Abstract
Alveolar de recruitment is a common problem during general anesthesia and operations. Pediatric cardiac surgery with cardiopulmonary Bypass is associated with interruption of ventilation and might enhance loss of Ventilation compared to other surgical procedures. Electrical impedance tomography (EIT) allows for monitoring of ventilation distribution and can be helpful in detecting pulmonary de recruitment. This case series demonstrates for the first time that EIT is feasible during open heart surgery and in patients with open chest on the ICU using adapted belts in pediatric patients. It might be helpful to monitor changes in tidal volume distribution, to detect loss of Ventilation during surgery and to guide recruitment maneuvers. Study registration: NCT06270485, clincialtrials.gov, 02/02/2024.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ventilation strategies in children and adults changed significantly over the past decades [1]. However, in children with congenital heart disease (CHD) there is still a lot of uncertainty regarding cardiopulmonary-interactions and how to manage mechanical ventilation to avoid hemodynamic impairment. Many physicians are concerned to use higher levels of positive-end-expiratory-pressure (PEEP) and tend to use higher driving-pressures instead which is supported by some older studies published during the 1990’s proposing the use of very low or no PEEP [2].
On the other hand several trials confirmed that ventilation mismatch and atelectasis contributes to higher pulmonary-vascular-resistance (PVR), reduced oxygenation and prolonged invasive mechanical ventilation and that driving-pressure might be much more relevant for hemodynamic effects than is PEEP [3, 4]. Electrical impedance tomography (EIT) is a relatively new monitoring tool using changes in electrical impedance of the lungs, detected by special sensor belts placed around the chest, to visualize and quantify regional distribution of ventilation. This technique aims to detect regional and global ventilation changes breath by breath and to evaluate the efficacy of therapeutic interventions. A significant clinical impact of EIT has already been shown in studies on a general pediatric population which reported alveolar de recruitment even during induction of anesthesia and short surgical procedures [5]. Up until now, there have been no reports of the use of EIT in pediatric cardiac surgery. Given the fact that a monitoring belt around a part of the chest is required for EIT measurements, it was unclear if EIT is feasible during pediatric cardiac surgery. With the device of Timpel Medical® we were able to adapt the belts in a way that makes it possible to use it in patients with open chest. The pediatric and adult Timpel-belts do consist of two parts (left and right) making it possible to adjust the size of the gap around the sternum by using a belt that is intended for smaller patients. Most devices leave an electrode-gap over the sternum and make it possible to adjust this gap in a small range of some centimeters. In our two patients we used neonatal belts that were intended for the use in smaller children making it possible to create a larger gap for sternotomy and surgery without losing any electrode signals. The neonatal Timpel-belts do consist of one instead of two parts compared to the pediatric and adult belts. To create the gap that is necessary it is possible to cut these neonatal belts in two parts at the indication line that is otherwise placed in the middle of the sternum. Both parts of this so cut belt are placed from the spine to the mamillae, one on the right and one on the left side. It is important to keep the offset of electrodes when fixing both belts on the spine (Figures in supplemental material). With this approach it is possible to monitor patients down to 3 kg during heart surgery with a gap of approximately 10–15 cm. To prevent signal loss of electrodes during surgery we fixed the belts with transparent dressings.
Here we report on 3 successful EIT measurements in 2 children with CHD. We performed 2 observational measurements during surgery without influencing any decision of the anesthesiologist or surgeon. In the second patient we monitored a second measurement on the CICU to guide an interventional and standardized recruitment maneuver that was performed due to significant atelectasis after surgery. To our knowledge this is the first report on using EIT during pediatric open-heart-surgery and in patients with open-chest on cardiac intensive care unit (CICU).
Case series
All EIT measurements were done with the Timpel Enlight 2100→ device (Timpel Medical®; 7955 Silverton Ave., Ste. 1216, San Diego, Ca. 92,126, USA).
Case 1
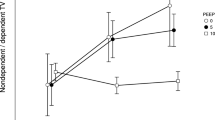
2-year-old female patient with a body weight of 11,3 kg (former preterm with 27 weeks of gestational age) who received surgical closure of an atrial septal defect via partial sternotomy. The patient was monitored with EIT (N5 belt cut in two parts) throughout the whole procedure, starting at Ventilation (Perseus, Draeger®, Germany) in a pressure-controlled mode with a PEEP of 6cmH2O showing normal lung compliance around 1 ml/cmH2O/kg. When going on Cardiopulmonary Bypass (CPB) ventilation was stopped (no driving-pressure) but a PEEP of 10cmH2O was maintained. Ventilation was re-started with a PEEP of 6cmH2O and driving-pressures between 8 and 17 cmH2O. Tidal-volume decreased from 8,7 ml/kg (compliance 1,1 ml/cmH2O/kg) prior CPB to 5,3 ml/kg (compliance 0,64 ml/cmH2O/kg) after CPB compared prior CPB (Fig. 1). EIT showed a significant decrease in end-expiratory-lung-volume (EELZ = FRC) compared to baseline indicating alveolar de recruitment (Fig. 2). Because increasing the peak-inspiratory-pressures did not improve volumes, a manual recruitment maneuver using hand-bagging for several breaths was performed. Additionally higher driving-pressures were applied for some minutes (up to 17cmH2O). The patient was uneventfully extubated in the operating-room at the end of the procedure and transferred to CICU on nasal cannula oxygen.
