Abstract
Mechanical ventilation is an important life-saving therapy for general anesthesia and critically ill patients, but ventilation itself may be accompanied with lung injury. Ventilator-induced lung injury (VILI) exacerbates pre-existing lung disease, leading to poor clinical outcomes. Especially for patients undergoing cardiothoracic surgery and receiving one-lung ventilation (OLV), optimizing the parameters of OLV is closely related to their prognosis. It is not clear what is the best strategy to minimize VILI through adjusting ventilation parameters, including tidal volume, positive end expiratory pressure and driving pressure, etc. Different parameters, in combination, are responsible for VILI. Protective ventilation strategies, aiming to reduce postoperative pulmonary complications, have been discussed in many clinical studies and different opinions have been raised. This review addresses the pathogenesis of VILI and focus on the OLV management and better protective OLV strategies during thoracic surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Mechanical ventilation is a very important medical procedure for anesthetists, even a potential life-saving therapy for some critically ill patients [1]. But this invasive procedure sometimes is accompanied with unwanted effects. And the term, VILI, stands for ventilator-induced lung injury, was introduced in 1993 [2]. Over the past three decades, researchers and doctors are trying to understand the mechanism of VILI through animal models and clinical practices. It is recognized that lung injury can be caused by barotrauma, volutrauma, atelectrauma, and biotrauma [3]. With the understanding of VILI, an additional goal of mechanical ventilation, including maintaining gas exchange and minimizing the work of breathing, has established: to minimize VILI. Various ventilation strategies are applied and well-studied.
According to the Global Cancer Statistics 2020, lung cancer was still the leading cause of cancer death, with an estimated number of 1.8 million deaths (18%) [4]. With the rising number of thoracic surgeries, the need for OLV is also increasing. Postoperative pulmonary complications (PPCs), especially after thoracic surgery, can affect the outcomes of patients and bring tremendous burden to patients and the medical system [5, 6].
As reported, the incidence of PPCs after thoracic surgery is 30–50% [7]. The use of video-assisted thoracic surgery approach has significantly lowered the rate of PPCs of elder patients from 45 to 28% [8]. Aside from the high rate of PPCs, meeting surgical needs and providing satisfactory surgical fields exposure also require adjusting ventilation parameters. Guideline for patients receiving lobectomy recommended a tidal volume (TV) of 6 mL/kg, a positive end-expiratory pressure (PEEP) of 5 cm H2O, and a partial pressure of carbon dioxide (PaCO2) of 50–70 mmHg [9]. But the recommendations of particular parameters did not take preoperative complications and intraoperative conditions into consideration, personalized OLV management is still critical for improving clinical outcomes and reducing PPCs [10].
This review is about the current studies associated with the mechanism of VILI and attempts to modify mechanical ventilation, especially OLV.
2 The definitions of postoperative pulmonary complications
The Lancet Commission on Global Surgery reported that more than 310 million surgical procedures are performed worldwide each year [11]. In patients undergoing surgery with general anesthesia and mechanical ventilation over 2 h, the incidence of PPCs is 33.4% [7]. Previous estimates of the incidence of PPCs have ranged from 5 to 80%, depending on the definition, severity consideration and types of surgery [7, 12,13,14,15].
Studies use different combinations and severity of postoperative pulmonary events to define PPCs. It is quite different in incidence of PPCs with different evaluation criterion, even in the same population [16]. The definitions of PPCs described in the ARISCAT study [12] are commonly used in clinical settings and studies. And the diagnostic criteria are listed in European Perioperative Clinical Outcome definitions as a standard definition of PPCs [17], showing in Table 1. Other scoring systems, like Melbourne Group Scale [18] and LAS VEGAS [19] criteria are showed in Tables 2 and 3.
3 The mechanism of ventilation-induced lung injury
In addition to risk factors related to patient and surgery, VILI is also one of the major causes of PPCs, which can be controlled and adjusted with anesthesia management. Improper use of positive pressure ventilation will be accompanied by serious complications, brings pulmonary function deterioration [20, 21]. Investigators took decades to reach thorough understanding of the mechanism of VILI. And the commonly recognized types of injury are barotrauma, volutrauma, atelectrauma, and biotrauma, showing in Fig. 1.
3.1 Barotrauma
The most commonly recognized form of barotrauma is the presence of extra-alveolar gas [22]. Barotrauma is caused by high transpulmonary pressure (Ptp) and may occur even at lower airway pressure or alveolar pressure (Palv) if pleural pressure (Ppl) is extremely negative. This phenomenon was firstly recognized and reported in 1944 by Mackin and his colleagues. A general overinflation and an elevated intra-alveolar pressure gradient lead to air escaping through ruptured alveolar bases, penetrating tissues and causing interstitial emphysema, mediastinal emphysema, subcutaneous emphysema, pericardial and retroperitoneal pneumatosis [23].
3.2 Volutrauma
In addition to high ventilation pressure, which can lead to alveolar rupture, excessive chest stretch due to high tidal volume can cause lung injury [24], termed “volutrauma” [25].
The debate of barotrauma versus volutrauma started long ago. In a classic study in 1992, by comparing high-pressure low-volume strategy and low-pressure high-volume strategy, Dreyfuss and colleagues found that volutrauma is more important than barotrauma, and coined the term “volutrauma” to emphasize that the choice of tidal volume is the single most important risk factor of mechanical ventilation associated lung injury [26].
It is true that high airway pressure alone does not cause VILI, as studies confirmed. However, the pertinent distending pressure of the lungs is not simply the airway pressure but the transpulmonary pressure (alveolar pressure minus pleural pressure, Ptp = Palv−Ppl), the difference between the pressure inside and outside the lung [25]. And the researcher pointed out that failure to consider transpulmonary pressure in mechanically ventilated patients can lead to miscalculating VILI risk.
