Abstract
Objective
To describe comprehensively the distribution and progression of high-frequency continuous vital signs monitoring data for children during critical care transport and explore associations with patient age, diagnosis, and severity of illness.
Design
Retrospective cohort study using prospectively collected vital signs monitoring data linked to patient demographic and transport data.
Setting
A regional pediatric critical care transport team based in London, England.
Patients
Critically ill children (age ≤ 18 years) transported by the Children’s Acute Transport Service (CATS) at Great Ormond Street Hospital (GOSH) between January 2016 and May 2021 with available high-frequency vital signs monitoring data.
Interventions
None.
Main results
Numeric values of heart rate (HR), blood pressure (BP), respiratory rate (RR), oxygen saturations (SpO2), and end-tidal carbon dioxide in ventilated children (etCO2) were extracted at a frequency of one value per second totalling over 40 million data points. Age-varying vital signs (HR, BP, and RR) were standardized using Z scores. The distribution of vital signs measured in the first 10 min of monitoring during transport, and their progression through the transport, were analyzed by age group, diagnosis group and severity of illness group. A complete dataset comprising linked vital signs, patient and transport data was extracted from 1711 patients (27.7% of all transported patients). The study cohort consisted predominantly of infants (median age of 6 months, IQR 0–51), and respiratory illness (36.0%) was the most frequent diagnosis group. Most patients were invasively ventilated (70.7%). The Infection group had the highest average (+ 2.5) and range (− 5 to + 9) of HR Z scores, particularly in septic children. Infants and pre-school children demonstrated a greater reduction in the HR Z score from the beginning to the end of transport compared to older children.
Conclusions
Marked differences in the distribution and progression of vital signs between age groups, diagnosis groups, and severity of illness groups were observed by analyzing the high-frequency data collected during paediatric critical care transport.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Critically ill children admitted at general hospitals frequently require emergency transport to tertiary paediatric intensive care units (PICUs) for a higher level of care [1,2,3]. Most of these transports are performed by paediatric critical care transport teams (PCCTs) who act as “mobile PICUs”, stabilize and safely transport critically ill children to PICUs [4, 5], which have been providing a better care to transported children with improved outcomes [6].
PCCTs are in an ideal position to recognize clinical deterioration early and institute critical care treatments in a timely way to improve children’s outcomes [7]. However, although vital signs, such as heart rate (HR), blood pressure (BP) and respiratory rate (RR), are monitored continuously during transport, timely recognition of deterioration (or response to treatment) can be challenging due to a variety of factors: the physically challenging environment, limited number of staff, a wide range of patient ages and diagnoses encountered, rapid changes in patient physiology, the need for urgent interventions, and cognitive overload. It means that physiological status is often assessed in ‘snapshots’ rather than the patient’s trajectory [8]. There is also scant literature on the extent to which vital signs deviate from ‘normal’ values in this population. A deeper understanding of the distribution and progression of vital signs during transport could empower PCCTs by providing valuable insights into the acceptable limits of these indicators. This knowledge would support well-informed clinical decisions and enhance the quality of care provided.
The distribution of physiological parameters has been recently described in normal children as well as in pre-hospital settings [9,10,11]. The centiles and distributions of continuously measured vital signs have been reported in hospitalized critically ill children [12, 13]. To the best of our knowledge, there are no studies that report the distribution and evolution of physiological parameters during paediatric critical care transport. In this study, we present, for the first time, a comprehensive description of the distribution and progression of continuous vital sign data collected at a high frequency of one reading per second during transport using a dataset that includes a large cohort of transported critically ill children. Additionally, we investigate variability in these data based on patient age, diagnosis, and severity of illness.
Methods
Study design and setting
The study was registered and approved by the research and innovation department at Great Ormond Street Hospital (GOSH). Formal ethical approval was waived since data were collected as part of routine care and anonymized before analysis, which was covered by generic research database approval (17/LO/0008). This was a retrospective cohort study that analyzes continuously monitored physiologic variables of critically ill children (age ≤ 18 years) transported to PICUs by the Children’s Acute Transport Service (CATS), a regional PCCT based in London, between 1 July 2016 and 30 May 2021.
