Abstract
Bilateral superficial cervical plexus block (BSCPB) is widely used in thyroid surgery. However, its ability to reduce patients’ perioperative pain remains controversial. Therefore, this study aimed to investigate the value of using BSCPB perioperatively for thyroid surgery by conducting a systematic review and meta-analysis of relevant clinical studies. In this systematic review and meta-analysis, we conducted comprehensive searches in the PubMed, Embase, and Cochrane Library databases to collect all randomized controlled trials (RCTs) that used BSCPB for thyroid surgery. The included studies were then analyzed for heterogeneity using the chi-square test, and studies with large heterogeneity were subjected to subgroup or sensitivity analyses. Treatment effects were measured using odds ratio (OR) or weighted mean difference (WMD) and 95% confidence interval (CI). A total of 19 RCTs with 1,365 patients who underwent thyroid surgery (713 and 652 patients in the BSCPB and control groups, respectively) were included in this systematic review. Most of the studies reported that cervical plexus blocks were used preoperatively, and the main drugs used were 0.25–0.75% ropivacaine or bupivacaine. The BSCPB procedure could significantly reduce visual analog scale scores in the immediate (WMD: −1.12, 95% CI: −1.51 to −0.73, P < 0.00001), 6-h (WMD: −1.06, 95% CI: −1.60 to −0.53, P = 0.0001) and 24-h (WMD: −0.87, 95% CI: −1.29 to −0.45, P < 0.0001) postoperative period and also reduce opioid requirements for patients in the post-anesthesia care unit (50.99% vs 72.92%, OR: 0.3, 95% CI: 0.17 to 0.52, P < 0.0001) and in the wards (39.80% vs 59.79%, OR: 0.27, 95% CI: 0.12 to 0.59, P = 0.001). Additionally, BSCPB reduced the incidence of postoperative nausea and vomiting (OR: 0.50, 95% CI: 0.29 to 0.87, P = 0.01). Due to the large heterogeneity, the results only suggest decrease use of intraoperative fentanyl and postoperative morphine in the BSCPB group. The use of BSCPB alleviates of postoperative pain, opioid requirement, and reduces incidence of postoperative nausea and vomiting in patients who have undergone thyroid surgery. More clinical studies are needed for further conclusions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Thyroid disorders (e.g., goiter and thyroid cancer) are becoming more prevalent worldwide, and partial or total thyroidectomy are the main recommended treatment methods [1]. Although the duration needed for thyroidectomy is relatively short, patients still experience moderate pain and discomfort (including incision site pain, posterior neck pain, and occipital headache), and approximately 93% of patients require analgesia equivalent to at least 20 mg oral morphine for postoperative relief [2]. Medications such as oral non-steroidal anti-inflammatory drugs and morphine are commonly used for pain relief, but the use of opioids in wards may trigger side effects such as drowsiness, respiratory depression, nausea, and vomiting, which are detrimental to recovery post-thyroid surgery. Projectile vomiting events may cause dislodgement of the neck sutures [3], and respiratory depression is potentially the most serious complication after thyroid surgery and can also be fatal.
In recent years, multimodal analgesia has played an important role in reducing postoperative opioid doses and its associated side effects [4]. Analgesia with nerve blocks is emerging as the main method of postoperative analgesia due to its precise effect and low systemic toxicity. Bilateral superficial cervical plexus block (BSCPB) can block several plexuses innervating the neck (the lesser occipital nerve, great auricular nerve, transverse cervical nerve, and supraclavicular nerve) and is widely used as an adjunctive analgesia method in neck surgery [5]. The cervical plexus comprises anterior branches from the C1 to C4 segments, with the anterior branch at the C5 segment involved sometimes. The cervical plexus is located deep to the sternocleidomastoid muscle and anterior to the middle scalene muscles and levator scapulae. There are superficial and deep branches in the cervical plexus. The superficial cervical plexus emerges around the middle of the posterior border of the sternocleidomastoid muscle and travels radially upward, anteriorly, and inferiorly, sending out lesser occipital, great auricular, transverse cervical, and supraclavicular branches to the skin of the occiput, behind the ears, front of the neck, shoulders, and upper chest, respectively. The superficial cervical plexus is located superficially and has a clear body surface localization (midpoint of the posterior border of the sternocleidomastoid muscle). Thus, the primary anesthesiologist can also perform the block quickly using body surface location or ultrasound localization [6]. Local anesthetic can be injected between the sternocleidomastoid muscle and prevertebral fascia to block the superficial cervical plexus [7]. In recent years, several randomized controlled trials (RCTs) have reported the use of superficial cervical plexus blocks in the perioperative anesthetic management of thyroid surgery [8-12]. However, there have been some controversial findings about whether the procedure can reduce postoperative pain and complications in patients. Given that most RCTs are single-center, small sample studies, the conclusions are yet to be confirmed.
