Abstract
The patient-centered medical home (PCMH) model has aimed to enhance chronic care in a primary care setting where providers are expected to provide timely post-discharge follow-up and decrease potentially preventable hospital readmissions through coordinated disease management. The study examined PCMH and other (risk) factors associated with 30-day unplanned readmission as well as 7- and 28-day follow-up visit with primary care providers (PCPs). We identified 8424 New York State Medicaid patients having initial stroke discharges during 2016–2018 from the Medicaid claims database and Statewide Planning and Research Cooperative System. A patient was in the PCMH group if the attributed provider had a valid National Committee for Quality Assurance PCMH recognition upon patient’s discharge. Cox regression and competing risk analyses were used to estimate the hazard ratios of readmissions and follow-up visits between PCMH and non-PCMH groups. The PCMH group had slightly but not statistically significant lower all-cause and recurrent stroke unplanned readmission rates. While the general follow-up rates between the two groups are similar, the PCMH group had significantly higher rates of stroke-specific 7-day (HR = 1.27, P < 0.01) and 28-day follow-up visits (HR = 1.22, P < 0.01). PCPs play an essential role in post stroke care. Our findings show a significantly higher rate of stroke-specific follow-up visits and a trend towards lower readmissions among patients in the PCMH group. The intervals between stroke discharge and follow-up visit time in our study population were generally greater than the recommended timeframe. We recommend the PCMH care model to improve patients’ primary care follow-up and prevent potential readmissions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Stroke is one of the leading causes of death in the United States [1]. In non-fatal cases, conditions such as persistent neurological deficits, pneumonia, chronic pain, and depression may arise and require coordination of care to maximize recovery [2,3,4,5]. Most stroke survivors experience significant challenges in the management of residual physical and emotional changes as well as prevention of recurrent stroke and control of pre-existing chronic conditions. Hence, timely follow-up is an essential component of outpatient care [6,7,8]. A previous study showed that only 5% of stroke patients had a follow-up appointment within the first week of discharge [9]. About 11–14% of stroke patients were readmitted to hospitals within 30 days [10,11,12]. Furthermore, the rate of early recurrent stroke at the first month can be as high as 1.2–4.2% [13,14,15] and is one of the top causes of unplanned readmission [16] after an initial stroke hospitalization.
Unplanned hospital readmission causes significant financial burden [17] and is potentially avoidable [18]. For stroke survivors, the mortality rate can be three times higher after a readmission [19]. To address high readmission rates, especially for chronic diseases, the Hospital Readmissions Reduction Program (HRRP) and transitional care interventions such as home visits, telemonitoring, and case management have been implemented in hospitals and healthcare systems [20,21,22]. Beside hospital-based interventions, the role of primary care providers (PCPs) has gained importance in improving the transition from hospital to home [23]. In particular, patient-centered primary care is considered a best practice for poststroke care as the process involves sequences of assessment, management, and feedback to address changing needs of the patient over time [24].
The patient-centered medical home (PCMH) is a care delivery model that puts patients at the forefront. It provides patient-centered access to care and comprehensive care coordination to achieve high-quality and cost-effective primary care. In this model, patients establish a treatment relationship with a specific PCP and obtain team-based care coordinated through this provider including specialists, hospitals, home health services, and community supports [25]. The PCMH-model is designed to reduce gaps in the transition from hospital to community level care, provides coordinated disease management for patients, and thereby should decrease hospital readmissions due to preventable disease exacerbations or complications. The PCMH model is considered an effective approach to enhance chronic care delivery in a primary care setting for patients with complex care needs.
Recent evaluations of PCMH have yielded mixed results. Previous studies reported no statistically significant positive impact of PCMH on utilization or quality outcomes [26,27,28,29]. Conversely, others have found that PCMH implementation benefits in multiple ways, such as improved quality of care and clinical outcomes, and reductions in emergency department visits, hospitalizations, and readmissions [30,31,32,33]. In particular, some studies have shown that the transformation to PCMH was associated with improvements in chronic care, healthcare utilization, and disease control [33, 34]. While most PCMH evaluations have recruited general study populations, some have focused on condition-specific outcomes such as asthma [35, 36], diabetes [37, 38], and hypertension [39, 40].