Data sources
The CATS team implemented a technical solution (SwiftCare, Kinseed Limited, Uxbridge, UK) in 2016 to enable the gathering, collation, and storage of multi-parameter monitoring of numeric and waveform vital signs, such as heart rate (HR), respiratory rate (RR), systolic, mean, and diastolic blood pressure (BP) (non-invasive as well as arterial when available), oxygen saturations (SpO2), body temperature and end-tidal carbon dioxide (etCO2) during transports. Data were stored at high resolution (one data point per second for numeric vital sign). Upon the arrival of the CATS team at the patient's bedside in the referring hospital, the ambulance staff utilized a smartphone equipped with SwiftCare software to establish an automatic and wireless connection with the patient monitor (Philips Intellivue MP5, Philips, Netherlands). They recorded both numeric and waveform vital sign data continuously until the patient handover at the destination PICU.
Study data
The analyzed dataset consists of data on patient demographics, diagnosis, interventions, transport episode data, and numeric vital signs. Numeric vital sign observations were measured every second, including HR, SpO2, etCO2, RR in invasively ventilated patients RR(v) and in unventilated patients RR(u); we also analyzed non-invasive systolic, mean, and diastolic blood pressure (SBP, MBP and DBP) values measured intermittently (values were carried forward every 1 s until a new recording was made). For each transport, these granular physiological data were linked to patient and transport data extracted from the CATS electronic information system (SwiftCare, Kinseed Limited, Uxbridge, UK) such as age, gender, interventions, and primary diagnosis. Our dataset also included the Paediatric Index of Mortality 3 (PIM3) score calculated using variables collected at/around the time the CATS team arrived at the patient bedside [14]. The transport was divided into three stages: stabilization (from CATS arrival at the referring hospital to departure from the referring hospital), patient journey (from departure from referring hospital to arrival at the PICU), and handover (from arrival on PICU to leaving the PICU). The duration of each of these three stages was also ascertained. We did not consider waveform data (such as ECG data) in this initial study.
Data cleaning and analysis
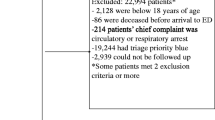
Extensive data cleaning was initially undertaken to validate and then discard implausible values for physiological variables (e.g., HR < 0 or > 300) as previously described [13]. We carried out missing value imputation, outlier detection, and data format conversion in both personal, diagnosis and transport data. Patients with missing/corrupted values that could not be recovered in patient demographics (such as age and gender), transport episode, and PIM3 score were excluded (see Online Resource 4, Supplementary Figure S1 for patient screening).
Since the cohort comprised children of different ages with different ‘normal’ ranges for vital signs, we standardized these values based on previously published normal values from healthy children by age [9]. Standardization was done using Z scores, which indicates how much a given vital sign value deviates from the mean value in healthy children of similar age and gender. Details of the Z score calculations are provided in Online Resource 1. We categorized the patient’s primary diagnosis into six major diagnosis groups (Online Resource 2). We carefully reviewed the list of detailed primary diagnosis names, sought input from the emergency transport team of clinicians and consultants, and created a limited number of major diagnosis groups that were simple, clear, and aligned with the clinical relevance of the diagnoses in our study population. The characteristics of the study cohort were described in terms of age group, diagnosis group, four most common diagnoses, and PIM3 score group.
The vital signs collected were analyzed because it can provide the transport team with valuable information about the development of diseases and children’s health conditions when the CATS team arrived at the patient's bedside. As a large majority of patients have over 10 min of vital sign monitoring data (≥ 600 data points on record), distributions of vital sign numerical values were generated using the first 10 min of monitoring time from patients (indicating patient physiology at first contact) and stratified by age, diagnosis, and PIM3 score to inspect data distributions at the very beginning time.
Progression of vital sign data over the entire transport was compared between age groups, diagnosis groups and PIM3 score groups We normalized each patient's distribution before generating the population-level distribution to avoid sampling bias due to different numbers of contributing values, which would lead to distributions weighted to represent patients with more data points. Bearing this in mind, we divided the data into consecutive non-overlapping intervals with a bin size of 5 min because 5-min resolution has been reported as an effective interval for health monitoring and deterioration prediction [15]. At the individual patient level within each 5-min bin, we calculated statistical measures for each vital sign such as mean and standard deviation (SD) of the raw values as well as the Z-score derived from the raw value. At the population-level, we calculated the mean value of each 5-min mean value from the patients in that group (see Online Resource 3 for graphical illustration of the calculation). A linear regression model was applied to determine if vital signs trends changed over transport time.
