Abstract
Background
Reliable performance frameworks and indicators are essential for understanding the ability of public health systems to meet their mandates and to encourage ongoing learning and quality improvement. While such frameworks exist in health care, they are not well established in public health.
Methods
We conducted a scoping review of indexed and grey literature to identify quality frameworks for public health systems in Canada and comparable countries. The search included documents published in English from 2012 to May 2022 and focused on countries with similar national contexts and public health systems to Canada. Articles that focused solely on the health care system, editorials, opinions, books, correspondence, or commentaries, and those that were highly focused on a specific area of public health work that was not generalizable, were excluded. The included studies underwent thematic analysis to identify common themes.
Results
The indexed literature search yielded 420 citations, none of which met the inclusion criteria. The grey literature search identified 1500 documents, four of which originated from national-level public health organizations in England, Wales, and the United States. The identified quality frameworks varied in their goals, reflecting the role of the organization producing the document. However, several themes common to the majority of frameworks emerged, including a skilled workforce, strong leadership, effective and timely service, equity, quality improvement, close partnerships, adequate resourcing, and innovation.
Conclusion
Although the study did not identify a commonly used framework or approach, it highlights major themes that can guide the development of a suite of indicators supporting structural and process enablers and community impact to measure and report on the quality of public health systems. Notably, the study emphasizes the importance of non-peer-reviewed literature in this field and underscores the need for more transparent documentation of framework and indicator development processes. Developing reliable performance frameworks and indicators that promote ongoing learning and quality improvement is crucial for public health systems to fulfill their mandate of promoting and protecting health in the population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Background
The coronavirus disease 2019 (COVID-19) pandemic has led to renewed global interest in public health systems and their ability to address complex current and future public health challenges [1, 2]. In Canada, public health and publicly funded health systems are distinct, although they are closely related in that both are aimed at improving the health of Canadians. Public health initiatives, such as disease surveillance and health promotion, aim to prevent diseases and reduce the need for costly medical interventions, while publicly funded health services provide Canadians with access to the medical care they need when they are sick or injured, such as in hospital care [3].
Critical to understanding the ability of the public health system to meet its mandate are a performance framework and indicators that reliably measure whether or not the system is achieving what it set out to accomplish, allow for examination of performance amongst comparators, and encourage ongoing learning and quality improvement [4,5,6].
Within the health care sector, for example, hospitals and primary care [7], there is a long history of quality measurement to drive system performance. In an overview of countries in Europe, Williams and Nolte described six common domains of quality in health care, including (1) effectiveness, (2) efficiency, (3) access, (4) patient focus or responsiveness, (5) safety, and (6) equity [8]. However, quality measurement is still a developing field within public health [8]. Some relevant work to date includes that of the Public Health Quality Forum in the United States that developed a consensus statement in 2008 defining quality in public health as “the degree to which policies, programs, services and research for the population increase desired health outcomes and conditions in which the population can be healthy” [9]. They further described nine characteristics of quality in public health, including (1) population-centred, (2) equitable, (3) proactive, (4) health-promoting, (5) risk-reducing, (6) vigilant, (7) transparent, (8) effective, and (9) efficient [9]. More recently, O’Neill and colleagues conducted a qualitative study of public health system performance in Canada and identified conceptual, methodological, contextual, and infrastructure challenges in designing a performance measurement system for public health [6]. Some key challenges identified in this work included the mission and purpose of public health systems which includes a wide range of activities from health promotion to health protection and emergency response; the complexity of public health systems and actors, which involves multiple levels of government, organizations, and actors; the need for stable funding and foundational information technology to sustain a measurement system; and variation in governance and organizational structure of public health systems across jurisdictions, which make it challenging to design a performance measurement system that is flexible enough to accommodate these variations [6].
At present, there is no commonly accepted and used framework for measuring quality in public health systems. This scoping review aims to identify quality frameworks and describe key domains or components for public health systems in comparator countries.
2 Methods
We conducted a scoping review using the methods of Arksey and O’Malley [10] to identify quality frameworks for public health systems in selected comparator countries. The method consisted of six stages, including (1) identifying the research question; (2) identifying relevant literature; (3) selecting relevant literature; (4) extracting the data; (5) reporting the results. Arksey and O’Malley’s final step, consulting with stakeholders, was omitted due to capacity constraints during the COVID-19 pandemic.