3.3 Atelectrauma
Ventilation at an absolutely low volume may also contribute to lung injury. During mechanical ventilation, the stress and strain multiply at the junction of overinflated lung and normal inflated lung, the opened and collapsed lung tissue [27]. In 1970, Mead and colleagues presented the idea by models and equations [28]. And Slutsky named the repetitive opening/collapse injury “atelectrauma” [29]. Cyclic collapsing and opening of the lung in the operation side also can cause severe trauma.
3.4 Biotrauma
Intracellular mediator is another cause of lung injury induced by mechanical ventilation. Kawano reported in 1987 that large number of granulocytes were found in damaged lung after mechanical ventilation. And with depletion of granulocytes, the animals showed better gas exchange and improved pulmonary function [30]. And the concept of “biotrauma” was introduced in 1998 by Tremblay and Slutsky [31]. Mechanical ventilation can trigger the release of injurious inflammatory mediators, including interleukin (IL)-1β, IL-6, IL-8, macrophage inflammatory protein-2, tumor‑necrosis factor-α, etc. The proinflammatory response may happen in the circulatory system, not just within the lung, which is different from the other types of injuries [32].
4 Protective ventilation strategies
The concept of protective ventilation originated from the treatment of acute respiratory distress syndrome (ARDS) and has been widely used in clinical respiratory support therapy and mechanical ventilation during general anesthesia. As reported in previous randomized control trials, the protective ventilation procedure consists of mainly three parts: TV, PEEP and lung recruitment maneuvers (RM).
In the recent decade, researchers tried various protective ventilation parameters, both combined and separated [33,34,35,36]. In the IMPROVE trial, the protective ventilation strategy group implemented specific measures. This included utilizing a tidal volume of 6 to 8 mL per kilogram of predicted body weight (PBW), maintaining a PEEP of 6 to 8 cm H2O, and performing lung recruitment maneuvers every 30 min after endotracheal intubation. The trial results demonstrated that the implementation of a lung-protective ventilation strategy in intermediate-risk and high-risk patients undergoing major abdominal surgery yielded favorable clinical outcomes. Furthermore, this approach was associated with a reduction in both major pulmonary and extrapulmonary complications [33]. However, in the study, PEEP was used in only one group and in combination with periodic RM and low TV, while the control group received no PEEP, no RM, and high TV. These combinations make it difficult to identify the benefits of low TV, PEEP or RM respectively. One other study showed TV is not the determining factor: among the patients undergoing major surgery, receiving ventilation with low tidal volume of 6 mL/kg PBW compared with conventional tidal volume of 10 mL/kg PBW, with PEEP applied the same between groups, did not significantly reduce pulmonary complications within the first 7 postoperative days [34]. Atelectasis, resulted in low tidal volume, can be worse when FiO2 is high. Low FiO2 may prevent absorption atelectasis [9, 37].
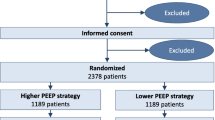
As for PEEP, studies also gave different answers. In previous studies, using high level of PEEP and RM may decrease the driving pressure and improve clinical outcomes and decrease pulmonary complications [35, 38, 39]. The PROVHILO trial compared the lower PEEP (≤ 2 cm H2O) group with intraoperative ventilation at a tidal volume of 8 mL/kg PBW vs the higher PEEP (12 cm H2O) group with a tidal volume of 8 mL/kg PBW combined with scheduled recruitment maneuvers [36]. It reveals the strategy with a higher PEEP and RM did not protect patients undergoing open abdominal surgery against postoperative complications. In some ways, higher level of PEEP may also impaired hemodynamics, which made it unsuitable for hemodynamically unstable patients. In the research using PEEP titration method with electrical impedance tomography revealed a preferred PEEP level for patients with a body mass index (BMI) ≥ 35 kg/m2 about 18.5 cm H2O [40]. The PROBESE trial also showed that ventilation strategy with a higher PEEP of 12 cm H2O and alveolar recruitment maneuvers compared with a strategy with a lower PEEP of 4 cm H2O, did not reduce PPCs [41].
Another controversial topic is the lung recruitment maneuver. The recruitment maneuvers were supposed to reduce pulmonary atelectasis and reported to reduce severe pulmonary complications among patients with hypoxemia [42, 43]. On the opposite, several studies indicated that applying RM did not bring better clinical outcomes, even was associated with increased cardiovascular adverse events [44, 45].
Driving pressure (DP, plateau minus end-expiratory airway pressure), also a predictor of outcomes in patients with ARDS, has been suggested to be the key variable for optimization when performing mechanical ventilation in patients with ARDS. On contrary, a study reported no significant difference between driving pressure lowering maneuvers group and protective ventilation group with a fixed PEEP of 5 cm H2O [46].
There is still no generally accepted “perfect” ventilation strategy.
5 One-lung ventilation strategies
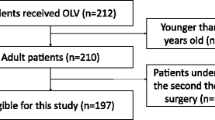
The one-lung ventilation in thoracic surgery usually consists of three stages: preoperative two-lung ventilation, intraoperative one-lung ventilation and postoperative two-lung ventilation. In the research analyzing the postoperative outcome of lung cancer resections for patients over 60 years old, Detillon and colleagues reported the incidence of PPCs is as high as 29.9% [47]. Considering the risks of hypoxemia and lung injury associated with high airway pressure during OLV, the ideal ventilation strategy should be modified individually and cover the above three stages. In clinical scenarios, anesthesiologists change the ventilation parameters in the following aspects to achieve better OLV.
