Abstract
Purpose
To determine whether late admission to pediatric intensive care (ICU) from hospital wards is associated with patient outcomes.
Methods
Secondary analysis of prospectively collected data from an international multicenter cluster-randomized trial. Clinical deterioration events with urgent ICU admission were defined as late if the Children’s Resuscitation Intensity Scale was > 2 (indicating critical care interventions started from 12 h pre- to 1 h post-urgent ICU admission). The association of late admission with primary outcomes (ICU and hospital mortality) was estimated using logistically generalized estimating equation models adjusted for PIM2 probability of death.
Results
There were 2979 clinical deterioration events in 2502 patients, including 620 (20.8%) late ICU admissions. ICU mortality of the last urgent ICU admission was 15.4% for late compared to 4.5% for non-late ICU admission (PIM-adjusted OR (95%CI) 1.63 (1.14, 2.33), p < 0.01). Hospital mortality was 19.7% in late compared to 6.0% for non-late urgent ICU admission (PIM-adjusted OR 1.56 (1.12, 2.16), p < 0.01). Late ICU admissions accounted for 20.9% of clinical deterioration events, and 90/179 (50.2.0%) of ICU and 103/222 (46.4%) of hospital deaths after clinical deterioration events. Secondary outcomes associated with late ICU admission included longer ICU stay (2.3 days, p = 0.02), more ventilation days (407/1000 ICU days, p < 0.0001), and more frequent treatment with dialysis, inhaled nitric oxide, and extracorporeal membrane oxygenation (p < 0.01).
Conclusion
Late ICU admission from hospital wards was associated with higher ICU and hospital mortality, greater use of ICU technologies, and longer ICU stays. How to prevent late ICU admission and its consequences requires further study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Take-home message
In a secondary analysis of prospectively collected data from a large international multicenter cluster-randomized trial, late urgent admission to pediatric intensive care was associated with intensive care mortality, aOR (95%CI) 1.63 (1.14, 2.33) and OR (95%CI)1.65 (95% CI 1.16, 2.36), and hospital mortality, aOR 1.56 (1.12, 2.16) and OR (95%CI)1.58 (95% CI 1.14, 2.19), compared to non-late urgent intensive care admissions. Understanding the mechanisms, plus preventing and mitigating the consequences of late intensive care admissions should be a priority for future research.
Introduction
Management in critical illness is frequently time-sensitive. Treatment delays in sepsis, after stroke, myocardial infarction, and critical illness in adults are each associated with worse outcomes [1]. In adult critically ill patients, timely admission to the intensive care unit (ICU) has been associated with improved outcomes [2, 3] and forms the basis of the “right care right now” imperative advocated by the Society of Critical Care Medicine, underpins the concept of “failure to rescue” in the rapid response literature [4, 5], and grounds the rationale for timely initiation of mechanical circulatory support for patients in ICU [6]. Single-center studies suggest that children urgently admitted to ICU from hospital wards have increased risk-adjusted mortality compared with children admitted electively or from other ICUs [7], and ICU mortality is higher and survivorship outcomes worse in patients who experience pre-ICU arrest, or those receiving some versus no ICU therapies in the first 12 h after ICU admission [8, 9].
Our cluster randomized trial Evaluating Processes of care and Outcomes in Children’s Hospitals (EPOCH) of the Bedside Pediatric Early Warning System (BedsidePEWS) compared with usual care found no significant difference in the primary outcome—hospital mortality and that the secondary outcome—a composite measure that we called the “significant clinical deterioration event” was significantly reduced in intervention hospitals [10]. This measure of late ICU admission involved the provision of significant respiratory and/or circulatory support before and/or immediately after ICU admission (Table 1). Reducing this late ICU admission is consistent with the notion of early warning approaches to permit timely ICU admission. The rationale for the use of this late ICU admission measure was based on its face validity, informal endorsement by members of two clinical trial organizations, association with ICU mortality in preliminary evaluation [11, 12], and the anticipated consequences for individual patients as a means to reduce mortality [10]. We sought to evaluate these assumptions and quantify the system-level effects of late ICU admission.