Therefore, this study aimed to assess the efficiency, safety, and potential advantages of BSCPB in thyroid surgery by conducting a systematic review and meta-analysis of relevant clinical studies in the literature.
2 Materials and methods
In this systematic review, meta-analyses were performed in strict accordance with the criteria stated in PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analysis, PRISMA) [13]. The protocols retrieved for this study were registered on the PROSPERO platform (registration number CRD42022309503).
2.1 Literature search
A computerized search in the PubMed, Embase, Cochrane Library databases was conducted to collect data on clinical studies involving the use of BSCPB as anesthesia in thyroid surgery. The timeframe used for the search was from the establishment of the database until December 30, 2022, and the search was limited to studies in English. The search was conducted using subject terms, with the search title/abstract containing a combination of the terms “cervical plexus,” “cervical plexus block,” “thyroidectomy,” and “thyroid surgery”. And the complete search strategy in PubMed is as follows: (thyro*[Title/Abstract]) AND ((cervical plexus block[Title/Abstract]) OR (cervical plexus[Title/Abstract])) (see Supplemental Table 1 for search protocol). To broaden the search, further computerized or manual reviews of all the retrieved review articles and citations in conference abstracts were performed. After the search protocol was jointly determined by all the research staff, the literature search was then completed by a single designated searcher (Author Y.C.).
2.2 Screening criteria
All the literature from the initial search was exported to the Endnote management software (Version. 9). The inclusion criteria for this study were as follows: 1) RCTs, 2) studies involving participants who underwent thyroid surgery, 3) studies involving a BSCPB group versus a control group using saline/no block, and 4) studies including the inclusion of at least one outcome indicator involving patient prognosis. The exclusion criteria were as follows: 1) duplicate or suspected duplicate studies; 2) editorials, letters to editors, review papers, and case reports; and 3) studies with incomplete study data; 4) patients who have history of analgesic administration within 4 weeks before surgery or have chronic pain in the last three months; and 5) Literature not in English.
2.3 Data extraction and outcome indicators
Two researchers (Authors Y.C. and H.S.) independently screened the literature, extracted information, and performed cross-checking. Any disagreements were resolved through discussion or consultation with a third party (Author L.N.). The literature was screened by first reading the title of the study and then by excluding clearly irrelevant literature. The abstract and full text were then read to determine their inclusion. If needed, the original study authors were contacted by email and telephone to obtain information that was not identified but deemed important to the study. The general information extracted included basic data about the included studies such as (1) the first author and time of publication; (2) baseline characteristics of the study population, including sample size, type of study, and procedures performed; (3) number of cases in each study case group versus control group; (4) key elements of the risk of bias assessment; and (5) outcome indicators and outcome measures of interest, with key indicators including postoperative pain status using the visual analog scale (VAS), postoperative analgesia use, incidence of postoperative nausea and vomiting, time to first postoperative rescue analgesia, and dose of intraoperative fentanyl and postoperative morphine administered within 24 h.
2.4 Risk of bias assessment
Risk of bias assessments were performed independently by two investigators (Authors Y.C. and H.L.), and any disagreement was resolved through discussion or consultation with a third party (Author Y.Z.). The included RCTs were evaluated using Cochrane Collaboration (RevMan 5.3 software) according to the following criteria [27]: method of randomization, allocation concealment, blinding (study subjects, study researchers, and personnel who measured study outcomes), completeness of outcome data, selective reporting of study results, and other possible biases. For each study, the six items mentioned above were judged as “low risk of bias”, “high risk of bias”, or “unclear risk” (lack of relevant information or uncertain bias).
