Abstract
Background
Critical care nurses are vital in the care of patients with life-threatening illnesses in intensive care units. To optimize their effectiveness, it is crucial to enhance their proficiency in professional care techniques. Implementing evidence-based training standards can improve nurses' knowledge, skills, and attitudes, ultimately enhancing healthcare services for patients.
Aim/purpose
The aim of this study protocol is to outline a series of quasi-experimental, non-randomized, single-group studies that assess the impact of standardized training courses on the development of competencies in diverse care techniques for critical care nurses.
Methodology
A comprehensive checklist will be created to evaluate nurses' professional qualifications in the specific care techniques under investigation. This checklist will be used during three expert panel sessions for each study. Nurses will then undergo theoretical and practical training to enhance their competence in implementing these techniques. To assess the training effectiveness, each nurse's competency level will be evaluated before, during, and after the training using a checklist to track their learning curve.
Results
This study will use the learning curve model to determine the optimal number of repetitions required for novice intensive care unit nurses to attain a satisfactory level of competence in each targeted care technique after training.
Conclusion
These findings could standardize nursing education practices and optimize skill practice frequency, leading to improved quality of education in the field.
Trial registration
This study is also registered at U.S. National Library of Medicine under "Clinicaltrials.gov" identifier NCT02830971, https://www.clinicaltrials.gov/ct2/show/NCT02830971, first date registered 13/07/2016 and last updated on 15/04/2021.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The Intensive Care Unit (ICU) is a specialized healthcare unit that plays a pivotal role in providing critical care to patients facing life-threatening conditions, making any medical error potentially catastrophic [1, 2]. The quality of healthcare services and treatments provided in the ICU directly impacts patients' survival rates and their overall quality of life [3, 4]. Due to the severity of their conditions or altered mental state, ICU patients heavily rely on nursing care, as they are often unable to perform even basic activities [5]. This demanding environment requires critical care nurses to exhibit complex and well-informed management skills, presenting one of the most significant professional challenges in a high-tech healthcare environment [6].
In order to address these challenges effectively, critical care nurses must possess a high level of knowledge and proficiency in a wide range of care techniques [7, 8]. Their competence, endurance, and adequate knowledge are paramount in achieving positive patient outcomes and resilience when dealing with critically ill individuals [9, 10]. Consequently, the development of knowledge and nursing care skills through standard training courses becomes imperative in enhancing the competency of critical care nurses in their professional practice [11, 12].
Standardized training courses incorporate evidence-based practices, simulations, and hands-on training to augment the competencies of nurses [13,14,15,16] and have shown promise in reducing medication errors, reducing hospital stays, and improving patient satisfaction. However, implementing standardized training courses can present certain challenges, such as time constraints, lack of comprehensive protocols, cost, and resistance to change. Addressing these challenges requires thoughtful strategies to ensure successful integration and adoption of standardized training courses for critical care nurses [17, 18].
To ensure the successful implementation of effective training courses, it is essential to consider several key factors. These factors include understanding the specific needs and requirements of the healthcare system, assessing the knowledge and experience level of the nurses, and establishing clear and measurable learning objectives. These objectives should encompass various aspects, such as the quality and frequency of training, as well as the optimal learning time needed for each technique [11]. Moreover, evaluating the quality of standardized training courses for developing competencies in diverse care techniques for critical care nurses requires careful consideration of factors like goal alignment, a comprehensive curriculum, diverse teaching strategies, experienced instructors, effective assessment methods, learner support and resources, and participant feedback. The presence of these elements plays a vital role in determining the overall quality and effectiveness of the courses in enhancing critical care nursing skills and knowledge. By incorporating these factors, training courses can be standardized and optimized to meet the diverse needs of participants, ensuring their success.
Given the significance of enhancing the competencies of critical care nurses working in the ICU, this study protocol aims to outline a robust methodology for conducting a series of semi-experimental studies. These studies seek to rigorously evaluate the impact of standardized training courses on the development of competencies in various care techniques for critical care nurses. Through a systematic approach, this research endeavors to contribute valuable insights that will pave the way for more effective and standardized nursing education, ultimately elevating the quality of critical care provided to patients.