There is limited literature on the PCMH effect for patients experiencing an acute episode such as stroke that requires comprehensive coordinated care after hospital discharges. In this study, we examined the impact of PCMH among New York State Medicaid members on follow-up care utilization and unplanned hospital readmission following an initial stroke admission.
2 Methods
The study population includes New York State Medicaid members aged 18 or older having their initial stroke discharge between January 1, 2016 and December 31, 2018 and survived through discharge. Patients having stroke discharges prior to the study period were excluded from the study. Records of inpatient stays and outpatient follow-up visits between January 1, 2016 and January 31, 2019 were extracted from the New York State Department of Health Medicaid claims database. Additional hospitalization records for Medicaid-Medicare dual eligible members that were not captured in the Medicaid data system due to reimbursement regulations were obtained from New York Statewide Planning and Research Cooperative System (SPARCS). In this study, we examine healthcare utilization in the primary care setting after the end of an inpatient episode. To explicitly identify the start and end of an inpatient episode, any sequence of consecutive or overlapping inpatient records in the claims data due to transferring to other facilities or to non-acute inpatient status (e.g. rehabilitation, skill nursing facility) was concatenated into one single stay. The duration of the stay was calculated as the range between the earliest admission date and the latest discharge date among the entire inpatient stay. After this process, we only included the first stroke hospitalization that ended during the study period for each patient.
All acute and non-acute inpatient claims up to January 31, 2019 were used to identify the study population, stroke hospitalizations, and readmissions. While the study period ends on December 31, 2018, we extended the collection of inpatient claims by one month to capture 30-day readmissions. The stroke hospitalizations were identified by stroke primary diagnoses defined as ICD-9 diagnosis codes: 430.x, 431.x, 434.×1, 436.x and ICD-10 diagnosis codes: I60.x, I61.x, I63.x, I64.x. Any readmissions and follow-up visits with the above primary diagnosis codes were identified as stroke-specific events. Unplanned readmissions were those acute and not planned. Planned readmissions were defined using planned procedures and diagnoses (e.g. maintenance chemotherapy, organ transplant) following the Healthcare Effectiveness Data and Information Set (HEDIS) Plan All-Cause Readmissions (PCR) manual. Follow-up visits were defined as outpatient services rendered by PCPs who are PCMH-recognized providers, New York State designated PCPs in the Provider Network Data System (PNDS), or providers with primary taxonomy. Patients who died during a stroke hospitalization or within 30 days of discharge were excluded from the study.
Patients’ clinical characteristics before the initial stroke hospitalization were extracted from New York State Medicaid claims between October 1, 2013 and December 31, 2018, which included history of transient ischemic attack (TIA) and preexisting chronic conditions such as coronary artery disease (CAD), diabetes (DM), hypertension (HTN), heart failure (HF), and sickle cell disease (SCD). The SCD conditions were identified from the claim data by any ICD-9 and ICD-10 diagnosis codes of 282.41, 282.42, 282.6, or D57.x. Similarly, a history of TIA was identified with any ICD-9 diagnosis codes of 435.x or ICD-10 G45.x. Preexisting chronic conditions were flagged if relevant diagnoses were reported in the claims of outpatient or professional evaluation and management (E&M) services or as primary diagnoses of inpatient claims.
We attributed each patient of an index stroke hospitalization to a PCP who rendered the most primary care services for the patient during a 1-year period prior to the admission date. Observations without attributed providers were dropped from the analysis. A hospitalization was classified into the PCMH group if the attributed provider had a valid NCQA PCMH recognition with any level at the time of discharge. During the study period, providers could have been recognized under NCQA’s 2011, 2014, 2017, or NYS PCMH recognition program. The NYS PCMH recognition program is exclusive to New York State and was released on April 1, 2018. To achieve NYS PCMH recognition, practices have to complete the core criteria of the NCQA PCMH model along with 11 New York State required criteria which focus on care management and coordination, health information technology, and behavioral health.