Methods
We performed a secondary analysis of the EPOCH dataset (NCT01260831). The specific objectives were to describe and compare mortality and ICU resource utilization in patients with late versus other (non-late) urgent admission to ICU from an inpatient ward and to describe the proportions of ICU days represented by late versus other urgent ICU admission. Eligible events were clinical deterioration events occurring in eligible patients enrolled from 28 February 2011 to 21 June 2015 in inpatient wards in the 22 hospitals collecting data as part of the EPOCH trial. The participating hospitals were from New Zealand, England, Ireland, Italy, The Netherlands, and Canada, and had a median (IQR) of 82 (60–127) pediatric inpatient ward beds. All had a paediatric intensive care unit [10]. Eligible patients had no treatment limitations, were receiving care in an inpatient ward, and were not undergoing an anesthetist-supervised procedure at the time of the event.
Clinical deterioration events were defined as those that resulted in either death before urgent ICU admission or urgent ICU admission [defined as < 6 h from initiation to departure toward the ICU from the event location]. Late ICU admission was defined as the subset of clinical deterioration events with one or more of the following: death before ICU; provision of cardiopulmonary resuscitation, tracheal intubation, administration of vasoactive medication, or provision of fluid boluses of 60 ml/kg or more in the 12 h before ICU admission; or in the first hour of ICU admission having tracheal intubation, cardiopulmonary resuscitation, initiation of extracorporeal membrane oxygenator therapy, or death [10]. Late ICU admission included mortality in patients without Do Not Attempt Resuscitation orders who died before transfer to ICU. This definition of late ICU admission was operationalized using the Children’s Resuscitation Intensity Scale, with a scale of > 2 pre-defined to indicate late ICU admission (Table 1). We excluded patients who remained in the wards after one or more ICU consultations, resuscitation team calls, or immediate calls for physician attendance, as data was only available for those urgently admitted to ICU. For patients that had multiple clinical deterioration events, the last event and corresponding ICU admission were used for analysis.
The primary outcome was ICU mortality. Secondary outcomes were hospital mortality and the use of ICU therapies—non-invasive mechanical ventilation, invasive mechanical ventilation, inotrope-vasopressors, inhaled nitric oxide, dialysis (of any type), mechanical circulatory or respiratory support with ECMO, and the duration of ICU stay. These were expressed as the number and proportion of individuals experiencing each outcome, as the number of days individuals received each therapy or remained in the ICU, and as a portion of ICU resource utilization for the entire cohort.
Research involving human participants
This EPOCH sub-study was approved by the Human Research Ethics Board at the Hospital for Sick Children, Toronto, Canada; Approval REB # 1000062622. The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Consent to participate
The EPOCH trial had research ethics board approval obtained at each participating hospital. The need for written informed consent for patient or clinician participation was waived in all jurisdictions.
Analyses
Patient characteristics are summarized by counts and percentages and compared between those with late and other (non-late) urgent ICU admissions using chi-squared tests. The effect of late admission on ICU mortality and hospital mortality was estimated separately using logistically generalized estimating equation (GEE) models adjusted for PIM probability of death (using a 3-degree-of-freedom natural spline) and using an exchangeable correlation matrix to account for clustering within the hospital. The effect of late admission on secondary outcomes was estimated using univariable logistic (for binary variables) and linear (for other variables) GEE models with exchangeable correlation matrices to account for clustering within the hospital. Cumulative incidence functions were estimated for the two competing events that end the ICU stay, that is, in-ICU mortality and ICU discharge. The sub-distribution hazard ratio for the effect of ICU on the incidence of these events was estimated from the Fine and Gray model.