2 Materials and Methods
2.1 Study Design
This study will employ a quasi-experimental, nonrandomized, single-group trial with a time series design to establish standard learning curves for various common care techniques in the ICU. The reporting of this study will follow the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) statement [19]. The foundation of this study is based on a previously published series of two studies on "arterial blood gas sampling" and "oral hygiene care" techniques in the ICU [20, 21], with an additional investigation of twenty other care techniques using the same methodology.
2.2 Setting
The research will be conducted in mixed medical-surgical ICUs affiliated with teaching hospitals of Tehran University of Medical Sciences (TUMS), Iran. Each ICU comprises of 10 mixed medical-surgical, with a total of 28 working nurses. The patient turnover rate in these ICUs ranges from twelve to fifteen surgical patients and three to eight medical patients per week.
2.3 Ethical Approval
The study protocol has been approved by the Ethics Committee of Hamadan University of Medical Sciences, Iran (IR.UMSHA.REC.1400.603), following the guidelines of the World Medical Association's Declaration of Helsinki [22]. Additionally, the study was presented to the research ethics committee of Tehran University of Medical Sciences (TUMS), and the research package was clearly explained to hospital authorities.
2.4 Care Techniques in ICU
A panel of ten critical care nurses collaborated to identify a comprehensive list of essential care techniques that newly registered critical care nurses should acquire competence in.
The list includes 22 techniques, such as (1) arterial blood gas (ABG) interpretation, (2) basic cardiopulmonary resuscitation (CPR), (3) advanced CPR, (4) angiocath insertion, (5) basic chest radiography interpretation, (6) performing dressings/changes, (7) drug preparation and calculation, (8) drug clinical management, (9) basic theoretical and practical mechanical ventilation, (10) advanced theoretical mechanical ventilation interpretation, (11) advanced practical mechanical ventilation interpretation, (12) basic electrocardiogram (ECG or EKG) interpretation, (13) advanced EKG interpretation, (14) foley catheter insertion, (15) general scoring (16) performing arterial blood gas, (17) laboratory test interpretation, (18) performing oral hygiene care, (19) inserting nasogastric tube, (20) serum therapy, (21) specific scoring in ICU, and (22) performing oral, endotracheal tube, and tracheostomy suctioning.
2.5 Study Population
The study includes all newly registered critical care nurses from mixed medical surgical ICUs affiliated with TUMS, Iran.
2.6 Inclusion and Exclusion Criteria
Inclusion criteria for participating in this study involve having a bachelor’s degree in nursing, being a newly registered ICU nurses, having no prior practical experience in performing ICU care techniques, not having a physical disability that would hinder skill performance, and expressing willingness to participate in the study. Nurses transferred from the ICU to other wards during the study period will be excluded.
2.7 Sample Size and Sampling Methods
A power analysis using G*Power software (latest ver. 3.1.9.7; Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany), determined that 55 participants per group are needed to achieve a 95% confidence interval level and 90% power (www.psycho.uni-duesseldorf.de/abteilungen/aap/gpower3), with an anticipated attrition rate of 10%. Hence, the study aims to recruit 60 newly registered critical care nurses. Convenience and sequential sampling methods will be used to select participants.
2.8 Informed Consent and Participant Timeline
Participants will be provided with information about the study objectives, and well-trained research assistants will obtain written informed consent from those who agree to participate. Each participant will undergo a training period ranging from 2 to 6 months. Initially, all participants will receive two weeks of theory and practice training to become familiar with the care techniques. Subsequently, their performance will be recorded and evaluated by three trained observers until they reach a score of 95% on the learning curve.
2.9 Recruitment
A research assistant, tasked with obtaining informed consent and collecting baseline data, will create a comprehensive list newly registered nurses from mixed medical-surgical ICUs affiliated with teaching hospitals of TUMS, Iran. This list, along with the inclusion criteria, will be used to identify eligible participants. This method ensures the recruitment of an adequate number of nurses for the study.