2.1 Statistical analysis
Cox regression models were used to examine hazard ratios of 7-day and 28-day all-condition follow-up visit and 30-day all-cause unplanned readmission. Competing risk analyses were performed to assess hazard ratios of 7-day and 28-day stroke-specific follow-up visit and 30-day recurrent stroke readmission. In addition, for follow-up visit analyses, samples were right censored before the end of the observation window if a readmission was observed before any follow-up visit.
Propensity score matching method was also applied to examine the difference in 30-day unplanned readmission rates between the PCMH and non-PCMH groups, addressing potential confounding effects from the associated characteristics and risk factors. The propensity score for each patient in the two groups was estimated using a logistic regression model and then one-to-one matched with calipers equal to 0.2 [41].
Model covariates included patients’ demographics, non-dual status, history of TIA and preexisting chronic conditions, stroke type, and characteristics of the inpatient stay such as discharge year, length of stay, and hospitalization pattern which indicates whether the patient was discharged directly to home or transferred to another hospital, rehabilitation center, or skilled nursing facility before returning to home. The hospitalization pattern was included in models since it can be associated with stroke severity, care received, and outcomes [42, 43]. The differences in covariates between the PCMH and non-PCMH groups were assessed using chi-squared tests for categorical variables and t-tests for continuous variables. All analyses were conducted with SAS 9.4.
3 Results
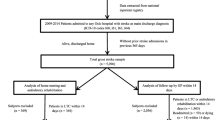
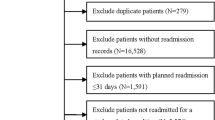
We identified 13,783 index stroke hospitalizations which included 5359 patients without attributed providers who were excluded from subsequent analyses. The final sample for readmission analyses consisted of 8424 index stroke hospitalizations, of which 4171 were contributed from patients in the PCMH group. Of 8424 index stroke hospitalizations, 5668 (PCMH n = 2906) from non-dual eligible members were used for follow-up visit analyses. We excluded dual eligible members (2756 patients) from follow-up visit analyses as their outpatient visits can be missing from Medicaid claims and such services, unlike hospitalization, are not included in SPARCS.
3.1 Demographics and clinical characteristics
Distributions of stroke patients’ demographics, medical history, and the characteristics of index stroke hospitalizations are presented in Table 1. For both readmission and follow-up visit analyses cohorts, there were no significant differences in stroke type, length of stay, discharge pattern, and history of DM, hypertension, and sickle cell disease between PCMH and non-PCMH groups. The PCMH group had higher percentage of non-White population, lower percentage of patients having pre-existing CAD, and more stroke discharges in 2018. In addition, for readmission analyses, the PCMH group had younger admitting age, larger proportion of non-dual eligible patients, and lower percentage of patients having history of HF and TIA. For follow-up visit analyses there was a higher proportion of male patients in the non-PCMH group. Table 1 also indicates that over 86% of stroke hospitalizations were due to ischemic stroke and over 80% of stroke patients in the study had hypertension.
3.2 Readmission and follow-up visits
Table 2 shows un-adjusted follow-up visit and readmission rates and adjusted hazard ratios from Cox and competing-risks regression models. The PCMH and non-PCMH groups had similar unadjusted all-condition follow-up rates that were both close to 43% within 7 days and 74% within 28 days. For stroke-specific follow-up, the unadjusted rates within 7 days were 13% for the PCMH group and 11% for non-PCMH group while within 28 days, the rates were 21% for the PCMH group and 18% for non-PCMH group. The regression results indicate the PCMH group had significantly higher rates of stroke-specific 7-day (Adjusted HR = 1.27, P < 0.01) and 28-day follow-up visits (Adjusted HR = 1.22, P < 0.01). Figure 1 shows the cumulative incidence function curve for un-adjusted follow-up visit within 28 days where the higher rate of the PCMH group remained significant after including variables listed in Table 1.