Results
The 220,363 patients enrolled in the 22 hospitals of the EPOCH trial were observed for 909,642 patient days during the baseline and post-randomization phases of the trial. Overall, there were 2979 clinical deterioration events with an associated urgent ICU admission or death prior to ICU admission (3.27/1000 patient days) in 2502 patients (2160 patients had one eligible event, 253 had two, and 89 had 3 to 8 eligible events). The 620 (20.8%) late ICU admissions were associated with 6219 (25.5%) days of ICU care and included a mean (SD) of 6.7 (12.0) days of mechanical ventilation per admission. The 2359 (79.2%) urgent ICU admissions that were not classified as late were in ICU for a total of 18,125 (74.5%) days and received a mean (SD) of 2.7 (8.9) days of mechanical ventilation.
Analysis of the last clinical deterioration event included 2502 patients, with 524 (20.9%) late and 1978 (79.1%) other urgent ICU admissions. There were 11 patients who died before ICU admission and 2 who died in the first hour of urgent ICU admission (Table 2). Patients who had late ICU admission were more likely to have had an associated resuscitation team call and a cardiovascular diagnosis and less likely to have a respiratory diagnosis compared to patients with other urgent ICU admissions. Clinical characteristics of the last eligible event were otherwise similar in patients with late versus other urgent ICU admissions (Table 2). PELOD scores on the first day of admission were significantly higher in patients with late ICU admission and were higher for the whole ICU stay (Table 3).
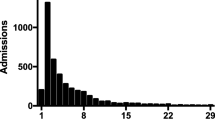
Mortality before urgent ICU admission occurred in 11 (0.5%) patients. Patients with late ICU admission had higher PIM-calculated probability of death with a mean difference of 9.6% (95% CI 8.0–11.2%). The primary outcome, mortality before ICU discharge, was 15.4% for patients with a late admission compared to 4.5% for those without late admission (Fig. 1), with adjusted (for PIM predicted mortality) OR of 1.65 (95% CI 1.16–2.36, p < 0.01). Figure 2 shows the cumulative incidence of mortality over the length of the ICU stay. For both late and non-late urgent ICU admissions, most deaths occurred in the first 2 weeks of ICU stay, with a much steeper increase in the late admission group. The sub-distribution hazard ratio (SDHR) for mortality comparing the late and non-late groups was 3.7 (95% CI 2.7, 4.9). Cumulative incidence of discharge alive from the ICU was decreased in the late group compared to the non-late group, with an SDHR of 0.63 (95% CI 0.57, 0.69), a result that aligns with the longer mean ICU length of stay in the late group (an analysis that does not differentiate on the final ICU disposition). In total, 92 of the 181 patients (50.8%) who died before or during an ICU admission did so in association with a late ICU admission event.
ICU Mortality according to the Children’s Resuscitation Intensity Scale. Point estimates with a 95% confidence interval for ICU mortality after clinical deterioration in patients without care restrictions. Patients were classified by the Children’s Resuscitation Intensity Scale. Late ICU admission was defined as scores of 3–7 and included patients who in 12 h before urgent ICU admission had received one or more of invasive positive pressure ventilation (endotracheal tube or tracheostomy) or significant circulatory support (inotropes, other vasoactive medications, mechanical support), had a cardiac arrest, were intubated, had a cardiac arrest, or were placed on extra-corporeal membrane oxygenator therapy within an hour of ICU admission. Other patients not receiving significant circulatory or invasive respiratory support in 12 h before or the first hour after urgent ICU admission are rated as one or two (non-invasive positive pressure ventilation) on this 7-point scale and are not classified as having late ICU admission. We did not present the data from patients who died during the event (score of 7) given the 100% mortality
Cumulative incidence of in-ICU death according to early or late urgent ICU admission. Cumulative incidence of ICU mortality and discharge in 2489 patients in the EPOCH trial with clinical deterioration events who survived more than 1 h after urgent ICU admission. We excluded the 11 patients who died before ICU admission and the 2 patients who died within an hour after admission. This Kaplan–Meier graph shows that those with a late ICU admission have a higher incidence of mortality and lower incidence of discharge at any time after ICU admission
Hospital mortality was 19.7% in patients with late ICU admission and 6.0% in other patients with urgent ICU admission, with an adjusted (for PIM predicted mortality) OR (95% CI) of 1.56 (1.12, 2.16), p < 0.01). Therefore, late ICU admissions accounted for 90/179 (50.3%) of ICU deaths and 103/222 (46.4%) of hospital deaths after clinical deterioration events.