The study dataset was analyzed within the Python environment. All analysis code was written in Python 3.8. Data manipulation and analysis were done using NumPy v1.18 [16] and Pandas v1.2.4 [17]. All charts were produced with MatPlotLib v3.1.3 [18] and seaborn v0.11.1 [19]. No statistical tests were performed for this descriptive paper.
Results
Study population
Between 1 July 2016 and 30 May 2021, the CATS team transported 6470 patients to PICU, of whom 6,182 were ≤ 18 years of age and had non-missing age data. Vital sign data was not collected in all transports due to challenges such as technical issues and availability of devices. In this study, a complete dataset comprising linked vital signs, patient and transport data was available in 1711 patients (27.7%) (Online Resource 4, Supplementary Figs. 1 and 2). The 1711 patients with linked study data were not systematically different from the overall population of 6182 transported patients, see Table 1. The study cohort consisted predominantly of infants (median age of 6 months, IQR 0–51), with the most frequent diagnostic groups being respiratory (36.0%), cardiovascular (25.1%) and neurological (17.5%). Median PIM3 predicted risk of mortality was 3.4% (IQR 2.1–5.2%). Most patients were invasively ventilated (70.7%) and nearly one-third required vasoactive agents (31.7%) during transport. The median overall transport time was 208 min (IQR 165–255).
Vital sign data
A total of over 40 million data points were extracted from the study cohort. The most frequently monitored vital signs were SpO2 (88.8% of the study cohort with at least 10 min of monitoring time) and HR (88.5%), followed by RR (84.7%), SBP, DBP, and MBP (82.2%), and etCO2 (63.4%). The number of patients by age group who had continuous monitoring vital sign data and the number of available data points for each vital sign are given in Table 2 (broken down by transport stage in Online Resource 4, Supplementary Table S1). In total, 1844 h of monitoring data for HR, 1854 h for SpO2, 1623 h for SBP, 1622 h for DBP, 1633 h for MBP, 1406 h for etCO2, 1442 h for RR(v), and 324 h for RR(u) were available for analysis.
Distribution of vital signs in the first 10 min of transport
The distribution of HR, BP, and RR Z scores by diagnostic group during the first 10 min of monitoring is shown in Fig. 1—the infection and respiratory group had the highest median and range of HR Z scores, and the greatest variation in BP and RR (in unventilated children). Figure 2 shows HR, BP, and RR Z score distributions in the four most common diagnoses (congenital heart disease, bronchiolitis, status epilepticus and sepsis)—septic children had the highest mean and standard deviation of HR Z scores. Distribution of SpO2 and etCO2 values by diagnosis showed that cardiovascular diagnosis group and congenital heart disease children had the lowest median SpO2 values (due to the presence of cyanotic heart lesions in the population); etCO2 values were highest in the respiratory group, particularly the bronchiolitis population (Online Resource 4, Supplementary Figure S3). Boxplots of Z score for HR and BP by PIM3 score group are shown in Online Resource 4, Supplementary Figure S4.
Trajectory of vital signs
The progression of HR and BP Z score values during the transport by age groups is shown in Fig. 3. Trends in Z score for HR indicated that infants and pre-school children demonstrated a reduction in the HR Z-score (indicating improving physiology) from the beginning to the end of transport, more pronounced than the reduction seen in older children (Online Resource 4, Supplementary Figure S5). Compared to younger age groups, the pre-school, school child, and adolescent groups present a greater variation in HR Z score with a range between + 1 and + 4. Progression of Z-score for HR by diagnosis group, with three individual patients’ trajectories superimposed (for comparing the individual longitudinal trajectory with the population level), and for BP by diagnosis and PIM3 score groups are respectively shown in Online Resource 4, Supplementary Figs. 6, 7, and 8.