2.1 Stage 1: Identifying the research question
The research question guiding the scoping review was: what frameworks have been used to assess the quality of the public health system at the national and provincial/territorial levels in Canada, and countries similar to Canada?
2.2 Stage 2: Identifying relevant literature
Public Health Ontario Library Services developed and performed the indexed and grey literature searches. MEDLINE (Ovid platform) was searched on May 16, 2022. The search strategy identified articles with at least one Medical Subject Headings (MeSH) Major Topic or title/natural language descriptor related to the concept of indicators/frameworks and at least one MeSH term or keyword in the title, natural language descriptor or abstract related to public health. Additionally, to focus the search during COVID-19, the identified articles contained at least one MeSH Major Topic or title/natural language descriptor related to health protection (i.e., control of communicable diseases, immunization, infection prevention and control, and emergency preparedness). Details of the search strategy are in Appendix A.
The grey literature was searched on May 30, 2022. The search strategy included web searches using a general search engine (Google) and two custom search engines programmed to search: 1) the websites of Canadian federal, provincial, and regional public health departments, and 2) the websites of selected international public health agencies. These programmable search engines assisted in providing customized Web searches by utilizing the Google search engine [11]. The grey literature strategies were adapted from the MEDLINE search strategy to accommodate the limitations of the search engines (e.g., 32-word limit per query), but the conceptual logic of the database search strategy was preserved. Only the first 50 results of web search queries (results sorted by relevance) were included for screening. The authors also hand-searched the reference lists of included grey literature and other articles as appropriate to identify any potentially relevant literature that had been missed in the search strategy. Details of the grey literature search strategy are in Appendix B.
Inclusion criteria included publication in English from 2012 to the time the search was performed in May 2022. We limited our searches to countries that have similar national contexts and public health systems to Canada through the use of a filter to exclude evidence from countries in Africa, the Caribbean, Central America, Latin America, South America, Asia, and Mexico, along with any articles tagged with MeSH terms for developing countries.
Additional exclusion criteria were frameworks focused solely on the health care system (e.g., hospital care); publications that took the form of an editorial, opinion, book, correspondence, or commentary; and publications that were highly focused on a specific area of public health work that were not more broadly relevant to public health systems.
2.3 Stage 3: Study selection
Included studies were determined using a three-step process. First, one reviewer (KR) screened articles and categorized them into two groups: (1) include or uncertain and (2) exclude. The documents in the include or uncertain group proceeded to the second step, where they underwent abstract or summary review by two reviewers (KR, MA). All articles that met the inclusion criteria or for which there was uncertainty proceeded to the third step of full-text screening. Any disagreement in the classification of articles at any step was discussed by the two reviewers (KR, MA). Disagreements were brought to a third reviewer (JH) to resolve through consensus-building. In addition, the second reviewer (MA) randomly reviewed 10% of all documents in the excluded group as a quality control measure.
2.4 Stage 4: Data collection and charting of the results
Data were extracted for included articles independently by two reviewers (KR, MA) and were collated in Microsoft Excel. Data extraction focused on descriptions of the frameworks, significant findings or themes, and methods if available.
2.5 Stage 5: Data summary, synthesis and report of results
Thematic analysis was performed on the included studies to identify common themes. One reviewer (KR) analyzed the information from each framework to identify common characteristics and grouped them into key themes. A second reviewer (MA) validated the findings independently by comparing the data extraction table to identified themes. Discrepancies were resolved through further discussion of all reviewers.
3 Results
The indexed literature search yielded 420 citations, with one duplicate publication identified and removed. Of the 419 publications that were included for the title and abstract screening, 34 were selected for full-text review. All of these articles were excluded primarily because they related to health care, as well as focused on quality improvement processes and were not generalizable to public health systems.
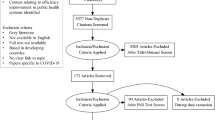
The grey literature search identified 1500 documents. After title screening, 50 documents were included for full-text review, and four documents met inclusion criteria. No additional papers for inclusion were found through reference list screening of relevant articles. Figure 1 is the PRISMA flow diagram for indexed and grey literature. The authors were not able to perform a critical appraisal of the included documents due to a lack of enough information about their methods.