2.10 Interventions
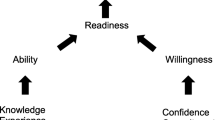
Figure 1 shows the study design steps for developing and testing a standardized learning curve to competency in professional care techniques for critical care nurses. The study involves three phases of interventions: (a) development of checklists, (b) training and (c) data collection.
2.10.1 Phase 1: Development of Checklists
A checklist will be created for each care technique to assess professional competence of critical care nurses through three expert panel sessions. The process will begin with an extensive literature review, encompassing latest documents, related articles, ICU nursing protocols, and clinical guidelines. Databases such as PubMed/MEDLINE, Scopus, Web of Science, EMBASE, ProQuest, Science Direct and nursing text books will be searched using Boolean search (AND and OR) with MeSH terms including “care techniques,” “ICU patients,” “intensive care units,” “clinical competence,” “clinical management,” “practice guideline,” “ICU nurses,” “oral hygiene,” “mouth hygiene,” “arterial blood gas,” “mechanical ventilator,” “cardiopulmonary resuscitation,” “angiocath insertion,” “chest radiography,” “electrocardiogram,” “foley catheter,” “ICU scoring,” “laboratory tests,” “nasogastric tube,” “serum therapy,” “endotracheal tube”, “tracheostomy tube”, and “suctioning.”
The development and validation of the checklist will involve three rounds of expert panels. These panels will include ten highly experienced critical care nurses (with over 20 years of experience in ICU settings) and 18 expert physicians, comprising five anesthesiologists, five internists, three pulmonologists, three intensivists, a nephrologist, and a cardiologist. During the first expert panel session, an initial draft of the checklist will be presented, followed by a 90-min discussion to achieve consensus in the first round. The primary checklist will then be shared with the expert members for further refinement, improvements, and editing. The results of the second session, lasting 120 min, will be carefully analyzed by the principal investigator and two independent researchers. Based on the outcomes of the second session, the third version of the checklist will be prepared, leading to the final version of the clinical survey checklist during the last session, which will also last 120 min.
2.10.2 Phase II: Training
A comprehensive training program will be delivered, focusing on specific care techniques and utilizing a final checklist as a guide. To ensure effective teaching and attentive participation, a comprehensive approach will be implemented, combining lecture-based sessions with face-to-face practical sessions. The training will begin with theory-based instruction, covering topics such as the physiology, anatomy, and pathophysiology related to the specific care technique. Emphasis will be placed on the importance of the care technique in preventing various diseases, particularly in ICU patients.
Subsequently, the training will progress to the introduction and explanation of the components of the final checklist. This session will provide a thorough understanding of the steps to be followed before, during, and after providing professional care. To reinforce the participants' understanding and competency, the training program includes a hands-on practical session. Under the guidance of full-time ICU instructors, nurses will have the opportunity to apply the care technique on models, simulations, and actual patients. This practical training enables participants to practice and refine their skills, ensuring their effectiveness in performing the technique. The duration of each training session may vary depending on the specific care technique, but typically a minimum of five 120-min sessions are provided. The comprehensive approach, combining theoretical knowledge and practical demonstrations, aims to equip nurses with the necessary expertise to deliver high-quality care in the ICU setting. It is important to note that the content of both theoretical and practical training sessions for each care technique will be presented in detail as separate modules, ensuring a thorough understanding and competency in each aspect of ICU care.
2.10.3 Phase III: Data Collection
2.10.3.1 Primary Outcome
The primary objective of this study is to establish standardized learning curves that determine the number of practices/attempts needed to achieve competency in each of the care techniques. The learning curve will be considered complete when a participant reaches a score of 95%. This threshold was chosen to ensure a minimal diversity of less than 5% and to effectively to flatten the learning curve.
2.10.3.2 Secondary Outcomes
In addition to establishing learning curves, this study aims to investigate the effect of sociodemographic factors such as age, gender, body max index (BMI), marriage status, as well as educational and work-related factors including grade point average (GPA), colleague’s cooperation, shift work and pre-education levels on the attainment of competence in each care technique.