Among 4171 index stroke hospitalizations in the PCMH group, 360 (8.6%) were followed by unplanned readmissions within 30 days and 100 (2.4%) of them were due to recurrent strokes. In the non-PCMH group, there were 388 (9.1%) readmissions out of 4253 index stroke hospitalizations and 106 (2.5%) of them were due to recurrent strokes. While the results show the PCMH group had fewer 30-day readmission rates, the differences are not significant. Our results showed that individual-level risk factors associated with significantly higher risk of 30-day all-cause readmission are history of HF (HR = 1.50, P < 0.01), having been transferred to another hospital (HR = 1.43 P = 0.03), and longer length of stay (HR = 1.004, P < 0.01). Similarly, two conditions associated with a significantly higher risk for 30-day recurrent stroke readmissions are ischemic stroke (HR = 2.31, P = 0.01) and preexisting HTN (HR = 1.90, P = 0.02).
There were 3903 patients from each of the PCMH and non-PCMH group matched on the logit of propensity score. The matched PCMH group had lower rates of 30-day all-cause readmission (8.7%) and readmission caused by recurrent strokes (2.3%), compared to the non-PCMH group (9.0% for all-cause and 2.5% for recurrent stroke). However, like the findings in the survival analysis of hazard ratio, the differences were not statistically significant.
4 Discussion
This study examined the association between the PCMH model and post-stroke care quality among New York State Medicaid members in respect of follow-up visits and readmissions. Our results showed that both PCMH and non-PCMH groups had similar all-condition follow-up visit rates. The findings align with recommendations on transitions of care for stroke patients discharged from hospitals where PCPs are notified about their patients’ discharges and appropriate follow-up would be arranged in discharge planning [44,45,46]. While follow-up visit within the first month after a hospital discharge has been generally considered as standard in order to address secondary prevention, changes of medication, and functional issues [45], findings from Buletko and Khawaja suggested such follow-up timeframe may not be optimal for stroke patients from the perspective of preventable readmission reduction [8]. A study also pointed out that follow-up within 7 days after discharge would meaningfully benefit high risk patients [47]. In a stroke care study, it revealed a follow-up gap where the median number of days to the first visit with primary care among stroke patients was 22 days from discharge [48]. Our 7-day follow-up rates (43%) for both groups indicated most stroke patients in our study population had a PCP visit scheduled outside this recommended timeframe.
Although the overall follow-up visit rates between the two groups are similar, the PCMH group had significantly higher visit rates with stroke as the primary reason as compared to the non-PCMH group. A previous study [6] found that during post-stroke follow-up visits with PCPs, stroke was not necessarily the foremost concern and was not documented as an issue for most visits, revealing that stroke got limited attention in follow-up visits with PCPs during the first year after the incident. In our study, we examined stroke-specific follow-up visits within 7 days and within 28 days. Our results suggest PCMH providers are more likely to be aware of and address patients’ stroke conditions after their hospital discharges within these timeframes. As PCMH practices are required to pass all core criteria and to achieve certain minimum credits from elective criteria across six concept areas (Team-Based Care and Practice Organization, Knowing and Managing Your Patients, Patient-Centered Access and Continuity, Care Management and Support, Care Coordination and Care Transitions, and Performance Measurement and Quality Improvement), our results could be explained by some recognition criteria that facilitate health information exchange and communications between facilities, providers, and patients. The core criteria require PCMH practices to identify patients with unplanned admissions and emergency department visits as well as to contact patients for status evaluations and follow-up appointments. In addition, practices receive credits during the PCMH recognition process for the electronic health record (EHR) system adoption and demonstrating abilities to send and receive patient information during the patient’s hospitalization. These features can help PCMH providers efficiently identify changes in patients’ statuses and needs when system communication is automated and utilized. As updates of stroke conditions are delivered and acknowledged shortly after hospital discharge, PCMH providers are able to identify and address stroke management during patients’ follow-up visits.
While the study did not find a statistically significant PCMH effect on readmission measures from either the survival analysis or the propensity score methods, our Cox regression models identified additional risk factors associated with readmission. In particular, history of hypertension was associated with higher risk of recurrent stroke. This finding is consistent with previous studies that have shown management of hypertension is one risk factor to be targeted to prevent recurrence [49, 50]. Our study population had a high prevalence of hypertension history which indicates a need for secondary prevention. Beside individual-level risk factors, our results showed longer length of stay and transfer to another hospital are associated with higher risk of 30-day all-cause readmission which may indicate the presence of system issues in quality of care that could be addressed by improved care management and care coordination through the enhanced NYSPCMH model. Notably, many practices just implemented the new standard during the study period. It may require a longer time to observe the effect on readmissions and overall follow-up visits.