Secondary outcomes in patients with late ICU admission included an ICU stay 2.3 days longer (p = 0.02), an additional 407 ventilation days per thousand ICU days (p < 0.0001), and more frequent treatment with dialysis, inhaled nitric oxide, and extracorporeal membrane oxygenation (all p < 0.01) (Table 2).
Discussion
In this secondary evaluation of the dataset of a large cluster RCT, we evaluated 2979 index clinical deterioration events in 2502 patients. A comparison of 524 patients with late ICU admission events, with 1978 patients with more timely urgent ICU admission showed patients with late ICU admission had higher severity of illness at ICU admission, greater use of ICU technologies, spent longer in ICU, and had increased ICU and hospital mortality.
These findings are concordant with other studies suggesting that the consequences of late ICU admission are significant [13,14,15,16,17]. Their implications relate to individual patients and to the health system. First, for individual patients, late ICU admission can be a sentinel event. We found late ICU admission was associated with significantly increased mortality, 2.3 days longer ICU length of stay, and increased organ dysfunction. This provides a rationale to target more timely ICU admission in critically ill children—or more specifically—the prevention of late ICU admission in patients with treatable conditions. We found an increased risk of mortality associated with late ICU admission events: the 21% of patients who had late ICU admission events comprised 50% (n = 90) of deaths occurring in or before ICU and 46% (n = 103) of the 222 deaths that occurred in the hospital. These data from 22 pediatric centers align with adult data underpinning the Society of Critical Care Medicine (SCCM) guidelines for adult ICU admission [18] and the notion of “right care right now” espoused by the SCCM and implicit in rapid response team, acute cardiovascular, and neurologic care [5, 19].
Second, and in contrast to the apparently disproportionate use of resources by individual patients, at a system level, the total resources consumed by patients with late ICU admission were diluted by the larger number of patients with less immediately severe illness. The 524 (21%) patients with late ICU admission events occupied 26% of the ICU days occupied by the 2502 patients with urgent ICU admission, 12% of all ICU days occupied by patients in the studied ICUs, and comprised 4.1% of all ICU patient admissions during the EPOCH trial [10]. We found that greater proportions of patients with late ICU admission used various ICU technologies; however, this meant that the absolute number of patients receiving ICU technologies was similar between late and non-late urgent ICU admissions. The inclusion of elective (scheduled or pre-planned) patients would further dilute the proportion of patients with late ICU admission amongst those receiving treatment with ICU technologies, further reducing the apparent program and system-level impacts of the sub-group of critically ill children with late ICU admission.
Third, the observation that most (n = 262, 72%) of the 365 patients dying in the hospital did not have a late ICU admission event [20] provides an explanation for the EPOCH finding of similar hospital mortality in the context of significantly reduced late ICU admission [relative risk 0.76 (95% CI 0.61–0.95)] in hospitals randomized to implement the BedsidePEWS vs. usual care [10]. Patients with late ICU admission may have constituted too small a proportion of children dying in hospital to modify overall mortality; similarly, their numbers were too small to meaningfully change ICU resource utilization. This, in addition to the lower-than-anticipated overall mortality rate, may explain the overall and subgroup findings in EPOCH that contrast with the perceptions of critical care practitioners and intensive care societies about the relevance of late ICU admission in individual patients.