2.10.3.3 Data Collection and Management
The study’s data collection will encompass recording various sociodemographic characteristics, including age, gender, BMI, and marriage status, as well as educational and work-related factors such as GPA, colleague’s cooperation, shift work, pre-education levels, major satisfaction, and supervisor. Well-trained research assistants will document this information in the case report form for each participant. In addition, after completing the training, three trained observers from ICU team will closely monitor the participants' performance of caring techniques. These observers will duly fill out checklists to assess participants’ proficiency. To minimize observer bias and its impact on participants, the scores from the first two weeks of observation will not be considered for each participant until the presence of observers becomes a routine part of the nurses’ environment. Confidentiality of all participants’ data will be strictly upheld, with hard copies of the data collection forms being securely stored in locked cabinets in the principal investigator’s office. Access to electronic clinical report forms, stored in the password-encrypted excel spreadsheets, will be restricted solely to the principal investigator and designated study team members.
2.10.3.4 Data Monitoring
A management committee (MC) and a data safety monitoring committee (DSMC) have been established to ensure transparent and safe study practices. The MC, comprising ten highly experienced critical care nurses and 18 expert physicians, will take responsibility for developing the study checklists, training the observers and critical care instructors, and monitoring the study procedures. Additionally, the MC will closely monitor the study procedures and ensure strict adherence to checklists and intervention protocols. Agreement among the panel members will be estimated using Kendall's coefficient of concordance during each session. Additionally, the content validity ratio (CVR) and content validity index (CVI) will be calculated based on input from 28 panelists for the three validation sessions. The reliability of the checklists will be assessed using the inter-rater reliability method, employing the Kappa agreement test. The principal investigator will collaborate with all members of the expert panel in this evaluation. An independent DSMC, consisting of critical care nurses, physicians, and biostatistics experts, will monitor recruitment, protocol adherence, and data collection and safety. It is important to note that this study carries minimal risk, with low adverse events. The only intervention involved will be the training provided by a full-time critical care instructor to novice critical care nurses, ensuring the standardization of care technique implementation.
2.11 Statistical Analysis
To examine the factors influencing the frequency of practices required to achieve specific levels of techniques competency, we will utilize the Poisson regression model. Nine Poisson models will be fitted to the data, corresponding to the necessary practice times to reaching skill scores of 55, 60, 65, 70, 75, 80, 85, 90, and 95. The predictable variables in these models will include GPA, gender, age, pre-education score, shift, cooperation, and supervisor. For each model (cutoff point), we will evaluate the predicted values against the actual values using the following calculation: Accuracy percentage = ((Actual times = Rounded Predicted times) / sample size) × 100. This calculation will help us determine the accuracy of the model in estimating the necessary practice times for achieving a specific level of competency. Ultimately, we will report the best-performing Poisson model based on its prediction accuracy and results [23].
We will report the average necessary practice times to reach each cutoff point, along with their distribution, through box plots. Additionally, we will present the average learning levels in two groups, categorized as high and low primary skill levels, using a learning curve diagram. The nurse’s skills will be categorized based on whether they are below average or above the average primary skill level. To assess the relative importance of the demographic variables in predicting practice scores, we will employ a linear regression using the relaimpo package in R software. The relative importance in this context refers to the resolution of R2 for the linear regression model, specifying the proportion of each variable’s contribution to the total predicted changes, with the sum of these effects equating to the R2 of the model. Larger values indicate greater importance and stronger impact of the variables on the linear model.
3 Discussion
The critical and high-stakes environment of ICUs underscores the undeniable importance and inevitability of training nurses, especially those specializing in critical care nurses [17, 24]. In light of this, the identification of training needs serves as a foundational step before initiating any training interventions at different levels and under different conditions. It is imperative for nursing education programs to be grounded in specific goals that effectively address the professional needs of providing better care. By doing so, not only can we elevate the quality of care provided to patients, but also reduce costs, enhance nurse satisfaction, and achieve organizational goals such as patient safety through comprehensive training [25, 26].