With the EIT device it is possible to generate ventilation change images. It is necessary to set marks at different time-points that should be compared. The reference mark (left image) reflects the impedance at the beginning of the operation. The cursor mark (image in the middle) was set after CPB was stopped. The ventilation change image on the right side reflects the change in ventilation between those two time points calculated by the device based on changes in impedance. The numbers and values on the right were generated with the device-specific proximal flow-sensor and show the measured values to the same time points outlined before. Re-start of mechanical ventilation after weaning from CPB shows loss of ventilation in impedance and reduced tidal-volumes and compliance measured by the flow sensor. Red-zones reflect loss of ventilation. Tidal-volumes decreased to 61% from baseline with same driving-pressures. Ventilation distribution is indicated by the percentage of ventilation in the region of interest. A/P = anterior/posterior, R/L = right/left, TVz = tidal volume, Pdriving = driving-pressure; Crs = Compliance Respiratory System; TVz = Tidal Volume, VT = Tidal Volume in ml
Loss of end-expiratory-lung-volume (EELZ = FRC) after weaning from CPB and going back on mechanical ventilation (Cur set after CPB compared with Ref before CPB). The reference mark in this case was set just before going on CPB and the cursor mark is set at the same time point than in Fig. 1 when weaning from CPB. There is no tidal-volume (TVz) generated during CPB as only static PEEP of 10cmH2O was applied. Big swings after returning on ventilation (10:45) indicate hand-bagging with high pressures and volumes. After weaning from CPB EELZ (= FRC) decreases subsequently. EELZ = end-expiratory-lung-volume, TVz = Tidal-Volume
Case 2
Male infant 4months of age, 4,5 kg (born preterm at 34 weeks gestational age with 1100 g) for surgical correction of Tetralogy of Fallot. X-ray prior surgery was normal, the patient did not need any breathing-support or supplemental oxygen before admission to hospital. We monitored the patient with EIT throughout the whole operation starting with intubation. We used a Timpel® neonatal N0 belt cut in two parts, leaving a gap around the sternum of approximately 10–15 cm for the operation field during open-heart-surgery. EIT was feasible with good image quality (belts captured the dorsal parts of the lungs to the anterior axillary-line on both sides). The patient was first ventilated using a volume-controlled mode with a volume-target of 10 ml/kg and a PEEP of 3cmH2O (Perseus, Draeger®, Germany) before starting CPB. EIT showed signals of alveolar overdistension in dynamic images at this time (Video 1, suppl.) Due to surgical difficulties and difficulties with weaning from CPB three CPB runs were necessary. During each CPB run ventilation was stopped and no PEEP was applied. When re-starting mechanical ventilation a pressure controlled mode (SIMV) was used with a PEEP of 5 cm H2O, driving-pressures > 15 cm H2O and inhaled-nitric-oxide was given with 40ppm. Tidal-volume decreased from 10 ml/kg in VCV with a driving-pressure of 12cmH2O prior operation (corresponding compliance of 1 ml/cmH2O/kg) to 5 ml/kg in PCV with a driving pressure of 19cmH2O (corresponding compliance < 0,5 ml/cmH2O/kg). EIT showed a decrease in end-expiratory-lung-volumes of about 100–120% in all regions of interest (anterior/posterior, right/left) indicating alveolar de-recruitment (Fig. 3, suppl.) and so called Pendelluft (movement of gas between two regions of the lung with different compliance) in dynamic images (Video 2, suppl.). No standardized recruitment maneuver was performed during surgery. Weaning from CPB was impossible. The patient went on central Veno-Arterial-ECMO. Within few hours the patient developed atelectasis of the right upper lobe and the next day also of the left lung generating tidal volumes around 1,5 ml/kg on a PEEP of 8 cm H2O and a driving-pressure of 15cmH2O in pressure-controlled ventilation. After performing an EIT-guided recruitment maneuver with incremental/decremental PEEP-titration up to 24cmH2O and constant driving pressure of 12 cm H2O (Servo-U, Getinge ®) the atelectatic lung regions could be re-opened and PEEP was maintained at 10 cm H2O with improvement in tidal-volumes. The chest X-ray images at the beginning of recruitment and afterwards are shown in Fig. 4. EIT monitoring was possible with good image quality throughout the whole procedure. When performing the recruitment maneuver EIT showed a redistribution of tidal volumes from the non-dependent anterior/ventral lung to the dependent posterior/dorsal lung resulting in a homogenization of tidal volume distribution especially during decremental PEEP titration. Sweep-gas-flow and FiO2 could be reduced on ECMO after recruitment. On day 7 the patient was successfully weaned from ECMO support.