5.1 Tidal volume
Considering individualized tidal volume, PBW, rather than actual body weight (ABW), should be used for estimating required TV [48]. There is significantly stronger correlation between height and lung size rather than ABW. ABW could produce excessive TV in obese patients with BMI higher than 40 kg/m.2, and inadequately low TV for underweight patients. Due to the redistribution of blood and the suppression of hypoxic pulmonary vasoconstriction, the TV during OLV is not half of that in two-lung ventilation. A proper tidal volume in OLV may be 4–6 mL/kg PBW [49]. A multicenter retrospective study shows protective ventilation with TV of 4.4 mL/kg (compared with TV of 6.4 mL/kg) was not associated with a reduction in pulmonary complications [50].
Low tidal volume may bring increased dead space and hypercapnia. An increase of respiratory rate (RR) from 12 per minute to 20 per minute could remove CO2 partly but increasing RR alone for a “normal” PaCO2 is not recommended. Most patients could burden a PaCO2 near 70 mmHg [51]. Shorten expiratory time and high RR may bring greater intrinsic PEEP and impair respiratory system [52].
5.2 Ventilation mode
Volume-controlled ventilation (VCV) and pressure-controlled ventilation (PCV) were the first two ventilation modes used during surgery. In VCV mode, the preset tidal volume is reached in a constant flow rate, which ensures an expected minute ventilation. The peak airway pressure can change with changes of lung compliance and airway resistance. In PCV mode, the inspiratory pressure is constant, but the tidal volume may change. PCV mode offers a lower peak airway pressure and intrapulmonary shunt during OLV [53]. Hypoxemia may occur to patients with poor lung compliance. In recent years, dual-controlled ventilation modes such as pressure-controlled volume guaranteed (PCV-VG) mode developed. PCV-VG is favorable due to decelerating flow compared to constant flow in VCV mode. And the tidal volume, which may change in PCV mode, is guaranteed. PCV-VG mode is also reported to reduce lung inflammatory response [54]. The incidence of PPCs, though, reported in the latest randomized controlled trial, did not differ across three ventilation mode groups (VCV, PCV and PCV-VG) for thoracic surgery patients with OLV [55].
5.3 PEEP
During protective ventilation with low TV, the risk of atelectasis is relatively high. PEEP may improve oxygenation and mitigate VILI by reducing atelectasis and cyclic lung collapse [3, 56]. Excessive PEEP, however, may cause barotrauma, inadequate ventilation-perfusion ratio and hypotension due to high intrathoracic pressure and low bloodflow to the right atrium [57]. Many studies have tried to find a proper PEEP level. There are two prevailing choices: the one is high PEEP (≥ 10 cm H2O) and the other is low PEEP (2–5 cm H2O). Fixed PEEP, however, does not consider the individual condition of patients, such as pre-existing pulmonary disease and lung volume changes after lung resection, etc. The concept of “PEEP titration” emerged.
One way to titrate PEEP is by minimizing DP. Driving pressure-guided ventilation strategy during OLV could lower the incidence of PPCs compared with conventional protective ventilation in thoracic surgery [58]. The core of protective ventilation is to lower mechanical power (MP). MP is the amount of energy transferred to the lung parenchyma per unit of time during mechanical ventilation [59, 60]. Recent studies showed the correlation between high MP and severer VILI both in animal models and patients [61,62,63]. The power equation is computed and verified [64, 65], showed in Formula 1, but very difficult to calculate. A surrogate formula using only RR, Vt, peak inspiratory pressure, PEEP and plateau pressure, all parameters can be easily acquired from the ventilator, to compute MP, showed in Formula 2 [66]. DP (= plateau pressure−PEEP), is the most important parameter in the equation. By modifying PEEP level, a minimal DP may be achieved. In the study of iPROVE-OLV, PEEP titration in the individualized perioperative open lung ventilation strategy in patients on OLV may probably help to reduce PPCs [67]. The investigators figured out the MP threshold of 12 J/min for VILI, meaning that patients are under higher risk of lung injury and whole-lung edema when MP is over 12 J/min, and the injury can be detected by CT scan [60]. The DP ≤ 14 cm H2O is recommended.
∆V: tidal volume; ELrs: the elastance of the respiratory system; I: E: the inspiratory-to-expiratory time ratio; Raw: the airway resistance.
Vt: the tidal volume in liters.
By utilizing electrical impedance tomography (EIT), the ventilation condition of lungs becomes visible [68, 69], allowing for non-invasive, real-time dynamic and visual monitoring. This technology is not only useful for PEEP titration but also for adjusting other parameters [68, 69]. The EIT device, equipped with one belt containing 16 electrodes placed around the thorax at the fifth intercostal space, can monitor the distribution of ventilation in different body positions. It records the gas exchange status under various TV and PEEP values and evaluates the effectiveness of RM. Additionally, the global inhomogeneity index can be calculated using EIT measurements [70]. It is important to note that during thoracoscopic surgery, the placement of the EIT belt may conflict with surgical site, making it difficult to apply EIT. Furthermore, EIT is not applicable when the lung is collapsed or unventilated. In further study, the researchers pointed out that using EIT-guided PEEP titration in elder patients undergoing thoracoscopic surgery, the optimal PEEP (range from 9–13 cm H2O) is obviously higher than previously recommend 5 cm H2O [68]. Comparing with fixed PEEP group, the patients in individual PEEP group had higher PaO2/FiO2 ratio, higher dynamic respiratory system compliance and lower DP. Surprisingly, evidence shows that EIT measurements can help to modify ventilation parameters and develop individual ventilation strategies.
5.4 Lung recruitment strategy
Lung recruitment is a big part of protective ventilation. It can re-open the collapsed alveoli, improve oxygenation and reduce ventilation dead space. During OLV, it is crucial to perform RM to prevent prolonged atelectrauma in the collapsed lung on the surgical side. Additionally, the ventilated lung on the non-surgical side also requires RM due to the potential risk of significant absorption atelectasis caused by exposure to high fraction of oxygen [71]. A systemic review of PEEP and RM shows that recruitment, reported in many studies, significantly improves PaO2 during OLV [72].