The overarching goal behind the designing of this series of quasi-experimental studies was to construct comprehensive checklists for each ICU care technique, enabling a thorough assessment of nurses’ professional competence at the three critical stages: before, during and after care. By employing these checklists and meticulously recording the learning curve, we aimed to guage the level of competence attained by nurses following training in each care technique. The insights derived from the learning curves shed light on the number of repetitions required by novice critical care nurses to attain an acceptable level of competence in each specific care technique. Such valuable information holds the potential to standardize clinical practices in nursing education and optimize the frequency of skill exercises, and thus elevating the overall quality of education in this crucial field [27,28,29,30].
The learning process for newly enrolled critical care nurses should include rapid information acquisition and frequent skill practice to achieve clinical competence [31, 32]. To achieve competence in these skills, the care process must continue until it is performed according to standards of care. Therefore, the learning curve method can be used to examine the time required to acquire clinical competence. This indicates an improvement in individual skill through repeated experiences [33, 34]. The benefits of using learning curve models in nursing education include the standardization of training through repetition of procedures and its cost-effectiveness, the reduction of patient iatrogenic injury through excessive repetition of procedures, and the improvement of training quality for nurses at all levels of initial competence [20, 21]. This scientific method is reusable and can be practiced in different educational settings for various medical skills, helping to improve the level of nursing training practice.
Evidence-based training and practice are necessary to improve quality of care, patient outcomes, and cost-effectiveness of healthcare [35]. It is considered the gold standard, providing a robust framework for providing safe and compassionate care [36]. Moreover, evidence-based training and practice encompass not only utilization of research findings, but also the development of nursing knowledge, attitudes, skills, and self-efficacy, which collectively improve the quality of the entry-level educational program in the ICU [37]. Given the critical nature of patients in the ICUs and the need for state-of-the-art facilities, experienced staff is a necessity. Understanding the extent of training and practice required for nurses to achieve professional nursing competence becomes of utmost importance to these policy makers.
4 Conclusion
The development of evidence-based training and standardized learning curves for critical care nurses in the ICU is of paramount importance to ensure the delivery of high-quality care, positive patient outcomes, and cost-effectiveness in healthcare. Implementing standardized training courses that incorporate evidence-based practices and simulations can lead to a reduction in medication errors, shorter hospital stays, and improved patient satisfaction. By identifying the necessary practice times to achieve specific levels of competency and considering various factors that influence learning, this research seeks to provide valuable insights for more effective and standardized nursing education. Ultimately, the results from this study will pave the way for elevating the quality of critical care provided to patients, ensuring that critical care nurses are fully prepared to meet the challenges of their profession with resilience and proficiency.
Availability of data and materials
Not applicable.
References
Farzi S, Irajpour A, Saghaei M, Ravaghi H. Causes of medication errors in intensive care units from the perspective of healthcare professionals. J Res Pharm Pract. 2017;6(3):158–65. https://doi.org/10.4103/jrpp.JRPP_17_47.
Camiré E, Moyen E, Stelfox HT. Medication errors in critical care: risk factors, prevention and disclosure. CMAJ. 2009;180(9):936–43. https://doi.org/10.1503/cmaj.080869.
Etemad M, Khani Y, Hashemi-Nazari S-S, Izadi N, Eshrati B, Mehrabi Y. Survival rate in patients with ICU-acquired infections and its related factors in Iran’s hospitals. BMC Public Health. 2021;21(1):787. https://doi.org/10.1186/s12889-021-10857-y.
Unal AU, Kostek O, Takir M, Caklili O, Uzunlulu M, Oguz A. Prognosis of patients in a medical intensive care unit. North Clin Istanb. 2015;2(3):189–95. https://doi.org/10.14744/nci.2015.79188.
Yang R. Dependency in critically ill patients: a meta-synthesis. Glob Qual Nurs Res. 2016;3:2333393616631677. https://doi.org/10.1177/2333393616631677.