Changes in EIT-Plethysmogram when re-starting ventilation after CPB. The changes of impedance signals before CPB and after 3 runs of CPB are shown here. There are 4 regions of interest (anterior, posterior, right and left) showing a decrease of End-Expiratory-Lung-Volume (= EELZ) by about 120% in all regions of interest. The posterior region of interest reflecting ventilation of the dorsal lung is substantially decreased compared the anterior region of interest reflecting ventral ventilation
Recruitment maneuver Case 2: picture on top: Substantial improvement of regional ventilation after recruitment maneuver with green areas reflecting gain of ventilation and red zones showing loss of ventilation indicating re-distribution of tidal-volume in this case due to homogenization of anterior and posterior ventilation. Picture in the middle: The gain in Amplitude in the global Plethysmogram reflects gain in tidal volume that occurs typically while decremental PEEP-titration after initial recruitment. X-Ray images before (left) and after recruitment (right). A/P = anterior/posterior, R/L = right/left, TVz = tidal volume, Pdriving = driving-pressure; Crs = Compliance Respiratory System; TVz = Tidal Volume, VT = Tidal Volume in ml
Discussion
There is evidence that alveolar de recruitment and formation of atelectasis is a common problem in mechanically ventilated children especially in the operating room [5, 6]. Surgical correction of patients with CHD is often associated with very long surgery times and changes in respiratory mechanics due to sternotomy and the use of CPB. There is only very little data on how to ventilate patients under these special conditions to prevent ventilation and perfusion mismatches. This is the first report on using EIT during pediatric cardiac surgery with CPB. Today EIT is getting more readily available as there are more devices on the market than few years ago. Many of them offer age-specific-belts making it possible to use them in children and infants. We were able to show that EIT is feasible during these operations with good image quality. As atelectasis formation occurs predominantly in the dorsal parts of the lung these areas are detected by EIT even during sternotomy by using belts that are intended for smaller children creating a larger ventral gap. Our data show that current ventilation strategies during pediatric cardiac surgery are potentially associated with clinically relevant alveolar de recruitment. Stopping ventilation during CPB is associated with substantial loss in end-expiratory-lung-volumes indicating alveolar de recruitment. The application of a static PEEP of 10cmH2O in Case 1 showed less de recruitment than applying no PEEP at all as in Case 2. But de recruitment in Case 1 also occurred when reducing PEEP from 10 to 6 cmH2O directly after CPB. A short recruitment maneuver after re starting ventilation aiming for a PEEP of 12-15cmH2O for few breaths with driving-pressures between 12 and 15 cm H2O for lung protection might be an approach to restore functional residual capacity (FRC) after weaning from CPB. We hypothesize that standardized recruitment maneuvers would be beneficial to restore FRC and to avoid ventilator-induced-lung-injury caused by high driving-pressures which are often applied when compliance is decreased and tidal volumes are low. The same signals of substantial decrease in FRC were seen in case 2. In this patient mechanical ventilation had been stopped three times without applying any kind of distending pressures to the lung, what might have aggravated alveolar de recruitment in this case. In both patients no standardized recruitment maneuvers had been applied during or after surgery. Case 2 developed significant atelectasis after surgery. We performed a standardized recruitment maneuver in this patient with open chest on VA-ECMO on pCICU. We were able to show that EIT could also be helpful to guide recruitment maneuvers with incremental/decremental PEEP-titration to avoid lung stress and strain especially in patients with significantly reduced lung compliance. Several recent studies in adults support this approach of which only few used EIT [7]. Performing those recruitment maneuvers in patients with very sick lungs takes time (up to several hours) and usually much higher PEEP level. In CHD-patients with normal lung compliance prior operation these maneuvers can be done within few minutes and with lower PEEP (up to 15 cm H2O) so that FRC is restored when going off CPB. Further trials are needed to determine which ventilation strategies are beneficial in preventing alveolar de recruitment and to avoid lung injury in this cohort of patients. EIT is a non-invasive and reproducible technique. The presented data demonstrate that EIT can be an additional valuable tool to assess ventilation strategies and that it is feasible even during pediatric cardiac surgery with sternotomy and in patients with open chest. Although the technique is not available in every institution and it takes some time to prepare the belts and device. Our results are limited by the fact that the use of the belts and device were off-label. The belts that were used in our two patients were intended to be used in smaller patients with a smaller circumference of the thorax. By using the described setting we were able to create a larger gap around the sternum that is necessary in case of sternotomy and in patients with open chest without having loss of electrode signals. The EIT pictures that were generated with this application are based on belts for smaller patients so that we cannot guarantee the same quality of EIT measurements compared to the use of belts that cover the whole circumference and are therefore larger. However, even if we created an “artificial baby-lung” by using smaller belts than intended we do believe that EIT signals can be helpful to monitor ventilation changes in those regions of the lung that are captured by the belts we used. This conclusion is supported by the observed changes measured with the device specific proximal flow sensor that showed the same signals regardless the fact that we used adapted belts.