These findings suggest that the sequelae of late ICU admission were significant and raise questions about the mechanisms underpinning late ICU admission and the preventability of these consequences. The observational data of this study suggest but do not demonstrate that patients with late ICU admission would benefit from earlier admission, and data from the parent EPOCH trial suggests that this benefit may not occur [10]. Hypotheses to explain these observations include (i) that severe illness may develop so rapidly that late ICU admission is not preventable, (ii) that under-recognition of and/or under-responsiveness to evolving illness creates delays and results in preventable late ICU admission, (iii) that a combination of both under-treatment and rapid illness progression occurs, and (iv) that the physical location of the patient at the time of resuscitation is less important than the severity of illness necessitating the provision of resuscitation. Our prior work suggests severe illness evolves over time and that patients with elevated severity of illness scores may improve without urgent ICU admission [13,14,15]. Prospective prediction of the “need” for ICU admission in the near-term by clinicians and severity of illness scores is challenging, and the opportunity cost of ICU admission “just-in-case” can be significant [16, 17].
There were limitations of this study. First, the focus of this study was on late ICU admission. The measure of late ICU admission we evaluated, using a Children’s Resuscitation Intensity Scale score > 2, has high face validity: the provision of ICU therapies before ICU or immediately after ICU admission is consistent with the notion that the ideal time for transfer was earlier than occurred. Informal “criteria” for urgent ICU admission probably were different in participating hospitals and may have in part been accounted for by clustering at the hospital level in analyses. Preventing late ICU admission may increase ICU admission rates. Second, we cannot be certain that all who would have benefitted from intensive care were admitted, nor that all who were admitted to intensive care benefited from ICU admission. By not excluding potentially “unnecessary” urgent ICU admissions, we may have introduced selection bias that made the comparator group—non-late ICU admissions, appear less sick and may have thus increased the apparent adverse consequences of late ICU admission. Other proposed measures of the timeliness of pediatric ICU admission suggest that many (84.5%) children acutely admitted to the ICU do not receive ICU interventions in the first 12 h of ICU admission which leads to questions about what constitutes the “ideal” time for ICU admission and what proportion of urgent ICU admissions “require” ICU interventions or “ICU care” [8].
Third, we did not have detailed data for potential confounders. We could not determine the reasoning behind urgent intensive care admission, nor details about patients who were not admitted to intensive care. We adjusted for severity of illness at ICU admission using the PIM2 score. This validated the severity of illness score that includes the most important variables ending 1 h after ICU admission. This may be a reasonable surrogate for missing confounders at the time of urgent ICU admission given its high correlation with ICU mortality and area under the receiver operating characteristic curve [21]. Its inclusion would have made results conservative—biasing toward the null. Fourth, we did not examine potential predictors of late ICU admission, which would be required to prevent this occurrence. In the EPOCH trial, implementation of the BedsidePEWS was associated with reduced late ICU admission, and therefore, implementation is one way to prevent late ICU admission [10]. Future work should explore patient characteristics, illness trajectory and prognosis, and clinician characteristics, workflows, and clinical responses that may help identify modifiable risk factors and other candidate interventions [14].
Strengths of this study include the international and multicenter prospective collection of data, the large number of patients included, and the pre-specified definition of late ICU admission using the Children’s Resuscitation Intensity Scale. Another strength is being able to adjust for the PIM2 score, a validated severity of illness score that predicts PICU mortality with an AUC of 0.90 [21]. The findings are compatible with initiatives including “right care right now” and surviving sepsis campaigns, and the Pediatric Advanced Life Support course, all emphasizing the early recognition of deteriorating patient conditions and the importance of early interventions to prevent further deterioration [19].
The findings are also compatible with mortality scoring systems used for quality-of-care assessment and as measures of the timeliness of ICU admission as predictors of subsequent death. For example, PIM2 includes data from the time of first face-to-face contact between a doctor from the ICU and the patient until one hour after admission to the ICU, including mechanical ventilation within 1 h of ICU admission and cardiac arrest prior to ICU admission, as strong predictors of higher mortality [21]. The PRISM score includes the most abnormal values in the first 12 h of PICU admission, and many of these physiological variables can be highly influenced by timely PICU admission, including systolic blood pressure, heart rate, PCO2, PaO2, blood urea nitrogen, and others [22]. Other studies have found high mortality after a cardiac arrest in the hospital wards, and a single-center study found that critical deterioration events (defined as ICU transfer with non-invasive ventilation, intubation, or vasopressor infusion within 12 h after ICU) were associated with in-hospital mortality of 19/114 (16.7%) and a mortality relative risk of 13.1 (95% CI 5.4, 32.1) compared to other PICU admissions after medical emergency team activation [8].