2.5 Evaluation of literature quality
Quality assessment was performed independently by two investigators (Authors Y.C. and L.N) and disagreements, if any, were resolved through discussion or consultation with a third party (Author Q.L.). Each included study was evaluated using the Jadad scale [28], with scores assigned for random sequence generation, blinding, withdrawals, and lost to follow-up. The total score ranged from 0 to 5, with scores of 0–2 indicating low quality and 3–5 indicating high quality.
2.6 Statistical analysis
Meta-analysis was performed using the RevMan 5.3 software (Revman, The Cochrane Collaboration, Oxford, UK), with odds ratio (OR) as an effect indicator for count data and mean difference (MD) as an effect indicator for measurement data; point estimates and 95% confidence interval (CI) were recorded for each effect. The data represented by the median and interquartile range were first converted to mean and standard deviation [29]. The heterogeneity of the included studies was analyzed using the χ2 test (test level α = 0.05) before combining effect sizes, and the magnitude of heterogeneity was determined by combining P values and I2 quantification. Because of the different surgeons, techniques and other conditions, the heterogeneity of the operation itself exists, a random-effects model was used [30]. Studies with significant clinical heterogeneity were subjected to a subgroup, sensitivity, or solely descriptive analysis. Subgroup analysis was performed for the primary outcomes according to (1) the type of local anesthetics; and (2) the measure of control group. Subgroup analysis was performed only if there were at least two studies in each subgroup. Sensitivity analysis was carried out by repeatedly excluding one trial at one time. The test level for the meta-analysis was α = 0.05.
3 Results
3.1 Search results
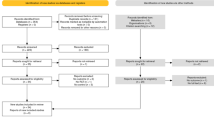
A total of 366 articles were retrieved, and 132 articles remained after deduplicating using Endnote 9.0. After detailed reading of the full text, a total of 18 articles that met the criteria of this study were included after excluding 112 articles for various reasons, including no control group (n = 1), ongoing trial (n = 65), grouping criteria not met (n = 3), incomplete data (n = 1), not in English (n = 1) and non-clinical nature (n = 42). The literature screening process is detailed in Fig. 1.
3.2 Characteristics of included studies
All the included studies were of high quality (Jadad score ≥ 3, Table 1), with a clear description of the study methods and a low overall risk of bias (Fig. 2). The 18 articles included were all RCTs, with a total of 1,265 patients (663 in the superficial cervical plexus block group and 602 in the control group). With the exception of two studies (Alexandre Herbland 2006, T. Steffen 2010), in which the superficial cervical plexus was used preoperatively and postoperatively. In most of the studies, superficial cervical plexus blocks were used preoperatively, and the main drugs used were 0.25–0.75% ropivacaine or bupivacaine, except for one study (G. Andrieu 2007), wherein clonidine was used as an adjuvant, as specified in Table 1. The method used for anesthesia in thyroid surgery was mostly combined intravenous–inhalation anesthesia, with the exception of three studies (Zemedu Aweke 2018, Yophtahe B. Woldegerima 2020, T. Steffen 2010), wherein the method used was unspecified. In addition, the findings of three studies revealed that the use of superficial cervical plexus block did not reduce the patients’ postoperative pain (Alexandre Herbland 2006, Ashraf A Moussa [8], Zeynep Eti 2006), whereas the findings of the remaining 17 studies revealed that the use of superficial cervical plexus block significantly reduced the patients’ postoperative pain.
3.3 Key outcome indicators
3.3.1 Postoperative visual analog scale (VAS) scores
All the studies that included postoperative VAS scores (score of 0–10) were included in the analysis, and four time points were identified for the analysis. Three or more studies satisfied the mentioned time points: immediate (Fig. 3A), 6-h (Fig. 3B), 12-h (Fig. 3C), and 24-h (Fig. 3D) postoperative time points. The results showed that patients in the superficial cervical plexus block group were more likely to have lower VAS scores in the immediate postoperative [weighted mean difference (WMD): −1.1, 95% CI: −1.76 to −0.74, P < 0.00001], 6-h postoperative (WMD: −1.06, 95% CI: −1.60 to −0.53, P < 0.0001) and 24-h postoperative (WMD: −0.87, 95% CI: −1.29 to −0.45, P < 0.0001) time points than patients in the control group. Although patients in the superficial cervical plexus block group had lower VAS scores at the 12-h postoperative time points than those in the control group, there was no statistically significant differences (P > 0.05) (Fig. 3).