3.1 General characteristics of included documents
The four documents included originated from England (n = 1), Wales (n = 1), and the United States (US) (n = 2) [12,13,14,15]. All were published by national-level public health organizations, including two led or coordinated by a government [12, 13], one by an association [14], and one by a non-governmental organization [15]. The described goals of the public health quality frameworks were diverse and reflected the role of the entity producing the document. Public Health System Group for England and Public Health Wales were most similar in their goals of improving quality in public health with a focus on people receiving services, health equity, working with partners, and good administration/governance. Although the National Association of County and City Health Officials do not clearly describe the goal of their framework, it captures some components found in the government frameworks, such as having a clear purpose and identifying user needs. It additionally provides a toolkit to implement quality by linking needs assessment, planning and improvement efforts with a strong emphasis on indicators and reporting. The goal of the Public Health Accreditation Board quality framework was very different from the other three frameworks and is intended to be used as a guidebook to support accreditation requirements. Table 1 provides additional information on the included documents.
3.2 Themes
The analysis identified thirteen themes from the included frameworks. These themes are presented from most to least common in Table 2. The only theme described in all frameworks was “skilled workforce”. For example, the Public Health System Group for England described this theme as “investment in the public health workforce and their continuous development [12].”
The next group of themes were found in the majority of frameworks (three of four). These themes included (1) strong leadership, (2) effective and timely service, (3) equity, (4) quality improvement, (5) close partnerships, (6) adequate resourcing, and (7) innovation. The strong leadership theme was linked to concepts of culture and effective governance. For example, Public Health Wales’ framework described this as “leadership and culture [13].” The effective and timely service theme contained references to responsiveness. The Public Health System Group for England also described the importance of responsiveness, with additional emphasis on this aspect across the life course [12]. The equity theme was commonly described as referring to access and usage. Both the Public Health System Group for England and Public Health Wales frameworks went beyond equity in access and described the importance of decreasing health inequities. Quality improvement was mentioned in all documents except that of the Public Health System Group for England. The Public Health Accreditation Board further made connections between some of the key themes and linked quality improvement, research and evaluation as drivers of innovation [15]. Interestingly, close partnerships were mentioned in all frameworks except that of the National Association of County and City Health Organizations. The partnership theme included concepts, such as collaboration, co-development, and public engagement. Concepts included in the adequate resourcing theme referred to financial sufficiency and sustainability, prioritization, and a strong organizational structure. The Public Health System Group for England also described the importance of prioritizing work in a deliberate way within the available resources [12]. Lastly, in this category, strong innovation was included in all the frameworks except that of the National Association of County and City Health Organizations.
The next group of themes was included in half of the frameworks (two of four): (1) assessment and evaluation, (2) measuring improvement, (3) safety, (4) evidence-informed decision-making, and (5) clear communication. Assessment and evaluation focused on community- and population-level work. Measuring improvement also overlapped with evaluation in the Public Health System Group for England framework and emphasized transparency [12]. Service user safety was mentioned in the Public Health System Group for England and Public Health Wales documents [12, 13]. Evidence-informed decision-making was present in the England and Wales frameworks [12, 13], with the Public Health System Group for England describing the importance of evidence generation and using need and evidence to inform decision-making [12]. Communication was mentioned in both the Public Health Wales and Public Health Accreditation Board frameworks [13, 15].
4 Discussion
This scoping review provides a comprehensive overview of the indexed and grey literature describing quality frameworks for public health systems. While there was no commonly used framework or approach found, we identified thirteen major themes. Derose and colleagues described a framework for local public health system quality assessment, including over-arching components of structure, process, and outcomes [27]. The thirteen themes identified in our study support their finding. The themes can be further categorized into three components, including the strength of the public health agency’s structural enablers (skilled workforce, strong leadership, adequately resourced); the process of work (quality improvement processes, close partnerships, innovation, assessment and evaluation, measuring improvement, evidence-informed decision-making); and the impact on those served (effective and timely service, equity, safety, communication) (Fig. 2). Additionally, there is significant overlap in the themes identified in our review of quality frameworks in public health and dimensions of quality frameworks described within the health care system. The US Institute of Medicine and Health Quality Ontario, Canada, both identified a number of areas of health care system quality which overlap with our findings [28, 29]. These include accessible, effective, safe, patient-centred (analogous to community needs and public engagement), equitable, efficient, and appropriately resourced.