4.1 Limitations
This study is limited in that administrative claims do not contain patients’ clinical data. The underlying health condition upon discharge may vary between patients and contribute to outcomes observed. Additionally, our study only investigated patients’ healthcare utilization within one month following stroke discharges. Results may not be generalizable to any long-term benefit.
In this study, patients were attributed to PCPs based on their primary care services covered by Medicaid. Thus, 5359 patients (Dual-Eligible N = 1708) were excluded from analyses due to no primary care services billed to Medicaid prior to their stroke hospitalization. In addition, dual-eligible patients with primary care services partially captured in the Medicaid data may not have been attributed to the optimal PCPs who actually rendered the most primary care services. While we included both dual and non-dual patients in our readmission analyses, 2756 attributed dual patients (PCMH N = 1265) were excluded from follow-up visit analyses due to the lack of availability of follow-up service utilization data.
5 Conclusion
Primary care providers have an essential role in post-stroke care. Our findings show a significantly higher rate of stroke specific follow-up visits and a trend towards lower readmissions among patients in the PCMH group. However, the gap between stroke discharge and follow-up visit time in our study population exceeds the recommended timeframe for this population and is an opportunity for enhanced efforts to improve post discharge care. We recommend the PCMH care model to improve patient’s primary care follow-up and prevent potential readmission through enhanced health information exchange and care management and coordination.
Data availability
The study used administrative data including NYS Medicaid claims and SPARCS claims. The data is not available due to the requirement of the Health Insurance Portability and Accountability Act (HIPAA) Privacy Rule. Medicaid data can be obtained through CMS (https://data.cms.gov/). SPARCS data can be requested from the SPARCS program (https://www.health.ny.gov/statistics/sparcs/).
Code availability
Data analyses were conducted with SAS® 9.4 PHREG Procedure.
References
Xu J, Murphy SL, Kochanek KD, Arias E. Mortality in the United States, 2018. NCHS Data. 2020;78:355.
Sposato LA, Hilz MJ, Aspberg S, et al. Post-stroke cardiovascular complications and neurogenic cardiac injury: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020;76(23):27682785.
Armstrong JR, Mosher BD. Aspiration pneumonia after stroke: intervention and prevention. Neurohospitalist. 2011;1(2):85–93.
O’Donnell MJ, Diener HC, Sacco RL, et al. Chronic pain syndromes after ischemic stroke:PRoFESS trial. Stroke. 2013;44(5):1238–43.
Schwarzbach CJ, Grau AJ. Komplikationen nach Schlaganfall : Klinische Herausforderungen in der Schlaganfallnachsorge [Complications after stroke : Clinical challenges in stroke aftercare]. Nervenarzt. 2020;91(10):920–5.
Pedersen RA, Petursson H, Hetlevik I. Stroke follow-up in primary care: a prospective cohort study on guideline adherence. BMC Fam Pract. 2018;19(1):179.
Santos E, Broussy S, Lesaine E, et al. Post-stroke follow-up: Time to organize. Rev Neurol (Paris). 2019;175(1–2):59–64.
Buletko A, Khawaja Z. Timing of follow-up after acute ischemic stroke and readmissions. Neurology. 2015;84(14):154.
Nahab F, Takesaka J, Mailyan E, et al. Avoidable 30-day readmissions among patients with stroke and other cerebrovascular disease. Neurohospitalist. 2012;2(1):7–11.
Fonarow GC, Smith EE, Reeves MJ, et al. Hospital-level variation in mortality and rehospitalization for medicare beneficiaries with acute ischemic stroke. Stroke. 2011;42(1):159–66.
Bambhroliya AB, Donnelly JP, Thomas EJ, et al. Estimates and Temporal Trend for US Nationwide 30-Day hospital readmission among patients with ischemic and hemorrhagic stroke. JAMA Netw Open. 2018;1(4):e181190.