3.3.2 Postoperative nausea and vomiting
Overall, 12 studies (866 patients) reported the incidence of postoperative nausea and vomiting in patients after thyroid surgery and found that the use of superficial cervical plexus block reduced the incidence of postoperative nausea and vomiting (OR: 0.50, 95% CI: 0.29 to 0.87, P = 0.01) (Fig. 4A). Results of subgroup analysis based on the type of local anesthetics used showed that the incidence of postoperative nausea and vomiting was lower in the bupivacaine group compared to the control group (OR: 0.42, 95% CI: 0.20 to 0.88, P= 0.02), the ropivacaine group (OR: 0.61, 95% CI: 0.24 to 1.55, P = 0.3) (Fig. 4B). The subgroup analysis based in the measures of control group performed showed that there is no statistically significant difference in postoperative nausea and vomiting in the ESPB group compared with control group in patients who received saline (OR: 0.57, 95% CI: 0.30 to 1.09, P = 0.09) or no block (OR: 0.32, 95% CI: 0.09 to 1.13, P = 0.08) as control (Fig. 4C).
3.4 Secondary outcome indicators
3.4.1 Time to first need of postoperative analgesia
Three studies reported the time to first postoperative rescue analgesia required by patients. All the three studies showed that patients in the superficial cervical plexus block group took a longer time before needing their first postoperative rescue analgesia; however, the overall mean effect was not significantly different between the groups (WMD: 9.27, 95% CI: −8.67 to 27.22, P = 0.31) (Table 2).
3.4.2 Requirement of postoperative analgesia
We compared the rate of postoperative opioid requirement for patients in the post-anesthesia care unit (PACU) and in the wards with the rate of non-opioid requirement for patients in the wards. The results showed that the use of superficial cervical plexus block significantly reduced the postoperative opioid requirement for patients in the PACU (OR: 0.3, 95% CI: 0.17 to 0.52, P < 0.0001) and wards (OR: 0.27, 95% CI: 0.12 to 0.59, P = 0.001) but did not reduce the non-opioid requirement for patients in the wards (OR: 0.34, 95% CI: 0.08 to 1.39, P = 0.13) (Table 2).
3.4.3 Intraoperative fentanyl and postoperative morphine dosage
A total of 5 studies (277 patients) recorded the intraoperative fentanyl dosage, and the results suggested that the superficial cervical plexus block reduced the intraoperative fentanyl dosage (WMD: -33.55, 95% CI: −53.54 to −13.55, P = 0.001, (Table 2)). However, due to the large heterogeneity among studies (I2 = 98%), further sensitivity analyses were conducted, and the results suggested that removal of any study did not reduce the heterogeneity. This was considered to be attributed to the different timings at which fentanyl was used in these studies. No subgroup analysis could be performed; hence, the results can only be used as a reference.
In addition, 5 studies (281 patients) recorded the use of morphine in the 24-h postoperative period, and the results suggested that the superficial cervical plexus block group showed reduced use of morphine in the 24-h postoperative period (WMD: −6.91, 95% CI: −11.43 to −2.39, P = 0.003, (Table 2)). However, the heterogeneity among studies was large (I2 = 90%), and a sensitivity analysis suggested that the same conclusion remained after removing the studies of Nathalie Dieudonne (2001) and Yusheng Yao (2019) (I2 = 0, WMD: −10.67, 95% CI [−13.23, −8.11]). After reviewing the original articles, this was considered to be attributed to the unclear route of morphine administration (Nathalie Dieudonne 2001) and indications for morphine use (Yusheng Yao 2019).
3.5 Publication bias and sensitivity analysis
A funnel plot of the results showed no obvious asymmetry (Fig. 5) and no publication bias, which has been confirmed with the application of Egger tests (P = 0.307). Sensitivity analysis was conducted by repeatedly removing one trial at a time and assessing if the P-value exceeded 0.05 in each case. There was no trial that significantly affected the last pooled results of outcomes.