This scoping review builds on the small body of literature describing quality frameworks for public health systems. A significant amount of knowledge on this subject is in the non-peer-reviewed literature. This scoping review benefits from a more comprehensive search of both the indexed and grey literature.
5 Limitations
This review was challenged by the paucity of literature. Additionally, the documents reviewed did not describe the methods for developing the frameworks (e.g., literature review, evaluation criteria for inclusion, who comprised decision-makers, etc.). Thus, we were unable to assess the risk of biases. This includes that quality and its underlying components may be different for practitioners, policy makers, communities, and individuals, and may also not reflect the views of those who are marginalized. We also limited our review to the English language literature and studies from countries comparable to Canada in terms of socio-demographic and public health system contexts. This may limit our findings of knowledge in this field. However, this may not reflect real-world implementation and interpretation of frameworks by different public health systems.
Future work should look to identify measures and targets of success within the identified public health quality framework themes that can be used to regularly report on public health systems.
6 Conclusions
There is an identified need for frameworks and indicators to measure and compare public health system performance within and between jurisdictions with similar socio-demographic and public health system contexts. This is especially true in the wake of the COVID-19 pandemic as public health systems support community recovery and prepare for the future. Our scoping review provides a starting point from which public health systems can develop indicators that support ongoing measurement of their quality of performance. Clear and transparent documentation of development processes and evaluation findings after implementation will further contribute to a learning public health system focused on quality.
Data availability
Contact the authors for further information.
Abbreviations
- COVID-19:
-
Coronavirus disease 2019
- MeSH:
-
Medical Subject Headings
- US:
-
United States
References
Public Health Agency of Canada. State of Public Health in Canada, 2021 [Internet]. Ottawa: Public Health Agency of Canada; 2021.
UK Government. Transforming the public health system: reforming the public health system for the challenges of our times. London: UK Government; 2021.
Government of Canada. Canada’s health care system. Ottawa: Health Canada; 2021.
National Health Service Institute for Innovation and Improvement. The good indicators guide: understanding how to use and choose indicators. London: National Health Service Institute for Innovation and Improvement; 2017.
Law M, Graham R, Bridge E, Ross K. A primer on quality in public health: What’s needed to advance CQI in Ontario public health. Qual Prim Care. 2013;21(2):93–101.
O’Neill M, De Prophetis E, Allin S, Pinto AD, Smith RW, Di Ruggiero E, Schwartz R, Pawa J, Ammi M, Rosella LC. “We cobble together a storyline of system performance using a diversity of things”: a qualitative study of perspectives on public health performance measurement in Canada. Arch Public Health. 2022;80(1):1. https://doi.org/10.1186/s13690-022-00731-3.
Braithwaite J, Hibbert P, Blakely B, Plumb J, Hannaford N, Long JC, Marks D. Health system frameworks and performance indicators in eight countries: a comparative international analysis. SAGE Open Med. 2017;4(5):2050312116686516. https://doi.org/10.1177/2050312116686516.
Williams G, Nolte E. Assuring the quality of public health services. In: organization and financing of public health services in Europe. Copenhagen: World Health Organization Regional Office for Europe; 2018.
US Department of Health and Human Services. Consensus statement on quality in the public health system. Washington: US Dept of Health and Human Services; 2008.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Google. Add a custom search engine to your site. Mountain View: Google Programmable Search Help; 2023.
Public Health System Group for England. Quality in public health: a shared responsibility. London: Public Health System Group for England; 2019.
Public Health Wales. Quality and impact framework. Wales: Public Health Wales; 2012.
National Association of County & City Health Official. Measuring what matters in public health. Washington: National Association of County & City Health Official; 2018.
Public Health Accreditation Board. Standards and measures for initial accreditation version. Washington: Public Health Accreditation Board; 2022.
Centers for Disease Control and Prevention. The 10 essential public health services: an overview. Atlanta: Centers for Disease Control and Prevention; 2021.
Tilson H, Gebbie KM. The public health workforce. Annu Rev Pub Health. 2004;25:341–56.
Canadian Public Health Association. Leadership in public health practice. Ottawa: Canadian Public Health Association; 2016.
Public Health Ontario. Health equity. Ottawa: Public Health Ontario; 2022.