When switching from one-lung ventilation to two-lung ventilation, a controlled high airway pressure (usually 40 cm H2O) is needed for re-expansion. When transitioning from OLV to two-lung ventilation, it is necessary to apply a controlled high airway pressure (typically around 40 cm H2O) to facilitate re-expansion of the collapsed lung. One commonly utilized and extensively studied method for achieving this is through the application of sustained inflation [73]. This involves the use of continuous positive airway pressure (CPAP) set at 40 cm H2O for a duration of 40 s. Lung ultrasound and EIT are popular non-invasive bedside imaging techniques for RM quantifying [74]. However, the sudden increase in airway pressure can stimulate the release of proinflammatory factors and increase alveolar shear strain. A stepwise RM, increasing pressure step by step, shows less hemodynamic change and less mechanical and biochemical lung injury [75, 76].
Hypoxemia during OLV for thoracic surgery is common in anesthesia [77]. Application of CPAP to the non-ventilated lung is usually recommended. However, CPAP may impede surgical exposure in the hemithorax. Other techniques treating hypoxemia were developed. Selective insufflation using fiberoptic bronchoscope was reported to improve oxygenation effectively [78]. Intermittent positive airway pressure method to the non-ventilated lung using a special filter can also correct desaturation [79].
6 Discussion
Current studies on protective ventilation have not fully elucidated the roles of ventilation parameters and the dominant factor of VILI. The development of PPCs, even the mild ones, can be associated with in-hospital mortality, ICU admission and re-admission, prolonged hospital stay and other sever outcomes, which is a huge burden for patients’ family and medical care system, making prevention of PPCs not only a therapeutic but an economic goal for optimization of mechanical ventilation [80]. And a personalized ventilation strategy for surgical and critically ill patients according to lung physiology and morphology and disease etiology may improve pulmonary function and clinical outcomes [81].
Optimizing ventilation strategy is a feasible attempt to lower the incidence of PPCs. The strategy using relatively low TV (6–8 mL/kg PBW, not absolutely low), low PEEP (PEEP ≤ 4 cm H2O) with RM, and low DP (≤ 14 cm H2O) is recommended. For OLV, the recommendations are: relatively low tidal volume of 4–6 mL/kg PBW; individualized PEEP for minimized DP (better ≤ 14 cm H2O); stepwise lung recruitment maneuver before OLV and after switching to two-lung ventilation; and minimal FiO2 to keep SpO2 ≥ 90%.
The effectiveness of strategies described above is still controversial. A large randomized controlled trial investigating high versus low positive end-expiratory pressure during general anesthesia for open abdominal surgery (PROVHILO trial) suggests that an intraoperative protective ventilation strategy should include a low TV and low PEEP, without RMs [36]. For obese patients, indicated in the PROBESE study, higher level of PEEP and RM did not reduce PPCs [41]. And the first randomized controlled trial discussing protective ventilation during OLV in thoracic surgery (PROTHOR study) compares the effects of intraoperative high PEEP with RM versus low PEEP without RM on PPC [82]. There is still a long way for finding a perfect way to minimize lung injury caused by mechanical ventilation.
Availability of data and materials
Data availability is not applicable to this article as no new data were created or analyzed in this study.
Abbreviations
- ABW:
-
Actual body weight
- ARDS:
-
Acute respiratory distress syndrome
- BMI:
-
Body mass index
- CPAP:
-
Continuous positive airway pressure
- DP:
-
Driving pressure
- EIT:
-
Electrical impedance tomography
- FiO2 :
-
Fraction of inspired oxygen
- ICU:
-
Intensive care unit
- IL:
-
Interleukin
- MP:
-
Mechanical power
- OLV:
-
One-lung ventilation
- PaCO2 :
-
Partial pressure of carbon dioxide
- Palv :
-
Alveolar pressure
- PaO2 :
-
Partial pressure of oxygen in arterial blood
- PBW:
-
Predicted body weight
- PCV:
-
Pressure-controlled ventilation
- PCV-VG:
-
Pressure-controlled volume guaranteed
- PEEP:
-
Positive end-expiratory pressure
- PPC:
-
Postoperative pulmonary complication
- Ppl :
-
Pleural pressure
- Ptp :
-
Transpulmonary pressure
- RM:
-
Recruitment maneuvers
- RR:
-
Respiratory rate
- SpO2 :
-
Peripheral oxygen saturation
- TV:
-
Tidal volume
- VCV:
-
Volume-controlled ventilation
- VILI:
-
Ventilator-induced lung injury
- WBC:
-
White blood cell
References
Walter K. Mechanical Ventilation. JAMA. 2021;326(14):1452. https://doi.org/10.1001/jama.2021.13084.
Adam EH, Funke M, Zacharowski K, Meybohm P, Keller H, Weber CF. Impact of Intraoperative Cell Salvage on Blood Coagulation Factor Concentrations in Patients Undergoing Cardiac Surgery. Anesth Analg. 2020;130(5):1389–95. https://doi.org/10.1213/ANE.0000000000004693.
Slutsky AS, Ranieri VM. Ventilator-induced lung injury. N Engl J Med. 2013;369(22):2126–36. https://doi.org/10.1056/NEJMra1208707.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–49. https://doi.org/10.3322/caac.21660.
Serpa Neto A, Hemmes SN, Barbas CS, Beiderlinden M, Fernandez-Bustamante A, Futier E, et al. Incidence of mortality and morbidity related to postoperative lung injury in patients who have undergone abdominal or thoracic surgery: a systematic review and meta-analysis. Lancet Respir Med. 2014;2(12):1007–15. https://doi.org/10.1016/s2213-2600(14)70228-0.
Cai L, Li Y, Sun L, Yang XW, Wang WB, Feng F, et al. Better perioperative outcomes in thoracoscopic-esophagectomy with two-lung ventilation in semi-prone position. J Thorac Dis. 2017;9(1):117–22. https://doi.org/10.21037/jtd.2017.01.27.