4 Discussion
This systematic review included 18 RCTs with 1,265 patients who underwent thyroid surgery. We systematically analyzed the significance of using BSCPB in thyroid surgery and found that the use of BSCPB reduced VAS scores in patients who underwent thyroid surgery in the immediate, 6-h and 24-h postoperative period as well as reduced the incidence of postoperative nausea and vomiting, the need for postoperative antiemetics, the postoperative opioid dosage, and potentially the intraoperative opioid dosage. The study findings suggest the potential advantages of BSCPB in thyroid surgery.
At present, general anesthesia with endotracheal intubation (combined with or without cervical plexus nerve block) is the main method for anesthesia in thyroidectomy. BSCPB also has a long history of use in thyroid surgery as a simple and safe form of nerve block anesthesia, especially in underdeveloped areas where general anesthesia equipment is relatively limited, given that superficial cervical plexus block combined with deep cervical plexus block can even be used alone for some simple thyroidectomies [31, 32]. Regarding the value of BSCPB for perioperative analgesia in thyroid surgery, several previous studies have focused on whether BSCPB can reduce the intraoperative opioid doses, the short-term postoperative pain level and analgesia doses, and the incidence of postoperative nausea and vomiting as well as of other related complications. Our findings in the present study are consistent with those of the vast majority of RCTs [10, 11, 14, 15, 17-26] that suggest that the use of BSCPB reduced the intraoperative opioid dose, the pain VAS scores within the 24 h postoperative period, and the incidence of postoperative nausea and vomiting. However, a relatively smaller number of studies have suggested that the postoperative pain did not significantly reduce in the BSCPB group compared with the control group [7-9]. In addition, there is literature [16, 17, 25, 33] that suggests that BSCPB can reduce the incidence of postoperative nausea and vomiting, which may be related to lower intraoperative and postoperative opioid doses. However, there are also studies [11] that suggest that BSCPB does not reduce the incidence of postoperative nausea and vomiting. These controversial findings may be related to the study population that was included, the thyroid surgery subtypes, and the medications used to maintain anesthesia intraoperatively in these studies. Thus, a comprehensive analysis of the relevant results is required.
Meta-analyses addressing the value of BSCPB in thyroid surgery have also been performed previously. Among them, there was a meta-analysis published by Rene Warschkow et al. in 2012 [33] that included a total of eight RCTs. The results suggested that BSCPB combined with general anesthesia reduced pain VAS scores at 6 and 24 h after thyroid surgery, but the effect on pain reduction was too small to be clinically meaningful. Thus, this evidence, though relevant, could not be used to confirm the value of BSCPB in thyroid surgery. Subsequently, in a meta-analysis published by D. Mayhew et al. in 2018 [34], a total of 14 RCTs were included, and the results suggested that BSCPB could achieve early effective pain relief within 24 h after thyroid surgery and could shorten hospital stay, but it had no significant beneficial effect on the incidence of postoperative nausea and vomiting. Comparing the findings of previous studies and related reviews, the value of BSCPB in thyroid surgery still remains controversial. Hence, this study continues to search for and update relevant literature in the last 3 years based on the foundation provided by previous studies to explore the value of BSCPB in depth once again. In this study, we further refined the search terms and search protocol to potentially include more articles and excluded several studies that had relatively more missing data and incorporated no-treatment control groups. We assessed the risk of bias and the quality of the included articles and found that all the included studies were of high quality and had a low risk of bias.
Compared with the previous meta-analysis, we found that BSCPB could reduce the incidence of postoperative nausea and vomiting. This difference could have arisen because of the small number of studies only including 732 patients in the study by D. Mayhew et al. compared with our study; Another reason may be that they did not separate the use of preoperative or postoperative BSCPB. In term of the incidence of postoperative nausea and vomiting, our study contains 12 studies including 866 patients and we did not include those groups which use clonidine and postoperative BSCPB. Subgroup analysis demonstrates that there may be a benefit if the local anesthetics is bupivacaine, and ropivacaine appears to have no benefit over control. Both saline control and no block showed no significant difference comparing with BSCPB, and the heterogeneity was high in both subgroups (I2 > 50%). This was perhaps because that the reduction of sample size after subgrouping resulting in false negative results. Hence, these results need to be treated with caution. For the two outcomes with larger heterogeneity (intraoperative fentanyl and 24-h postoperative morphine use), the sensitivity analyses that were further conducted suggested that removing any study did not reduce the heterogeneity. Due to the small number of the included studies and the inability to perform subgroup analyses, the results still need to be further explored.
