drafted and revised the manuscript; RL and YS reviewed and edited the manuscript; XW led the project. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, Z., Liu, Z., Gu, Y. et al. Microsatellite instability in gastric cancer: molecular features and clinical implications. CCB 3, 12 (2024). https://doi.org/10.1007/s44272-024-00017-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44272-024-00017-9