Fernandez-Bustamante A, Frendl G, Sprung J, Kor DJ, Subramaniam B, Martinez Ruiz R, et al. Postoperative Pulmonary Complications, Early Mortality, and Hospital Stay Following Noncardiothoracic Surgery: A Multicenter Study by the Perioperative Research Network Investigators. JAMA Surg. 2017;152(2):157–66. https://doi.org/10.1001/jamasurg.2016.4065.
Cattaneo SM, Park BJ, Wilton AS, Seshan VE, Bains MS, Downey RJ, et al. Use of video-assisted thoracic surgery for lobectomy in the elderly results in fewer complications. Ann Thorac Surg. 2008;85(1):231–5; discussion 235–6. https://doi.org/10.1016/j.athoracsur.2007.07.080.
Gao S, Zhang Z, Brunelli A, Chen C, Chen C, Chen G, et al. The Society for Translational Medicine: clinical practice guidelines for mechanical ventilation management for patients undergoing lobectomy. J Thorac Dis. 2017;9(9):3246–54. https://doi.org/10.21037/jtd.2017.08.166.
Pereira SM, Tucci MR, Morais CCA, Simões CM, Tonelotto BFF, Pompeo MS, et al. Individual Positive End-expiratory Pressure Settings Optimize Intraoperative Mechanical Ventilation and Reduce Postoperative Atelectasis. Anesthesiology. 2018;129(6):1070–81. https://doi.org/10.1097/aln.0000000000002435.
Meara JG, Leather AJ, Hagander L, Alkire BC, Alonso N, Ameh EA, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386(9993):569–624. https://doi.org/10.1016/s0140-6736(15)60160-x.
Canet J, Gallart L, Gomar C, Paluzie G, Vallès J, Castillo J, et al. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology. 2010;113(6):1338–50. https://doi.org/10.1097/ALN.0b013e3181fc6e0a.
Arozullah AM, Daley J, Henderson WG, Khuri SF. Multifactorial risk index for predicting postoperative respiratory failure in men after major noncardiac surgery. The National Veterans Administration Surgical Quality Improvement Program. Ann Surg. 2000;232(2):242–53. https://doi.org/10.1097/00000658-200008000-00015.
Ferreyra GP, Baussano I, Squadrone V, Richiardi L, Marchiaro G, Del Sorbo L, et al. Continuous positive airway pressure for treatment of respiratory complications after abdominal surgery: a systematic review and meta-analysis. Ann Surg. 2008;247(4):617–26. https://doi.org/10.1097/SLA.0b013e3181675829.
Fagevik Olsén M, Hahn I, Nordgren S, Lönroth H, Lundholm K. Randomized controlled trial of prophylactic chest physiotherapy in major abdominal surgery. Br J Surg. 1997;84(11):1535–8. https://doi.org/10.1111/j.1365-2168.1997.02828.x.
Agostini P, Naidu B, Cieslik H, Rathinam S, Bishay E, Kalkat MS, et al. Comparison of recognition tools for postoperative pulmonary complications following thoracotomy. Physiotherapy. 2011;97(4):278–83. https://doi.org/10.1016/j.physio.2010.11.007.
Jammer I, Wickboldt N, Sander M, Smith A, Schultz MJ, Pelosi P, et al. Standards for definitions and use of outcome measures for clinical effectiveness research in perioperative medicine: European Perioperative Clinical Outcome (EPCO) definitions: a statement from the ESA-ESICM joint taskforce on perioperative outcome measures. Eur J Anaesthesiol. 2015;32(2):88–105. https://doi.org/10.1097/eja.0000000000000118.
Reeve JC, Nicol K, Stiller K, McPherson KM, Denehy L. Does physiotherapy reduce the incidence of postoperative complications in patients following pulmonary resection via thoracotomy? a protocol for a randomised controlled trial. J Cardiothorac Surg. 2008;3:48. https://doi.org/10.1186/1749-8090-3-48.
LAS VEGAS investigators. Epidemiology, practice of ventilation and outcome for patients at increased risk of postoperative pulmonary complications: LAS VEGAS - an observational study in 29 countries. Eur J Anaesthesiol. 2017;34(8):492–507. https://doi.org/10.1097/eja.0000000000000646.
O’Gara B, Talmor D. Perioperative lung protective ventilation. BMJ. 2018;362:k3030. https://doi.org/10.1136/bmj.k3030.
Güldner A, Kiss T, Serpa Neto A, Hemmes SN, Canet J, Spieth PM, et al. Intraoperative protective mechanical ventilation for prevention of postoperative pulmonary complications: a comprehensive review of the role of tidal volume, positive end-expiratory pressure, and lung recruitment maneuvers. Anesthesiology. 2015;123(3):692–713. https://doi.org/10.1097/aln.0000000000000754.
Marcy T. Barotrauma: detection, recognition, and management. Chest. 1993;104(2):578–84. https://doi.org/10.1378/chest.104.2.578.
Hamilton-Farrell M, Bhattacharyya A. Barotrauma. Injury. 2004;35(4):359–70. https://doi.org/10.1016/j.injury.2003.08.020.
Hubmayr R, Kallet R. Understanding Pulmonary Stress-Strain Relationships in Severe ARDS and Its Implications for Designing a Safer Approach to Setting the Ventilator. Respir Care. 2018;63(2):219–26. https://doi.org/10.4187/respcare.05900.
Beitler JR, Malhotra A, Thompson BT. Ventilator-induced Lung Injury. Clin Chest Med. 2016;37(4):633–46. https://doi.org/10.1016/j.ccm.2016.07.004.
Dreyfuss D, Saumon G. Barotrauma is volutrauma, but which volume is the one responsible? Intensive Care Med. 1992;18(3):139–41. https://doi.org/10.1007/bf01709236.