This study has some limitations. First, although the quality of the included articles was high, most of the studies were single-center, small sample size studies, which makes the findings debatable. Second, the differences in anesthesia delivery methods, BSCPB block methods, and postoperative management methods among the various articles limited further discussion of the results. Third, different time points for the collection of outcome indicators as well as the different methods and medications used for postoperative analgesia limited the integrated analysis of more outcomes, leading to less inclusion of certain outcome indicators present in the articles. Finally, for most of the included studies, we could only extract 2–3 postoperative patient outcome indicators; therefore, there were fewer pooled studies per outcome indicator in our results. However, most of the pooled analyses showed good robustness (I2 < 50%).
In summary, the overall number of included articles in each outcome indicator and sample size used in this study were small, and though the level of homogeneity present was favorable, the level of evidence was still low. Hence, the conclusions garnered are for reference only. In future relevant RCTs, the age profile of the population, thyroid surgery subtypes, and standardized intraoperative anesthesia methods should be more subdivided to allow the conclusions drawn to be relatively reliable.
Availability of data and materials
The datasets used or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BSCPB:
-
Bilateral superficial cervical plexus block
- RCTs:
-
Randomized controlled trials
- OR:
-
Odds ratio
- WMD:
-
Weighted mean difference
- CI:
-
Confidence interval
- VAS:
-
Visual analog scale
- MD:
-
Mean difference
References
Kim J, Gosnell JE, Roman SA. Geographic influences in the global rise of thyroid cancer. Nat Rev Endocrinol. 2020;16:17–29. https://doi.org/10.1038/s41574-019-0263-x.
Lou I, Chennell TB, Schaefer SC, Chen H, Sippel RS, Balentine C, et al. Optimizing outpatient pain management after thyroid and parathyroid surgery: a two-institution experience. Ann Surg Oncol. 2017;24:1951–7. https://doi.org/10.1245/s10434-017-5781-y.
Cho YJ, Choi GJ, Ahn EJ, Kang H. Pharmacologic interventions for postoperative nausea and vomiting after thyroidectomy: a systematic review and network meta-analysis. PLoS One. 2021;16:e0243865. https://doi.org/10.1371/journal.pone.0243865.
Uhlmann RA, Reinhart HA 3rd, Postevka E, Snyder SK, Romero AM. A review of postoperative pain management for thyroid and parathyroid surgery. J Surg Res. 2019;241:107–11. https://doi.org/10.1016/j.jss.2019.03.050.
Hoh SY, Doon YK, Chong SS, Ng KL. Randomized controlled trial comparing bilateral superficial cervical plexus block and local wound infiltration for pain control in thyroid surgery. Asian J Surg. 2019;42:1001–8. https://doi.org/10.1016/j.asjsur.2019.01.017.
Tran DQ, Dugani S, Finlayson RJ. A randomized comparison between ultrasound-guided and landmark-based superficial cervical plexus block. Reg Anesth Pain Med. 2010;35:539–43. https://doi.org/10.1097/AAP.0b013e3181faa11c.
Shao P, Li H, Shi R, Li J, Wang Y. Understanding fascial anatomy and interfascial communication: implications in regional anesthesia. J Anesth. 2022;36:554–63. https://doi.org/10.1007/s00540-022-03082-3.
Moussa AA. Bilateral superficial cervical plexus block alone or combined with bilateral deep cervical plexus block for pain management after thyroid surgery. Alexandria J Anaesthesia Intensive Care. 2006;9(2):45–50.
Eti Z, Irmak P, Gulluoglu BM, Manukyan MN, Gogus FY. Does bilateral superficial cervical plexus block decrease analgesic requirement after thyroid surgery? Anesth Analg. 2006;102:1174–6. https://doi.org/10.1213/01.ane.0000202383.51830.c4.