Riley WJ, Moran JW, Corso LC, Beitsch LM, Bialek R, Cofsky A. Defining quality improvement in public health. J Public Health Manag Pract. 2010;16(1):5–7.
Prybil LD, Scutchfield FD, Dixon RE. The evolution of public health–hospital collaboration in the United States. Public Health Rep. 2016;131(4):522–5.
Pallipedia. Health resources. Houston: International Association for Hospice & Palliative Care; 2022.
The Public Health National Center for Innovations. Defining innovation in public health. Washington: The Public Health National Center for Innovations; 2022.
Rossi PH, Lipsey MW, Henry GT. Evaluation: A systematic approach. Thousand Oaks: Sage publications; 2018.
Mackintosh J, Ciliska D, Tulloch K. Evidence-informed decision making in public health in action. Environ Health Rev. 2015;58(1):15–9.
Winnipeg Regional Health Authority. Public Health Communication. Winnipeg: Winnipeg Regional Health Authority; 2022.
Derose SF, Schuster MA, Fielding JE, Asch SM. Public health quality measurement: concepts and challenges. Annu Rev Public Health. 2002;23(1):1–21.
Health Quality Ontario. Quality improvement. Toronto: Health Quality Ontario; 2022.
Institute of Medicine (US). Committee on quality of health care in America crossing the quality chasm: a new health system for the 21st century. Washington: National Academies Press; 2001.
Acknowledgements
Library Services, Public Health Ontario
Funding
None.
Author information
Authors and Affiliations
Contributions
JPH conceived, and JPH and MA designed the work. Acquisition and analysis of the data were performed by KR and MA. All authors contributed to the interpretation, drafting and critical revision, and gave final approval for the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate.
Not required.
Consent for publication
Consent for publication is given.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix A
Indexed literature (MEDLINE) search strategy
Ovid MEDLINE (R) ALL < 1946 to May 13, 2022 >
# | Searches | Results |
|---|---|---|
1 | *Quality Indicators, Health Care/ | 9600 |
2 | *Benchmarking/ or *Management Audit/ or *Quality Assurance, Health Care/ or *Quality Control/ or *Quality Improvement/ or *Quality of Health Care/mt, oa, st or *Total Quality Management/ | 71264 |
3 | (*Efficiency, Organizational/ or *Health Promotion/st or *Healthy People Programs/st or *Nursing Evaluation Research/ or *Population Health Management/st or *Population Health/st or *Program Evaluation/oa, mt, st or *Public Health Administration/st or *Public Health Nursing/st or *Public Health Practice/st or *Public Health/st or *Systems Analysis/ or *"Task Performance and Analysis"/) and (Benchmarking/ or Management Audit/ or Quality Assurance, Health Care/ or Quality Control/ or Quality Improvement/ or Quality Indicators, Health Care/ or Quality of Health Care/ or Total Quality Management/ or quality.kf,kw,ti.) | 4298 |
4 | Checklist/ or (scorecard* or "score card*" or "report card*" or benchmark* or "bench mark*" or ((quality or perform* or ((efficien* or effectiv*) and (program* or service* or "public health")) or accountab*) adj3 (indicator* or metric* or framework* or standard* or target or targets or index or indexes or indices or instrument or instruments or reporting or schema* or inventory or inventories)) or ((quality or perform* or ((efficien* or effectiv*) and (program* or service* or "public health")) or accountab*) adj3 (measur* or evaluat* or assess* or improv* or manag* or control* or assur* or score* or scoring or audit)) or ((quality or perform* or ((efficien* or effectiv*) and (program* or service* or "public health")) or accountab*) adj3 (tool or tools or strategy or strategies))).kf,kw,ti | 151873 |
5 | (2 or 3) and 4 | 29866 |
6 | (scorecard* or "score card*" or "report card*" or benchmark* or "bench mark*" or ((quality or perform* or ((efficien* or effectiv*) and (program* or service* or "public health")) or accountab*) adj3 (indicator* or metric* or framework* or standard* or target or targets or index or indexes or indices or instrument or instruments or reporting or schema* or inventory or inventories)) or ((quality or perform* or ((efficien* or effectiv*) and (program* or service* or "public health")) or accountab*) adj3 (measur* or evaluat* or assess* or improv* or manag* or control* or assur* or score* or scoring or audit)) or ((quality or perform* or ((efficien* or effectiv*) and (program* or service* or "public health")) or accountab*) adj3 (tool or tools or strategy or strategies))).ti | 123592 |