Gattinoni L, Quintel M, Marini JJ. Volutrauma and atelectrauma: which is worse? Crit Care. 2018;22(1):264. https://doi.org/10.1186/s13054-018-2199-2.
Mead J, Takishima T, Leith D. Stress distribution in lungs: a model of pulmonary elasticity. J Appl Physiol. 1970;28(5):596–608. https://doi.org/10.1152/jappl.1970.28.5.596.
Slutsky AS. Lung injury caused by mechanical ventilation. Chest. 1999;116(1 Suppl):9s–15s. https://doi.org/10.1378/chest.116.suppl_1.9s-a.
Kawano T, Mori S, Cybulsky M, Burger R, Ballin A, Cutz E, et al. Effect of granulocyte depletion in a ventilated surfactant-depleted lung. J Appl Physiol (1985). 1987;62(1):27–33. https://doi.org/10.1152/jappl.1987.62.1.27.
Tremblay LN, Slutsky AS. Ventilator-induced injury: from barotrauma to biotrauma. Proc Assoc Am Physicians. 1998;110(6):482–8.
Chen L, Xia HF, Shang Y, Yao SL. Molecular Mechanisms of Ventilator-Induced Lung Injury. Chin Med J (Engl). 2018;131(10):1225–31. https://doi.org/10.4103/0366-6999.226840.
Futier E, Constantin JM, Paugam-Burtz C, Pascal J, Eurin M, Neuschwander A, et al. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med. 2013;369(5):428–37. https://doi.org/10.1056/NEJMoa1301082.
Karalapillai D, Weinberg L, Peyton P, Ellard L, Hu R, Pearce B, et al. Effect of Intraoperative Low Tidal Volume vs Conventional Tidal Volume on Postoperative Pulmonary Complications in Patients Undergoing Major Surgery: A Randomized Clinical Trial. JAMA. 2020;324(9):848–58. https://doi.org/10.1001/jama.2020.12866.
Amato MB, Meade MO, Slutsky AS, Brochard L, Costa EL, Schoenfeld DA, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med. 2015;372(8):747–55. https://doi.org/10.1056/NEJMsa1410639.
Hemmes SN, de GamaAbreu M, Pelosi P, Schultz MJ. High versus low positive end-expiratory pressure during general anaesthesia for open abdominal surgery (PROVHILO trial): a multicentre randomised controlled trial. Lancet. 2014;384(9942):495–503. https://doi.org/10.1016/s0140-6736(14)60416-5.
Downs JB. Is supplemental oxygen necessary? J Cardiothorac Vasc Anesth. 2006;20(2):133–5. https://doi.org/10.1053/j.jvca.2006.01.009.
Duggan M, Kavanagh BP. Pulmonary atelectasis: a pathogenic perioperative entity. Anesthesiology. 2005;102(4):838–54. https://doi.org/10.1097/00000542-200504000-00021.
Neto AS, Hemmes SN, Barbas CS, Beiderlinden M, Fernandez-Bustamante A, Futier E, et al. Association between driving pressure and development of postoperative pulmonary complications in patients undergoing mechanical ventilation for general anaesthesia: a meta-analysis of individual patient data. Lancet Respir Med. 2016;4(4):272–80. https://doi.org/10.1016/s2213-2600(16)00057-6.
Nestler C, Simon P, Petroff D, Hammermüller S, Kamrath D, Wolf S, et al. Individualized positive end-expiratory pressure in obese patients during general anaesthesia: a randomized controlled clinical trial using electrical impedance tomography. Br J Anaesth. 2017;119(6):1194–205. https://doi.org/10.1093/bja/aex192.
Writing Committee for the PROBESE Collaborative Group of the PROtective VEntilation Network (PROVEnet) for the Clinical Trial Network of the European Society of Anaesthesiology; Bluth T, Serpa Neto A, Schultz MJ, Pelosi P, Gama de Abreu M; PROBESE Collaborative Group, et al. Effect of Intraoperative High Positive End-Expiratory Pressure (PEEP) With Recruitment Maneuvers vs Low PEEP on Postoperative Pulmonary Complications in Obese Patients: A Randomized Clinical Trial. JAMA. 2019;321(23):2292–305. https://doi.org/10.1001/jama.2019.7505.
Costa Leme A, Hajjar LA, Volpe MS, Fukushima JT, De Santis Santiago RR, Osawa EA, et al. Effect of Intensive vs Moderate Alveolar Recruitment Strategies Added to Lung-Protective Ventilation on Postoperative Pulmonary Complications: A Randomized Clinical Trial. JAMA. 2017;317(14):1422–32. https://doi.org/10.1001/jama.2017.2297.
Ferrando C, Suarez-Sipmann F, Tusman G, León I, Romero E, Gracia E, et al. Open lung approach versus standard protective strategies: Effects on driving pressure and ventilatory efficiency during anesthesia - A pilot, randomized controlled trial. PLoS ONE. 2017;12(5):e0177399. https://doi.org/10.1371/journal.pone.0177399.
Defresne AA, Hans GA, Goffin PJ, Bindelle SP, Amabili PJ, DeRoover AM, et al. Recruitment of lung volume during surgery neither affects the postoperative spirometry nor the risk of hypoxaemia after laparoscopic gastric bypass in morbidly obese patients: a randomized controlled study. Br J Anaesth. 2014;113(3):501–7. https://doi.org/10.1093/bja/aeu101.
Hodgson CL, Cooper DJ, Arabi Y, King V, Bersten A, Bihari S, et al. Maximal Recruitment Open Lung Ventilation in Acute Respiratory Distress Syndrome (PHARLAP). A Phase II, Multicenter Randomized Controlled Clinical Trial. Am J Respir Crit Care Med. 2019;200(11):1363–72. https://doi.org/10.1164/rccm.201901-0109OC.