Conclusion
In this secondary analysis of 2502 patients in a prospective multi-center dataset, we found late admission to PICU from the inpatient hospital units was associated with significantly higher ICU and hospital mortality, greater use of ICU technologies, and longer ICU stays for individual patients. Future studies should include a focus on reasons for urgent ICU admission, a description of sick patients who were not admitted to the ICU, and an evaluation of how reducing late ICU admission can reduce ICU and hospital mortality.
Availability of data and materials
The data set is available on reasonable request to support conduct of studies to address a specific research question. Approval is contingent upon the review and approval of a proposal including analytic plan submitted for consideration to the EPOCH executive steering committee.
References
Cox JL, Lee E, Langer A, Armstrong PW, Naylor CD (1997) Time to treatment with thrombolytic therapy: determinants and effect on short-term nonfatal outcomes of acute myocardial infarction. Canadian GUSTO Investigators. Global Utilization of Streptokinase and + PA for Occluded Coronary Arteries. CMAJ 156(4):497–505
Sankey CB, McAvay G, Siner JM, Barsky CL, Chaudhry SI (2016) “Deterioration to door time”: an exploratory analysis of delays in escalation of care for hospitalized patients. J Gen Intern Med 31(8):895–900
Harris S, Singer M, Rowan K, Sanderson C (2015) Delay to admission to critical care and mortality among deteriorating ward patients in UK hospitals: a multicentre, prospective, observational cohort study. Lancet 385(Suppl 1):S40
McClain Smith M, Chumpia M, Wargo L, Nicol J, Bugnitz M (2017) Watcher initiative associated with decrease in failure to rescue events in pediatric population. Hosp Pediatr 7(12):710–715
Hillman K, Parr M, Flabouris A, Bishop G, Stewart A (2001) Redefining in-hospital resuscitation: the concept of the medical emergency team. Resuscitation 48(2):105–110
Domico MB, Ridout DA, Bronicki R, Anas NG, Cleary JP, Cappon J, Goldman AP, Brown KL (2012) The impact of mechanical ventilation time before initiation of extracorporeal life support on survival in pediatric respiratory failure: a review of the Extracorporeal Life Support Registry. Pediatr Crit Care Med 13(1):16–21
Odetola FO, Rosenberg AL, Davis M, Clark S, Dechert R, Shanley T (2008) Do outcomes vary according to the source of admission to the pediatric intensive care unit. Pediatr Crit Care Med 9(1):20–25
Bonafide CP, Roberts KE, Priestley MA, Tibbetts KM, Huang E, Nadkarni VM, Keren R (2012) Development of a pragmatic measure for evaluating and optimizing rapid response systems. Pediatrics 129(4):e874-881
Ebrahim S, Singh S, Hutchison JS, Kulkarni AV, Sananes R, Bowman KW, Parshuram CS (2013) Adaptive behavior, functional outcomes, and quality of life outcomes of children requiring urgent ICU admission. Pediatr Crit Care Med 14(1):10–18
Parshuram CS, Dryden-Palmer K, Farrell C, Gottesman R, Gray M, Hutchison JS, Helfaer M, Hunt EA, Joffe AR, Lacroix J et al (2018) Effect of a pediatric early warning system on all-cause mortality in hospitalized pediatric patients: the EPOCH randomized clinical trial. JAMA 319(10):1002–1012
Parshuram CS, Dryden-Palmer K, Farrell C, Gottesman R, Gray M, Hutchison JS, Helfaer M, Hunt E, Joffe A, Lacroix J et al (2015) Evaluating processes of care and outcomes of children in hospital (EPOCH): study protocol for a randomized controlled trial. Trials 16:245
Parshuram CS, Bayliss A, Reimer J, Middaugh K, Blanchard N (2011) Implementing the bedside paediatric early warning system in a community hospital: a prospective observational study. Paediatr Child Health 16(3):e18-22