Discussion
For critically ill children, emergency pediatric transport represents a period of considerable physiological instability. In this study, we analyzed over 40 million data points to describe in detail the distribution and trajectory of commonly monitored vital signs in a large cohort of transported children. There were key differences between age groups, diagnosis groups and severity of illness groups in both the overall distribution and the progression over time of vital signs such as heart rate and blood pressure. In all age groups, but more so in pre-school and school age children, the average heart rate improved from the beginning of transport to the end of the transport, although the trajectory of individual patients was variable, with some showing little change throughout the transport.
The main strength of this study is the unique dataset of high-frequency vital sign data collected during transport; to our knowledge, this is the first description of such data in a large cohort of transported critically ill children. Even though vital signs are monitored continuously during pediatric critical care transport, these data have been seldom stored electronically and therefore there has been limited opportunity to harness them to provide computerized clinical decision support. In comparison, within the hospital setting, the increasing adoption of electronic health records (EHRs) means that vital sign data, even those collected at low frequency, have been used to predict clinical deterioration or severe sepsis for patients in inpatient settings [20, 21]. In critically ill children, low-frequency data may not adequately reflect the temporal variability and complexity of these signals; at least one report suggests that the higher the resolution of available data, the more comprehensive the description of the patient’s clinical state [22]. In our cohort, numeric data on HR, BP, RR, SpO2, and etCO2 were available at a high frequency (one value per second) in a large cohort of children allowing us to assess within- and between-patient variability.
Knowledge of the expected distribution of vital signs in the acute setting (especially during emergency transport) is important to guide clinical decisions and achieve a better understanding of vital sign interpretation. Since clinicians may choose to intervene more, or less, based on the expected range of values and their predicted trajectory. Using a target range for vital signs in a particular patient based on data from a non-critical care population could adversely impact management decisions, assessment of clinical trajectory, and potentially lead to alarm fatigue from inappropriately set limits [12]. Our data provide useful clinical insights: for example, they show that the highest HR Z scores are seen in children with infection (IQR 1.09–4.85) (especially septic patients) and those with a diagnosis of status epilepticus (IQR 0.87–3.29), and that the average set respiratory rate (median: -0.42) during ventilation is lower than the ‘normal’ value for age in all diagnosis groups. The average SpO2 in ventilated children (IQR [median]: 96.1–100 [99.4]) is higher than in children (IQR/median 95.0–100/98.5) who are spontaneously breathing. Children with a high severity of illness score (PIM3 > 0.3 IQR 0.46–2.7) have a larger variability in their HR Z score during transport unlike those with a small severity of illness score (0.01 < PIM3 ≤ 0.03 IQR0.06–3.16). Individual patient trajectories may differ from the average trajectory, and will help to spot “outliers” early.
In addition, another noteworthy aspect of strength is the provision of an alternative standardization approach for vital signs in pediatric patients using Z scores. This approach not only significantly minimizes discrepancies in age-dependent vital signs in transported children, but also assists clinicians in understanding how much the current vital sign observation deviates from the “normal” vital sign value for age in different patient cohorts, by providing both the raw vital sign value and its corresponding Z score [9]. Moreover, the transformed Z scores offer the potential to unlock the value of multiple vital sign monitoring and big data systems for clinical decision support in transport teams, by enabling the discovery of underlying patterns using large amounts of EHR data, longitudinal vital sign data, and transport episode data [23]. In future work, we plan to conduct prospective research on the impact of data-driven models such as machine learning and deep learning models, on real-time assessment of patient health deterioration during transport using our data.
Limitations
Not all transported children had data stored, raising the potential for our sample to be unrepresentative; however, we have shown that patient characteristics of the study cohort are similar to the overall transported population. The proportion of missing data was also uneven across age groups, which may have introduced bias. Another limitation is that in some cases, vital sign data did not cover the entire transport duration (at least vital signs were seldom stored electronically in some cases), i.e., it started later than the arrival of the team at the patient bedside and ended before patient handover on the PICU. Vital sign capture was not uniform among the individual vital sign measure, and the average monitoring time is around 60 min. In this study, we tried to quantify a typical monitoring time frame (e.g., first 10 min of monitoring, and 5-min monitoring interval) to observe the vital sign trends. In addition, unlike in a hospital setting, transports end when the patient reaches the PICU rather than when the patient improves sufficiently for discharge or dies, which means that it is difficult to appreciate the full trajectory of clinical improvement from transport data alone.