Data availability
All data of the underlying case series can be provided to the editors if necessary.
Code availability
Not applicable.
Abbreviations
- CPB:
-
Cardio Pulmonary Bypass
- CHD:
-
Congenital Heart Disease
- CICU:
-
Cardiac Intensive Care Unit
- ECMO:
-
Extracorporeal Membrane Oxygenation
- EELZ:
-
End-Expiratory-Lung-Volume
- EIT:
-
Electrical Impedance Tomography
- FRC:
-
Functional Residual Capacity
- ICU:
-
Intensive Care Unit
- PCV:
-
Pressure Controlled Ventilation
- PEEP:
-
Positive End Expiratory Pressure
- PVR:
-
Pulmonary Vascular Resistance
- SIMV:
-
Synchronized Intermittend Mandatory Ventilation
- VCV:
-
Volume Controlled Ventilation
References
Amato MB, Meade MO, Slutsky AS et al (2015) Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med Feb 19(8):747–755. https://doi.org/10.1056/NEJMsa1410639
Shekerdemian LS, Bush A, Lincoln C, Shore DF, Petros AJ, Redington AN (1997) Cardiopulmonary interactions in healthy children and children after simple cardiac surgery: the effects of positive and negative pressure ventilation. Heart Dec 78(6):587–593. https://doi.org/10.1136/hrt.78.6.587
Khemani RG, Parvathaneni K, Yehya N, Bhalla AK, Thomas NJ, Newth CJL (2018) Positive End-Expiratory Pressure Lower Than the ARDS Network Protocol Is Associated with Higher Pediatric Acute Respiratory Distress Syndrome Mortality. Am J Respir Crit Care Med. Jul 1. ;198(1):77–89. https://doi.org/10.1164/rccm.201707-1404OC
Boesing C, Schaefer L, Schoettler JJ et al (2023) Effects of individualised positive end-expiratory pressure titration on respiratory and haemodynamic parameters during the Trendelenburg position with pneumoperitoneum: a randomised crossover physiologic trial. Eur J Anaesthesiol Nov 1(11):817–825. https://doi.org/10.1097/EJA.0000000000001894
Nascimento MS, Rebello CM, Costa ELV et al (2023) Effect of general anesthesia and controlled mechanical ventilation on pulmonary ventilation distribution assessed by electrical impedance tomography in healthy children. PLoS ONE 18(3):e0283039. https://doi.org/10.1371/journal.pone.0283039
Clasen D, Winter I, Rietzler S, Wolf GK (2023) Changes in ventilation distribution during general anesthesia measured with EIT in mechanically ventilated small children. BMC Anesthesiol Apr 12(1):118. https://doi.org/10.1186/s12871-023-02079-z
Songsangvorn N, Xu Y, Lu C et al (2024) Electrical impedance tomography-guided positive end-expiratory pressure titration in ARDS: a systematic review and meta-analysis. Intensive Care Med Mar 21. https://doi.org/10.1007/s00134-024-07362-2
Funding
Open Access funding enabled and organized by Projekt DEAL. The work was supported by a funding of Deutsche Herzstiftung e.V. to author JCC. There was no involvement in the clinical work or the interpretation of data by the funding party.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
JCC was responsible for conception, acquisition, analysis and interpretation of data, drafting and reviewing of the manuscript, ME was involved in conception and acquisition of data, review, MKB and MYC were involved in acquisition of data and review, MK was involved in interpretation of data and reviewing the work, OM was involved in conception, interpretation and review. All authors reviewed the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the Charité on November 24th 2023, EA2/224/23. Written informed consent of parents was obtained prior to examination including consent to publication of data.
Competing interests
The authors have no relevant financial or non-financial interests to disclose. The authors have no competing interests to declare that are relevant to the content of this article. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript. The authors have no financial or proprietary interests in any material discussed in this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Clausen, JC., Emeis, M., Kleine-Brueggeney, M. et al. “Electrical impedance tomography during open heart surgery and on the cardiac icu is feasible to monitor ventilation in children with congenital heart disease”. Intensive Care Med. Paediatr. Neonatal 2, 19 (2024). https://doi.org/10.1007/s44253-024-00043-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44253-024-00043-4