Xing J, Wu R, Liang L, Fang H, Chen L, Luo C. Comparison of the analgesic effects of intravenous infusion of Dexmedetomidine versus bilateral superficial cervical plexus block after thyroidectomy: a randomized controlled trial. Clin J Pain. 2021;37:623–8. https://doi.org/10.1097/AJP.0000000000000954.
Herbland A, Cantini O, Reynier P, Valat P, Jougon J, Arimone Y, et al. The bilateral superficial cervical plexus block with 0.75% ropivacaine administered before or after surgery does not prevent postoperative pain after total thyroidectomy. Reg Anesth Pain Med. 2006;31:34–9. https://doi.org/10.1016/j.rapm.2005.10.008.
Wang Y, Shen J, Xie R, Tan D, Jin X, Shen L, et al. Evaluation of a precision approach to intraoperative ropivacaine nerve block to improve postoperative analgesia in 120 patients undergoing thyroid surgery. Med Sci Monit. 2022;28:e935563. https://doi.org/10.12659/MSM.935563.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Rev Esp Cardiol (Engl Ed). 2021;74:790–9. https://doi.org/10.1016/j.rec.2021.07.010.
Ahiskalioglu A, Yayik AM, Oral Ahiskalioglu E, Dostbil A, Doymus O, Karadeniz E, et al. Ultrasound-guided bilateral superficial cervical block and preemptive single-dose oral tizanidine for post-thyroidectomy pain: a randomized-controlled double-blind study. J Anesth. 2018;32:219–26. https://doi.org/10.1007/s00540-018-2468-x.
Andrieu G, Amrouni H, Robin E, Carnaille B, Wattier JM, Pattou F, et al. Analgesic efficacy of bilateral superficial cervical plexus block administered before thyroid surgery under general anaesthesia. Br J Anaesth. 2007;99:561–6. https://doi.org/10.1093/bja/aem230.
Cai HD, Lin CZ, Yu CX, Lin XZ. Bilateral superficial cervical plexus block reduces postoperative nausea and vomiting and early postoperative pain after thyroidectomy. J Int Med Res. 2012;40:1390–8. https://doi.org/10.1177/147323001204000417.
Hisham N, Ashraf M, Mohamed R, Adil K, Saif A. The Influence of Bilateral Superficial Cervical Plexuses Block (BSCBs) as pre-emptive analgesia on patient satisfaction after thyroid surgery. Alexandria J Anaesthesia Intensive Care. 2005;8(4):11–7.
Kesisoglou I, Papavramidis TS, Michalopoulos N, Ioannidis K, Trikoupi A, Sapalidis K, et al. Superficial selective cervical plexus block following total thyroidectomy: a randomized trial. Head Neck. 2010;32:984–8. https://doi.org/10.1002/hed.21286.
Shih ML, Duh QY, Hsieh CB, Liu YC, Lu CH, Wong CS, et al. Bilateral superficial cervical plexus block combined with general anesthesia administered in thyroid operations. World J Surg. 2010;34:2338–43. https://doi.org/10.1007/s00268-010-0698-7.
Dieudonne N, Gomola A, Bonnichon P, Ozier YM. Prevention of postoperative pain after thyroid surgery: a double-blind randomized study of bilateral superficial cervical plexus blocks. Anesth Analg. 2001;92:1538–42. https://doi.org/10.1097/00000539-200106000-00038.
Steffen T, Warschkow R, Brandle M, Tarantino I, Clerici T. Randomized controlled trial of bilateral superficial cervical plexus block versus placebo in thyroid surgery. Br J Surg. 2010;97:1000–6. https://doi.org/10.1002/bjs.7077.
Karthikeyan VS, Sistla SC, Badhe AS, Mahalakshmy T, Rajkumar N, Ali SM, et al. Randomized controlled trial on the efficacy of bilateral superficial cervical plexus block in thyroidectomy. Pain Pract. 2013;13:539–46. https://doi.org/10.1111/papr.12022.