7 | limit 6 to ("in data review" or in process or publisher or "pubmed not medline") | 18264 |
8 | 1 or 5 or 7 | 56287 |
9 | *Public Health/ or *Public Health Administration/ or *Public Health Practice/ or *Public Health Systems Research/ or *Public Health Nursing/ or *Health Promotion/ or *United States Public Health Service/ or *"Centers for Disease Control and Prevention, U.S."/ or *Healthy People Programs/ or *Population Health/ or *Population Health Management/ or *Health Policy/ or ((*Health Education/ or *Risk Reduction Behavior/ or *Preventive Health Services/ or *Preventive Medicine/ or *Primary Prevention/ or *Public Policy/ or *Nutrition Policy/) and (Community Health Nursing/ or Community Health Planning/ or Community Health Services/ or Community Integration/ or Community Medicine/ or Community Networks/ or Community Participation/ or Community-Based Participatory Research/ or Community-Institutional Relations/ or Population Characteristics/ or Population Dynamics/ or Population Groups/ or Government Programs/ or Health Planning/ or Regional Health Planning/)) or ((Health Education/ or Risk Reduction Behavior/ or Preventive Health Services/ or Preventive Medicine/ or Primary Prevention/ or Public Policy/ or Nutrition Policy/) and (*Community Health Nursing/ or *Community Health Planning/ or *Community Health Services/ or *Community Integration/ or *Community Medicine/ or *Community Networks/ or *Community Participation/ or *Community-Based Participatory Research/ or *Community-Institutional Relations/ or *Population Characteristics/ or *Population Dynamics/ or *Population Groups/ or *Government Programs/ or *Health Planning/ or *Regional Health Planning/)) or (("public health" or "health system" or "health protection" or "population health" or "health promotion" or "health unit*" or "health authorit*" or "health department*" or (health* adj3 program*) or (health* and (communit* or population) and (educat* or program* or prevent*)) or "health region" or "health regions").ti. not medline.st.) | 186748 |
10 | *Communicable Disease Control/ or exp *Disease Outbreaks/pc or *Disease Transmission, Infectious/pc or (((communicab* or infectious*) adj3 (program* or service* or prevent* or control*)).ti. not medline.st.) | 33046 |
11 | *Epidemiology/ or *Public Health Surveillance/ or *Sentinel Surveillance/ or *Population Surveillance/ or *Epidemiological Monitoring/ or ((surveillance or epidemiol*).ti. not medline.st.) | 55530 |
12 | *Infection Control/ or ((infect* adj3 (prevent* or control)).ti. not medline.st.) | 17917 |
13 | *Immunization Programs/ or *Immunization/ or *Mass Vaccination/ or *Vaccination Coverage/ or *Vaccination/ or *Vaccine-Preventable Diseases/ or ((immuniz* or immunis* or vaccinat* or "vaccine preventable").ti. not medline.st.) | 81,578 |
14 | *Disaster Planning/ or exp *Disasters/oa, pc or *Mass Casualty Incidents/oa, pc or (*Emergencies/ not (exp Emergency Service, Hospital/ or Emergency Medical Services/ or exp Surgical Procedures, Operative/)) or (("emergency planning" or (disaster* and (plan* or prepar* or manag* or respon* or recover*)) or "emergency preparedness" or "emergency management" or "emergency response").ti. not medline.st.) | 22149 |
15 | 10 or 11 or 12 or 13 or 14 | 202194 |
16 | Public Health/ or Public Health Administration/ or Public Health Practice/ or Public Health Systems Research/ or Public Health Nursing/ or Health Promotion/ or United States Public Health Service/ or "Centers for Disease Control and Prevention, U.S."/ or Healthy People Programs/ or Population Health/ or Population Health Management/ or Health Policy/ or Health Education/ or Risk Reduction Behavior/ or Preventive Health Services/ or Preventive Medicine/ or Primary Prevention/ or Public Policy/ or Nutrition Policy/ or Community Health Nursing/ or Community Health Planning/ or Community Health Services/ or Community Integration/ or Community Medicine/ or Community Networks/ or Community Participation/ or Community-Based Participatory Research/ or Community-Institutional Relations/ or Population Characteristics/ or Population Dynamics/ or Population Groups/ or Government Programs/ or Health Planning/ or Regional Health Planning/ or ("public health" or "health system" or "health protection" or "population health" or "health promotion" or "health unit*" or "health authorit*" or "health department*" or (health* adj3 program*) or (health* and (communit* or population) and (educat* or program* or prevent*)) or "health region" or "health regions").ab,kf,kw,ti | 1046166 |