Middleton A, Kuo YF, Graham JE, et al. Readmission patterns over 90-day episodes of care among medicare fee-for-service beneficiaries discharged to post-acute care. J Am Med Dir Assoc. 2018;19(10):896–901.
Stahmeyer JT, Stubenrauch S, Geyer S, Weissenborn K, Eberhard S. The frequency and timing of recurrent stroke: an analysis of routine health insurance data. Dtsch Arztebl Int. 2019;116(42):711–7.
Khanevski AN, Bjerkreim AT, Novotny V, et al. Thirty-day recurrence after ischemic stroke or TIA. Brain Behav. 2018;8(10): e01108.
Lovett JK, Coull AJ, Rothwell PM. Early risk of recurrence by subtype of ischemic stroke in population-based incidence studies. Neurology. 2004;62(4):569–73.
Rao A, Barrow E, Vuik S, Darzi A, Aylin P. Systematic review of hospital readmissions in stroke patients. Stroke Res Treat. 2016;2016:9325368.
Friedman B, Basu J. The rate and cost of hospital readmissions for preventable conditions. Med Care Res Rev. 2004;61(2):225–40.
Goldfield NI, McCullough EC, Hughes JS, et al. Identifying potentially preventable readmissions. Health Care Financ Rev. 2008;30(1):75–91.
Nouh AM, McCormick L, Modak J, Fortunato G, Staff I. High mortality among 30-day readmission after stroke: predictors and etiologies of readmission. Front Neurol. 2017;8:632.
Joo JY, Liu MF. Effectiveness of transitional care interventions for chronic illnesses: a systematic review of reviews. Appl Nurs Res. 2021;61: 151485.
Kamermayer AK, Leasure AR, Anderson L. The effectiveness of transitions-of-care interventions in reducing hospital readmissions and mortality: a systematic review. Dimens Crit Care Nurs. 2017;36(6):311–6.
Kripalani S, Theobald CN, Anctil B, Vasilevskis EE. Reducing hospital readmission rates: current strategies and future directions. Annu Rev Med. 2014;65:471–85.
Tang N. A primary care physician’s ideal transitions of care–where’s the evidence? J Hosp Med. 2013;8(8):472–7.
Kernan WN, Viera AJ, Billinger SA, et al. Primary care of adult patients after stroke: a scientific statement from the American Heart Association/American Stroke Association. Stroke. 2021;52(9):e558–71.
O’Dell ML. What is a patient-centered medical home? Mo Med. 2016;113(4):301–4.
Veet CA, Radomski TR, D’Avella C, et al. Impact of healthcare delivery system type on clinical, utilization, and cost outcomes of patient-centered medical homes: a systematic review. J Gen Intern Med. 2020;35(4):1276–84.
Jackson GL, Powers BJ, Chatterjee R, et al. The patient centered medical home. A systematic review Ann Intern Med. 2013;158(3):169–78.
Flieger SP. Impact of a patient-centered medical home pilot on utilization, quality, and costs and variation in medical homeness. J Ambul Care Manage. 2017;40(3):228–37.
Nichols DE, Haber SG, Romaire MA, Wensky SG. Multi-Payer Advanced Primary Care Practice Evaluation Team. Changes in utilization and expenditures for medicare beneficiaries in patient-centered medical homes: findings from the multi-payer advanced primary care practice demonstration. Med Care. 2018;56(9):775–83.
Cole MB, Galarraga O, Wilson IB. The Impact of Rhode Island’s Multipayer Patient-centered Medical Home Program on Utilization and Cost of Care. Med Care. 2019;57(10):801–8.
Cuellar A, Helmchen LA, Gimm G, et al. The CareFirst Patient-centered medical home program: cost and utilization effects in its first three years. J Gen Intern Med. 2016;31(11):1382–8.
Chu LH, Tu M, Lee YC, Sood N. The impact of patient-centered medical homes on safety net clinics. Am J Manag Care. 2016;22(87):532–8.
Hearld LR, Hearld KR, Guerrazzi C. Patient-centered medical home capacity and ambulatory care utilization. Am J Med Qual. 2017;32(5):508–17.