Gurkan Y, Tas Z, Toker K, Solak M. Ultrasound guided bilateral cervical plexus block reduces postoperative opioid consumption following thyroid surgery. J Clin Monit Comput. 2015;29:579–84. https://doi.org/10.1007/s10877-014-9635-x.
Suh YJ, Kim YS, In JH, Joo JD, Jeon YS, Kim HK. Comparison of analgesic efficacy between bilateral superficial and combined (superficial and deep) cervical plexus block administered before thyroid surgery. Eur J Anaesthesiol. 2009;26:1043–7. https://doi.org/10.1097/EJA.0b013e32832d6913.
Yao Y, Lin C, He Q, Gao H, Jin L, Zheng X. Ultrasound-guided bilateral superficial cervical plexus blocks enhance the quality of recovery in patients undergoing thyroid cancer surgery: a randomized controlled trial. J Clin Anesth. 2020;61:109651. https://doi.org/10.1016/j.jclinane.2019.109651.
Aweke Z, Sahile WA, Abiy S, Ayalew N, Kassa AA. Effectiveness of bilateral superficial cervical plexus block as part of postoperative analgesia for patients undergoing thyroidectomy in Empress Zewditu Memorial Hospital, Addis Ababa. Ethiopia Anesthesiol Res Pract. 2018;2018:6107674. https://doi.org/10.1155/2018/6107674.
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. https://doi.org/10.1136/bmj.d5928.
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. https://doi.org/10.1016/0197-2456(95)00134-4.
McGrath S, Zhao X, Steele R, Thombs BD, Benedetti A, Collaboration DESD. Estimating the sample mean and standard deviation from commonly reported quantiles in meta-analysis. Stat Methods Med Res. 2020;29:2520–37. https://doi.org/10.1177/0962280219889080.
Furlan AD, Pennick V, Bombardier C, van Tulder M, Editorial Board CBRG. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine (Phila Pa 1976). 2009;34:1929–41. https://doi.org/10.1097/BRS.0b013e3181b1c99f.
Spanknebel K, Chabot JA, DiGiorgi M, Cheung K, Lee S, Allendorf J, et al. Thyroidectomy using local anesthesia: a report of 1,025 cases over 16 years. J Am Coll Surg. 2005;201:375–85. https://doi.org/10.1016/j.jamcollsurg.2005.04.034.
Snyder SK, Roberson CR, Cummings CC, Rajab MH. Local anesthesia with monitored anesthesia care vs general anesthesia in thyroidectomy: a randomized study. Arch Surg. 2006;141:167–73. https://doi.org/10.1001/archsurg.141.2.167.
Warschkow R, Tarantino I, Jensen K, Beutner U, Clerici T, Schmied BM, et al. Bilateral superficial cervical plexus block in combination with general anesthesia has a low efficacy in thyroid surgery: a meta-analysis of randomized controlled trials. Thyroid. 2012;22:44–52. https://doi.org/10.1089/thy.2011.0260.
Mayhew D, Sahgal N, Khirwadkar R, Hunter JM, Banerjee A. Analgesic efficacy of bilateral superficial cervical plexus block for thyroid surgery: meta-analysis and systematic review. Br J Anaesth. 2018;120:241–51. https://doi.org/10.1016/j.bja.2017.11.083.
Acknowledgements
Not applicable.
Funding
This study was supported by National key research and development program (No. 2018YFC2001805).
Author information
Authors and Affiliations
Contributions
Y.C. and H.S. designed the clinical study; Y.C., L.N., H.L., Q.L. and Y.Z conducted initial searches, reviewed trials, and included trials into analysis; Y.C. analyzed the data and drew graphs and tables; Y.C. drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
In this systematic review, meta-analyses were performed in strict accordance with the criteria stated in PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analysis, PRISMA). The protocols retrieved for this study were registered on the PROSPERO platform (registration number CRD42022309503).
Consent for publication
The work described has not been published before.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplemental Table 1.
Search Protocol.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cai, Y., Nong, L., Li, H. et al. Effect of bilateral superficial cervical plexus block on postoperative pain, nausea, and vomiting in thyroid surgery: a systematic review and meta-analysis. APS 1, 13 (2023). https://doi.org/10.1007/s44254-023-00012-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44254-023-00012-8