17 | 15 and 16 | 40525 |
18 | 9 or 17 | 218848 |
19 | 8 and 18 | 938 |
20 | (exp Africa/ or exp Caribbean Region/ or exp Central America/ or exp Latin America/ or exp South America/ or exp Asia/ or Mexico/ or Developing Countries/) not (North America/ or exp Canada/ or exp United States/ or exp Australia/ or New Zealand/ or exp Europe/ or exp Developed Countries/) | 1399518 |
21 | 19 not 20 | 834 |
22 | limit 21 to english | 754 |
23 | limit 22 to yr = "2012 -Current" | 423 |
24 | remove duplicates from 23 | 420 |
Appendix B:
Grey literature search strategy
4.1 Web searches (custom search engines)
Search Canadian Health Departments and Agencies| https://cse.google.com/cse?cx=54dae8807550ea08a
Search Strategy | Date Searched | # Records Reviewed |
|---|---|---|
"public health" effectiveness OR quality OR impact OR performance measure OR monitor OR assess OR evaluate OR scorecard OR report-card OR benchmark | 2022-06-13 | 50 |
health-unit OR health-authority OR health-department OR health-region or "population health" effectiveness OR quality OR impact OR performance measure OR monitor OR assess OR evaluate OR scorecard OR report-card OR benchmark | 2022-06-13 | 50 |
"public health" OR health-unit OR health-authority OR health-department OR health-region OR "population health" effectiveness OR quality OR impact OR performance indicator OR metric OR framework | 2022-06-13 | 50 |
"public health" OR health-unit OR health-authority OR health-department OR health-region OR "population health" effectiveness OR quality OR impact OR performance standards OR target OR index OR instrument OR reporting OR schema OR inventory | 2022-06-13 | 50 |
"public health" OR health-unit OR health-authority OR health-department OR health-region OR "population health" accountability OR accreditation indicator OR metric OR framework OR standards OR target OR index OR instrument OR reporting OR schema OR inventory | 2022-06-13 | 50 |
communicable OR infectious program OR service OR prevent OR control "public health" effectiveness OR quality OR impact OR performance measure OR monitor OR assess OR evaluate OR scorecard OR report-card OR benchmark | 2022-06-13 | 50 |
surveillance OR epidemiology "public health" effectiveness OR quality OR impact OR performance measure OR monitor OR assess OR evaluate OR scorecard OR report-card OR benchmark | 2022-06-13 | 50 |
infection prevention OR control "public health" effectiveness OR quality OR impact OR performance measure OR monitor OR assess OR evaluate OR scorecard OR report-card OR benchmark | 2022-06-13 | 50 |
immunization OR vaccination OR "vaccine preventable" "public health" effectiveness OR quality OR impact OR performance measure OR monitor OR assess OR evaluate OR scorecard OR report-card OR benchmark | 2022-06-13 | 50 |
"emergency planning" OR "emergency preparedness" OR "emergency management" OR "emergency response" OR disaster* planning OR preparedness OR management OR response OR recovery "public health" effectiveness OR quality OR impact OR performance measure OR monitor OR assess OR evaluate OR scorecard OR report-card OR benchmark | 2022-06-13 | 50 |
Search for International Public Health Resources | https://cse.google.com/cse?cx=b15f5d17bb6cc614d
Search Strategy | Date Searched | # Records Reviewed |
|---|---|---|
"public health" effectiveness OR quality OR impact OR performance measure OR monitor OR assess OR evaluate OR scorecard OR report-card OR benchmark | 2022-06-14 | 50 |
health-unit OR health-authority OR health-department OR health-region or "population health" effectiveness OR quality OR impact OR performance measure OR monitor OR assess OR evaluate OR scorecard OR report-card OR benchmark | 2022-06-14 | 50 |
"public health" OR health-unit OR health-authority OR health-department OR health-region OR "population health" effectiveness OR quality OR impact OR performance indicator OR metric OR framework | 2022-06-14 | 50 |
"public health" OR health-unit OR health-authority OR health-department OR health-region OR "population health" effectiveness OR quality OR impact OR performance standards OR target OR index OR instrument OR reporting OR schema OR inventory | 2022-06-14 | 50 |