Conclusions
Analysis of continuously collected high-frequency data during pediatric critical care transport showed marked differences in the distribution and progression of vital signs between age groups, diagnosis groups, and severity of illness groups.
Availability of data and materials
The data that support the findings of this study are available from Children’s Acute Transport Service and Great Ormond Street Hospital in London. Restrictions apply to the availability of these data, which were used under license for this study. Data are available from the corresponding author with the permission of Great Ormond Street Hospital.
References
AAP SoTM, Romito J, Alexander SN (2015) Guidelines for Air and Ground Transport of Neonatal and Pediatric Patients Manual. American Academy of Pediatrics, Itasca
Stroud MH, Trautman MS, Meyer K et al (2013) Pediatric and neonatal interfacility transport: results from a national consensus conference. Pediatrics 132(2):359–366
Paediatric Critical Care Society (2021) Quality standards for the care of critically ill or injured children. [cited 31 May 2023]. Available from: https://pccsociety.uk/wp-content/uploads/2021/10/PCCS-Standards-2021.pdf
Ramnarayan P, Dimitriades K, Freeburn L et al (2018) Interhospital transport of critically ill children to PICUs in the United Kingdom and Republic of Ireland: analysis of an International Dataset. Pediatr Crit Care Med 19(6):e300–e311
Ramnarayan P, Polke E (2012) The state of paediatric intensive care retrieval in Britain. Arch Dis Child 97(2):145–149
Ramnarayan P, Thiru K, Parslow RC et al (2010) Effect of specialist retrieval teams on outcomes in children admitted to paediatric intensive care units in England and Wales: a retrospective cohort study. Lancet 376(9742):698–704
Ramnarayan P, Intikhab Z, Spenceley N et al (2017) (2017) Inter-hospital transport of the child with critical cardiac disease. Cardiol Young 27(S6):S40–S46
Foronda C, VanGraafeiland B, Quon R et al (2016) (2016) Handover and transport of critically ill children: an integrative review. Int J Nurs Stud 62:207–225
Fleming S, Thompson M, Stevens R et al (2011) Normal ranges of heart rate and respiratory rate in children from birth to 18 years of age: a systematic review of observational studies. Lancet 377(9770):1011–1018
Bonafide CP, Brady PW, Keren R et al (2013) Development of heart and respiratory rate percentile curves for hospitalized children. Pediatrics 131(4):e1150–1157
Nielsen VML, Klojgard T, Bruun H et al (2020) Progression of vital signs during ambulance transport categorised by a paediatric triage model: a population-based historical cohort study. BMJ Open 10(11):e042401
Eytan D, Goodwin AJ, Greer R et al (2017) Heart rate and blood pressure centile curves and distributions by age of hospitalized critically ill children. Front Pediatr 5:52
Eytan D, Goodwin AJ, Greer R et al (2018) Distributions and behavior of vital signs in critically ill children by admission diagnosis. Pediatr Crit Care Med 19(2):115–124
Straney L, Clements A, Parslow RC et al (2013) Paediatric index of mortality 3: an updated model for predicting mortality in pediatric intensive care*. Pediatr Crit Care Med 14(7):673–681
Hyland SL, Faltys M, Hüser M, Lyu X et al (2020) Early prediction of circulatory failure in the intensive care unit using machine learning. Nat Med 26(3):364–373
Van Der Walt S, Colbert SC, Varoquaux G (2011) The NumPy array: a structure for efficient numerical computation. Comput Sci Eng 13(2):22–30
McKinney W (2011) pandas: a foundational Python library for data analysis and statistics. Python High Perform Sci Comput 14(9):1–9
Hunter JD (2007) Matplotlib: a 2D graphics environment. Comput Sci Eng 9(03):90–95
Seabold S, Perktold J (2010) Statsmodels: econometric and statistical modeling with python. InProceedings of the 9th Python in Science Conference, vol 57, No. 61. pp 10–25080. https://doi.org/10.25080/Majora-92bf1922-011
Mayampurath A, Jani P, Dai Y et al (2020) A vital sign-based model to predict clinical deterioration in hospitalized children. Pediatr Crit Care Med 21(9):820–826
Kamaleswaran R, Akbilgic O, Hallman MA et al (2018) Applying artificial intelligence to identify physiomarkers predicting severe sepsis in the PICU. Pediatr Crit Care Med 19(10):e495–e503
Eytan D, Jegatheeswaran A, Mazwi ML et al (2019) Temporal variability in the sampling of vital sign data limits the accuracy of patient state estimation. Pediatr Crit Care Med 20(7):e333–e341
Mamdani M, Slutsky AS (2021) Artificial intelligence in intensive care medicine. Intensive Care Med 47(2):147–149
Acknowledgements
We would like to acknowledge support from the Kinseed, GOSH DRIVE teams, and CHIMERA for data extraction and curation. Co-author KL is supported by UK Research and Innovation (UKRI) Centre for Doctoral Training in AI -enabled healthcare systems. Co-author TM is supported by the National Institute for Health and Care Research (NIHR) Applied Research Collaboration South-West Peninsula. The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Code availability
Analysis code used in this project is available from: Zenodo: https://zenodo.org/record/8040740.