Rosland AM, Wong E, Maciejewski M, et al. Patient-centered medical home implementation and improved chronic disease quality: a longitudinal observational study. Health Serv Res. 2018;53(4):2503–22.
Chakravorty S, Knapp CA. The impact of the patient-centered medical home on asthma-related visits to the emergency room: a fixed effects regression approach. Matern Child Health J. 2019;23(3):369–76.
Shippee ND, Finch M, Wholey DR. Assessing medical home mechanisms: certification, asthma education, and outcomes. Am J Manag Care. 2018;24(3):e79–85.
Dobbins JM, Peiper N, Jones E, Peterson LE, Phillips RL, et al. Patient-centered medical home recognition and diabetes control among health centers: exploring the role of enabling services. Popul Health Manag. 2018;21(1):6–12.
Bojadzievski T, Gabbay RA. Patient-centered medical home and diabetes. Diabetes Care. 2011;34(4):1047–53.
John JR, Tannous WK, Jones A. Effectiveness of a patient-centered medical home model of primary care versus standard care on blood pressure outcomes among hypertensive patients. Hypertens Res. 2020;43(9):892–902.
Pourat N, Chen X, Lee C, et al. Assessing the impact of patient-centered medical home principles on hypertension outcomes among patients of HRSA-Funded Health Centers. Am J Hypertens. 2019;32(4):418–25.
Austin PC. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat. 2011;10(2):150–61.
Xian Y, Thomas L, Liang L, et al. Unexplained variation for Hospitals’ use of inpatient rehabilitation and skilled nursing facilities after an acute ischemic stroke. Stroke. 2017;48(10):2836–42.
Hong I, Goodwin JS, Reistetter TA, et al. Comparison of functional status improvements among patients with stroke receiving postacute care in inpatient rehabilitation vs skilled nursing facilities. JAMA Netw Open. 2019;2(12): e1916646.
Adeoye O, Nystr¨om KV, Yavagal DR, et al. Recommendations for the Establishment of Stroke Systems of Care: A 2019 Update [published correction appears in Stroke. 2020 Apr;51(4):e70]. Stroke. 2019;50(7):e187-e210.
Mountain A, Patrice Lindsay M, Teasell R, et al. Canadian Stroke Best Practice Recommendations: Rehabilitation, Recovery, and Community Participation following Stroke. Part Two: Transitions and Community Participation Following Stroke. Int J Stroke. 2020;15(7):789–806.
Waring J, Marshall F, Bishop S, et al. An ethnographic study of knowledge sharing across the boundaries between care processes, services and organizations: the contributions to ‘safe’ hospital discharge. Southampton (UK): NIHR Journals Library. 2014.
Jackson C, Shahsahebi M, Wedlake T, DuBard C. Timeliness of outpatient follow-up: an evidence-based approach for planning after hospital discharge. Ann Fam Med. 2015;13(2):115–22.
Duncan PW, et al. Comprehensive stroke care and outcomes. Time Paradigm Shift Stroke. 2021;52(1):385–93.
Katsanos AH, Filippatou A, Manios E, et al. Blood pressure reduction and secondary stroke prevention: a systematic review and metaregression analysis of randomized clinical trials. Hypertension. 2017;69(1):171–9.
Wajngarten M, Silva GS. Hypertension and Stroke: Update on Treatment. Eur Cardiol. 2019;14(2):111–5.
Acknowledgements
The authors would like to acknowledge Raina Josberger, Alda Osinaga, Douglas Fish, and Nathan Graber of the New York State Department of Health, for their consultation, review, and edit of this work.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data extraction and analysis were performed by K-SC. The work was supervised by MW. The first draft of the manuscript was written by K-SC. All authors reviewed, commented, and edited on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics statement and consent to participate
This project does not meet the definition of research with human subjects under HHS 45 CFR 46.102.
Competing interests
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, KS., Wu, M. & Efferen, L.S. Impact of the PCMH model on post-stroke healthcare utilization. Discov Health Systems 3, 3 (2024). https://doi.org/10.1007/s44250-024-00066-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44250-024-00066-w