Park M, Yoon S, Nam JS, Ahn HJ, Kim H, Kim HJ, et al. Driving pressure-guided ventilation and postoperative pulmonary complications in thoracic surgery: a multicentre randomised clinical trial. Br J Anaesth. 2023;130(1):e106–18. https://doi.org/10.1016/j.bja.2022.06.037.
Detillon D, Veen EJ. Postoperative Outcome After Pulmonary Surgery for Non-Small Cell Lung Cancer in Elderly Patients. Ann Thorac Surg. 2018;105(1):287–93. https://doi.org/10.1016/j.athoracsur.2017.07.032.
Linares-Perdomo O, East TD, Brower R, Morris AH. Standardizing Predicted Body Weight Equations for Mechanical Ventilation Tidal Volume Settings. Chest. 2015;148(1):73–8. https://doi.org/10.1378/chest.14-2843.
Peel JK, Funk DJ, Slinger P, Srinathan S, Kidane B. Tidal volume during 1-lung ventilation: A systematic review and meta-analysis. J Thorac Cardiovasc Surg. 2022;163(4):1573–1585.e1. https://doi.org/10.1016/j.jtcvs.2020.12.054.
Colquhoun DA, Leis AM, Shanks AM, Mathis MR, Naik BI, Durieux ME, et al. A Lower Tidal Volume Regimen during One-lung Ventilation for Lung Resection Surgery Is Not Associated with Reduced Postoperative Pulmonary Complications. Anesthesiology. 2021;134(4):562–76. https://doi.org/10.1097/aln.0000000000003729.
Park JY. Permissive hypercarbia and managing arterial oxygenation during one-lung ventilation. Korean J Anesthesiol. 2020;73(6):469–70. https://doi.org/10.4097/kja.20597.
Wang H, He H. Dynamic hyperinflation and intrinsic PEEP in ARDS patients: who, when, and how needs more focus? Crit Care. 2019;23(1):422. https://doi.org/10.1186/s13054-019-2713-1.
Rozé H, Lafargue M, Batoz H, Picat MQ, Perez P, Ouattara A, et al. Pressure-controlled ventilation and intrabronchial pressure during one-lung ventilation. Br J Anaesth. 2010;105(3):377–81. https://doi.org/10.1093/bja/aeq130.
Yao W, Yang M, Cheng Q, Shan S, Yang B, Han Q, et al. Effect of Pressure-Controlled Ventilation-Volume Guaranteed on One-Lung Ventilation in Elderly Patients Undergoing Thoracotomy. Med Sci Monit. 2020;26:e921417. https://doi.org/10.12659/msm.921417.
Li XF, Jin L, Yang JM, Luo QS, Liu HM, Yu H. Effect of ventilation mode on postoperative pulmonary complications following lung resection surgery: a randomised controlled trial. Anaesthesia. 2022;77(11):1219–27. https://doi.org/10.1111/anae.15848.
McKown AC, Semler MW, Rice TW. Best PEEP trials are dependent on tidal volume. Crit Care. 2018;22(1):115. https://doi.org/10.1186/s13054-018-2047-4.
Sahetya SK, Goligher EC, Brower RG. Fifty Years of Research in ARDS. Setting Positive End-Expiratory Pressure in Acute Respiratory Distress Syndrome. Am J Respir Crit Care Med. 2017;195(11):1429–38. https://doi.org/10.1164/rccm.201610-2035CI.
Park M, Ahn HJ, Kim JA, Yang M, Heo BY, Choi JW, et al. Driving Pressure during Thoracic Surgery: A Randomized Clinical Trial. Anesthesiology. 2019;130(3):385–93. https://doi.org/10.1097/aln.0000000000002600.
Paudel R, Trinkle CA, Waters CM, Robinson LE, Cassity E, Sturgill JL, et al. Mechanical Power: A New Concept in Mechanical Ventilation. Am J Med Sci. 2021;362(6):537–45. https://doi.org/10.1016/j.amjms.2021.09.004.
Cressoni M, Gotti M, Chiurazzi C, Massari D, Algieri I, Amini M, et al. Mechanical Power and Development of Ventilator-induced Lung Injury. Anesthesiology. 2016;124(5):1100–8. https://doi.org/10.1097/aln.0000000000001056.
Santos RS, Maia LA, Oliveira MV, Santos CL, Moraes L, Pinto EF, et al. Biologic Impact of Mechanical Power at High and Low Tidal Volumes in Experimental Mild Acute Respiratory Distress Syndrome. Anesthesiology. 2018;128(6):1193–206. https://doi.org/10.1097/aln.0000000000002143.
Maia LA, Samary CS, Oliveira MV, Santos CL, Huhle R, Capelozzi VL, et al. Impact of Different Ventilation Strategies on Driving Pressure, Mechanical Power, and Biological Markers During Open Abdominal Surgery in Rats. Anesth Analg. 2017;125(4):1364–74. https://doi.org/10.1213/ane.0000000000002348.
Serpa Neto A, Deliberato RO, Johnson AEW, Bos LD, Amorim P, Pereira SM, et al. Mechanical power of ventilation is associated with mortality in critically ill patients: an analysis of patients in two observational cohorts. Intensive Care Med. 2018;44(11):1914–22. https://doi.org/10.1007/s00134-018-5375-6.
Gattinoni L, Tonetti T, Cressoni M, Cadringher P, Herrmann P, Moerer O, et al. Ventilator-related causes of lung injury: the mechanical power. Intensive Care Med. 2016;42(10):1567–75. https://doi.org/10.1007/s00134-016-4505-2.
Gattinoni L, Tonetti T, Quintel M. Intensive care medicine in 2050: ventilator-induced lung injury. Intensive Care Med. 2018;44(1):76–8. https://doi.org/10.1007/s00134-017-4770-8.