Parshuram CS, Duncan HP, Joffe AR, Farrell CA, Lacroix JR, Middaugh KL, Hutchison JS, Wensley D, Blanchard N, Beyene J et al (2011) Multicentre validation of the bedside paediatric early warning system score: a severity of illness score to detect evolving critical illness in hospitalised children. Crit Care 15(4):R184
Gawronski O, Parshuram C, Cecchetti C, Tiozzo E, CiofiDegliAtti ML, Dall’Oglio I, Scarselletta G, Offidani C, Raponi M, Latour JM (2018) Qualitative study exploring factors influencing escalation of care of deteriorating children in a children’s hospital. BMJ Paediatr Open 2(1):e000241
Gawronski O, Latour JM, Cecchetti C, Iula A, Rava L, CiofiDegliAtti ML, Dall’Oglio I, Tiozzo E, Raponi M, Parshuram CS (2022) Escalation of care in children at high risk of clinical deterioration in a tertiary care children’s hospital using the Bedside Pediatric Early Warning System. BMC Pediatr 22(1):530
Chapman SM, Grocott MP, Franck LS (2010) Systematic review of paediatric alert criteria for identifying hospitalised children at risk of critical deterioration. Intensive Care Med 36(4):600–611
Chapman SM, Wray J, Oulton K, Peters MJ (2016) Systematic review of paediatric track and trigger systems for hospitalised children. Resuscitation 109:87–109
Nates JL, Nunnally M, Kleinpell R, Blosser S, Goldner J, Birriel B, Fowler CS, Byrum D, Miles WS, Bailey H et al (2016) ICU admission, discharge, and triage guidelines: a framework to enhance clinical operations, development of institutional policies, and further research. Crit Care Med 44(8):1553–1602
Quality initiatives: right care right now. http://www.sccm.org/Professional_Development/Quality_Initiatives/Pages/Right_Care_Right_Now.aspx
Nicoll J, Dryden-Palmer K, Frndova H, Gottesman R, Gray M, Hunt EA, Hutchison JS, Joffe AR, Lacroix J, Middaugh K et al (2021) Death and dying in hospitalized pediatric patients: a prospective multicenter, multinational study. J Palliat Med 15(2):227-33
Slater A, Shann F, Pearson G (2003) Paediatric Index of Mortality Study G: PIM2: a revised version of the paediatric index of mortality. Intensive Care Med 29(2):278–285
Pollack MM, Patel KM, Ruttimann UE (1996) PRISM III: an updated pediatric risk of mortality score. Crit Care Med 24(5):743–752
Acknowledgements
For our colleague and friend, the late Ronald Gottesman MD.
Funding
This work was in part funded by an unrestricted grant from the Gluskin Sheff and Associates Pediatric Critical Care Research Endowment. The funding agency had no role in the design, conduct, interpretation nor the decision to publish this work.
Author information
Authors and Affiliations
Consortia
Contributions
All authors made substantial contributions to the conception or design of the work and interpretation of the data, revised the work for important intellectual content, approved the version to be published, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. CP drafted the first version of the manuscript. LS and GT statistically analyzed the data.
Corresponding author
Ethics declarations
Competing interests
Christopher Parshuram is a named inventor of the Bedside Pediatric Early Warning System and has shares in a decision support company in part owned by SickKids that was established to commercialize the Bedside Pediatric Early Warning System. The other authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Joffe, A.R., Dryden-Palmer, K., Shadkowski, L. et al. Evaluating associations between late intensive care admission and mortality, intensive care days, and organ dysfunctions: a secondary analysis of data from the EPOCH cluster randomized trial. Intensive Care Med. Paediatr. Neonatal 1, 19 (2023). https://doi.org/10.1007/s44253-023-00019-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44253-023-00019-w