Funding
This work is supported by the Institute of Healthcare Engineering at University College London, Rosetrees Trust (Grant number: UCL-IHE-2020\102), Great Ormond Street Hospital (Charity ref.X12018) and CHIMERA (Collaborative Healthcare Innovation through Mathematics, EngineeRing and AI) Centre at UCL (EPSRC EP/T017791/1).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Zhiqiang Huo, Padmanabhan Ramnarayan, John Booth, and Kezhi Li. The first draft of the manuscript was written by Zhiqiang Huo, Padmanabhan Ramnarayan, and Kezhi Li and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Formal ethical approval was waived since data were collected as part of routine care and anonymized before analysis, which was covered by generic research database approval (17/LO/0008).
Competing interests
The authors declare they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Supplemental Online Resource 1. Z-score Standardization and Calculation Methods. Table S1. Median and 90th Centile values for HR within different age ranges. Table S2. Median and 90th Centile values for RR within different age ranges. Table S3. Median and 95th Centile values for SBP within different age ranges by male and female. Table S4. Median and 95th Centile values for DBP within different age ranges by male and female. Table S5. Median and 95th Centile values for MBP within different age ranges by male and female.
Additional file 2:
Supplemental Online Resource 2. Table S1. List of six major diagnosis groups and detailed primary diagnosis.
Additional file 3:
Supplemental Online Resource 3. Method applied to generate progression of Z-scores for vital signs over transport time.
Additional file 4:
Supplementary Digital Content 4. Supplementary Table 1. Number of patients and number of data points from continuously collected. Supplementary Figure S1. Flow diagram showing how data study data was extracted. Supplementary Figure S2. Proportion of patient transports in which continuous vital signs data monitoring was completed by year during the study period (1 July 2016 to 30 May 2021). Supplementary Figure S3. Boxplots of SpO2 and etCO2 values in the first ten min of monitoring by diagnosis group and in four common diagnoses. Supplementary Figure S4. Boxplots of Z-scores for HR, SBP, MBP and DBP in the first ten min of monitoring by PIM3 score group. Supplementary Figure S5. Linear regression of Z-scores for HR (trends on the population level) over transport time by age group. Supplementary Figure S6. Progression of Z-scores for HR over transport time (minitues) by diagnosis group, with trajectories of three individual patients superimposed (25, 50 and 75 are the 25th, 50th, 75th percentiles). Supplementary Figure S7. Progression of Z-scores for SBP, MBP and DBP over transport time (minitues) by diagnosis group (25, 50 and 75 are the 25th, 50th, 75th percentiles). Supplementary Figure S8. Progression of Z-scores for HR, SBP, MBP and DBP values over transport time (minitues) by PIM3 score group (25, 50 and 75 are the 25th, 50th, 75th percentiles).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huo, Z., Booth, J., Monks, T. et al. Distribution and trajectory of vital signs from high-frequency continuous monitoring during pediatric critical care transport. Intensive Care Med. Paediatr. Neonatal 1, 18 (2023). https://doi.org/10.1007/s44253-023-00018-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44253-023-00018-x