Chiumello D, Gotti M, Guanziroli M, Formenti P, Umbrello M, Pasticci I, et al. Bedside calculation of mechanical power during volume- and pressure-controlled mechanical ventilation. Crit Care. 2020;24(1):417. https://doi.org/10.1186/s13054-020-03116-w.
Carramiñana A, Ferrando C, Unzueta MC, Navarro R, Suárez-Sipmann F, Tusman G, et al. Rationale and Study Design for an Individualized Perioperative Open Lung Ventilatory Strategy in Patients on One-Lung Ventilation (iPROVE-OLV). J Cardiothorac Vasc Anesth. 2019;33(9):2492–502. https://doi.org/10.1053/j.jvca.2019.01.056.
Liu K, Huang C, Xu M, Wu J, Frerichs I, Moeller K, et al. PEEP guided by electrical impedance tomography during one-lung ventilation in elderly patients undergoing thoracoscopic surgery. Ann Transl Med. 2019;7(23):757. https://doi.org/10.21037/atm.2019.11.95.
Sella N, Pettenuzzo T, Zarantonello F, Andreatta G, De Cassai A, Schiavolin C, et al. Electrical impedance tomography: A compass for the safe route to optimal PEEP. Respir Med. 2021;187:106555. https://doi.org/10.1016/j.rmed.2021.106555.
Zhao Z, Wang W, Zhang Z, Xu M, Frerichs I, Wu J, et al. Influence of tidal volume and positive end-expiratory pressure on ventilation distribution and oxygenation during one-lung ventilation. Physiol Meas. 2018;39(3):034003. https://doi.org/10.1088/1361-6579/aaaeb2.
Duggan M, Kavanagh BP. Atelectasis in the perioperative patient. Curr Opin Anaesthesiol. 2007;20(1):37–42. https://doi.org/10.1097/ACO.0b013e328011d7e5.
Peel JK, Funk DJ, Slinger P, Srinathan S, Kidane B. Positive end-expiratory pressure and recruitment maneuvers during one-lung ventilation: A systematic review and meta-analysis. J Thorac Cardiovasc Surg. 2020;160(4):1112–1122.e3. https://doi.org/10.1016/j.jtcvs.2020.02.077.
Fan E, Wilcox ME, Brower RG, Stewart TE, Mehta S, Lapinsky SE, et al. Recruitment maneuvers for acute lung injury: a systematic review. Am J Respir Crit Care Med. 2008;178(11):1156–63. https://doi.org/10.1164/rccm.200802-335OC.
Jonkman AH, Ranieri VM, Brochard L. Lung recruitment. Intensive Care Med. 2022;48(7):936–8. https://doi.org/10.1007/s00134-022-06715-z.
Suzumura EA, Amato MBP, Cavalcanti AB. Understanding recruitment maneuvers. Intensive Care Med. 2016;42(5):908–11. https://doi.org/10.1007/s00134-015-4025-5.
Silva PL, Moraes L, Santos RS, Samary C, Ornellas DS, Maron-Gutierrez T, et al. Impact of pressure profile and duration of recruitment maneuvers on morphofunctional and biochemical variables in experimental lung injury. Crit Care Med. 2011;39(5):1074–81. https://doi.org/10.1097/CCM.0b013e318206d69a.
Sticher J, Junger A, Hartmann B, Benson M, Jost A, Golinski M, et al. Computerize anesthesia record keeping in thoracic surgery–suitability of electronic anesthesia records in evaluating predictors for hypoxemia during one-lung ventilation. J Clin Monit Comput. 2002;17(6):335–43. https://doi.org/10.1023/a:1024294700397.
Ku CM, Slinger P, Waddell TK. A novel method of treating hypoxemia during one-lung ventilation for thoracoscopic surgery. J Cardiothorac Vasc Anesth. 2009;23(6):850–2. https://doi.org/10.1053/j.jvca.2008.12.024.
Russell WJ. Intermittent positive airway pressure to manage hypoxia during one-lung anaesthesia. Anaesth Intensive Care. 2009;37(3):432–4. https://doi.org/10.1177/0310057x0903700316.
Young CC, Harris EM, Vacchiano C, Bodnar S, Bukowy B, Elliott RRD, et al. Lung-protective ventilation for the surgical patient: international expert panel-based consensus recommendations. Br J Anaesth. 2019;123(6):898–913. https://doi.org/10.1016/j.bja.2019.08.017.
Pelosi P, Ball L, Barbas CSV, Bellomo R, Burns KEA, Einav S, et al. Personalized mechanical ventilation in acute respiratory distress syndrome. Crit Care. 2021;25(1):250. https://doi.org/10.1186/s13054-021-03686-3.
Kiss T, Wittenstein J, Becker C, Birr K, Cinnella G, Cohen E, et al. Protective ventilation with high versus low positive endexpiratory pressure during one-lung ventilation for thoracic surgery (PROTHOR): study protocol for a randomized controlled trial. Trials. 2019;20(1):213. Erratum in: Trials. 2019;20(1):259. https://doi.org/10.1186/s13063-019-3208-8.
Acknowledgements
Not applicable.
Funding
This work was supported by the Clinical Research Plan of SHDC (SHDC2020CR4063), Shanghai Medical Innovation Research Program "Science and Technology Innovation Action Plan" 2022 (22Y11901800) and National Natural Science Foundation of China (82202412).
Author information
Authors and Affiliations
Contributions
Jingxiang Wu: This author raised the idea and established the framework of the manuscript. Yuanyuan Zou and Zhiyun Liu: These authors drafted the manuscript. Jingxiang Wu and Qing Miao: These authors revised the manuscript and edited critically. All the authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors gave their content for publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zou, Y., Liu, Z., Miao, Q. et al. A review of intraoperative protective ventilation. APS 2, 10 (2024). https://doi.org/10.1007/s44254-023-00048-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44254-023-00048-w