"public health" OR health-unit OR health-authority OR health-department OR health-region OR "population health" accountability OR accreditation indicator OR metric OR framework OR standards OR target OR index OR instrument OR reporting OR schema OR inventory | 2022-06-14 | 50 |
communicable OR infectious program OR service OR prevent OR control "public health" effectiveness OR quality OR impact OR performance measure OR monitor OR assess OR evaluate OR scorecard OR report-card OR benchmark | 2022-06-14 | 50 |
surveillance OR epidemiology "public health" effectiveness OR quality OR impact OR performance measure OR monitor OR assess OR evaluate OR scorecard OR report-card OR benchmark | 2022-06-14 | 50 |
infection prevention OR control "public health" effectiveness OR quality OR impact OR performance measure OR monitor OR assess OR evaluate OR scorecard OR report-card OR benchmark | 2022-06-14 | 50 |
immunization OR vaccination OR "vaccine preventable" "public health" effectiveness OR quality OR impact OR performance measure OR monitor OR assess OR evaluate OR scorecard OR report-card OR benchmark | 2022-06-14 | 50 |
"emergency planning" OR "emergency preparedness" OR "emergency management" OR "emergency response" OR disaster* planning OR preparedness OR management OR response OR recovery "public health" effectiveness OR quality OR impact OR performance measure OR monitor OR assess OR evaluate OR scorecard OR report-card OR benchmark | 2022-06-14 | 50 |
Web searches (general)
Google Canada | https://www.google.ca/
Search Strategy | Date Searched | # Records Reviewed |
|---|---|---|
"public health" effectiveness OR quality OR impact OR performance measure OR monitor OR assess OR evaluate OR scorecard OR report-card OR benchmark | 2022-06-16 | 50 |
health-unit OR health-authority OR health-department OR health-region or "population health" effectiveness OR quality OR impact OR performance measure OR monitor OR assess OR evaluate OR scorecard OR report-card OR benchmark | 2022-06-16 | 50 |
"public health" OR health-unit OR health-authority OR health-department OR health-region OR "population health" effectiveness OR quality OR impact OR performance indicator OR metric OR framework | 2022-06-16 | 50 |
"public health" OR health-unit OR health-authority OR health-department OR health-region OR "population health" effectiveness OR quality OR impact OR performance standards OR target OR index OR instrument OR reporting OR schema OR inventory | 2022-06-16 | 50 |
"public health" OR health-unit OR health-authority OR health-department OR health-region OR "population health" accountability OR accreditation indicator OR metric OR framework OR standards OR target OR index OR instrument OR reporting OR schema OR inventory | 2022-06-16 | 50 |
communicable OR infectious program OR service OR prevent OR control "public health" effectiveness OR quality OR impact OR performance measure OR monitor OR assess OR evaluate OR scorecard OR report-card OR benchmark | 2022-06-16 | 50 |
surveillance OR epidemiology "public health" effectiveness OR quality OR impact OR performance measure OR monitor OR assess OR evaluate OR scorecard OR report-card OR benchmark | 2022-06-16 | 50 |
infection prevention OR control "public health" effectiveness OR quality OR impact OR performance measure OR monitor OR assess OR evaluate OR scorecard OR report-card OR benchmark | 2022-06-16 | 50 |
immunization OR vaccination OR "vaccine preventable" "public health" effectiveness OR quality OR impact OR performance measure OR monitor OR assess OR evaluate OR scorecard OR report-card OR benchmark | 2022-06-16 | 50 |
"emergency planning" OR "emergency preparedness" OR "emergency management" OR "emergency response" OR disaster* planning OR preparedness OR management OR response OR recovery "public health" effectiveness OR quality OR impact OR performance measure OR monitor OR assess OR evaluate OR scorecard OR report-card OR benchmark | 2022-06-16 | 50 |
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ramlackhan, K., Aloosh, M. & Hopkins, J.P. Public health quality frameworks: a scoping review. Discov Health Systems 2, 43 (2023). https://doi.org/10.1007/s44250-023-00057-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44250-023-00057-3