Acebedo-Urdiales MS, Medina-Noya JL, Ferré-Grau C. Practical knowledge of experienced nurses in critical care: a qualitative study of their narratives. BMC Med Educ. 2014;14:173–173. https://doi.org/10.1186/1472-6920-14-173.
Kaldan G, Nordentoft S, Herling SF, Larsen A, Thomsen T, Egerod I. Evidence characterising skills, competencies and policies in advanced practice critical care nursing in Europe: a scoping review protocol. BMJ Open. 2019;9(9):e031504–e031504. https://doi.org/10.1136/bmjopen-2019-031504.
Alfieri E, Mori M, Barbui V, Sarli L. Advanced competencies mapping of critical care nursing: a qualitative research in two Intensive Care Units. Acta Biomed. 2017;88(3S):67–74. https://doi.org/10.23750/abm.v88i3-S.6616.
Hessels AJ, Flynn L, Cimiotti JP, Cadmus E, Gershon RRM. The impact of the nursing practice environment on missed nursing care. Clin Nurs Stud. 2015;3(4):60–5. https://doi.org/10.5430/cns.v3n4p60.
Karaca A, Durna Z. Patient satisfaction with the quality of nursing care. Nurs Open. 2019;6(2):535–45. https://doi.org/10.1002/nop2.237.
Fukada M. Nursing competency: definition, structure and development. Yonago Acta Med. 2018;61(1):1–7. https://doi.org/10.33160/yam.2018.03.001.
Mlambo M, Silén C, McGrath C. Lifelong learning and nurses’ continuing professional development, a metasynthesis of the literature. BMC Nurs. 2021;20(1):62. https://doi.org/10.1186/s12912-021-00579-2.
Recio-Saucedo A, Dall’Ora C, Maruotti A, Ball J, Briggs J, Meredith P, et al. What impact does nursing care left undone have on patient outcomes? Review of the literature. J Clin Nurs. 2018;27(11–12):2248–59. https://doi.org/10.1111/jocn.14058.
Hessels AJ, Paliwal M, Weaver SH, Siddiqui D, Wurmser TA. Impact of patient safety culture on missed nursing care and adverse patient events. J Nurs Care Qual. 2019;34(4):287–94. https://doi.org/10.1097/ncq.0000000000000378.
Kalisch BJ, Xie B, Dabney BW. Patient-reported missed nursing care correlated with adverse events. Am J Med Qual. 2014;29(5):415–22. https://doi.org/10.1177/1062860613501715.
Kalisch BJ, Landstrom G, Williams RA. Missed nursing care: errors of omission. Nurs Outlook. 2009;57(1):3–9. https://doi.org/10.1016/j.outlook.2008.05.007.
Vatani J, Javadifar S, Rabori MAS, Khanikosarkhizi Z, Bardsirii TI, Mazloumi E, et al. Training needs assessment of intensive care nurses in Zabol University of Medical Sciences’ Hospitals. J Educ Health Promot. 2021;10:85–85. https://doi.org/10.4103/jehp.jehp_60_20.
Santana-Padilla YG, Bernat-Adell MD, Santana-Cabrera L. The training needs of critical care nurses: a psychometric analysis. Sci Prog. 2022;105(1):00368504221076823. https://doi.org/10.1177/00368504221076823.
Chan A-W, Tetzlaff JM, Altman DG, Laupacis A, Gøtzsche PC, Krleža-Jerić K, et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med. 2013;158(3):200–7. https://doi.org/10.7326/0003-4819-158-3-201302050-00583.
Vahedian-Azimi A, Rahimi-Bashar F, Pourhoseingholi M-A, Salesi M, Shamsizadeh M, Jamialahmadi T, et al. Effect of the specific training course for competency in doing arterial blood gas sampling in the intensive care unit: developing a standardized learning curve according to the procedure’s time and socioprofessional predictors. Biomed Res Int. 2021;2021:2989213. https://doi.org/10.1155/2021/2989213.
Samim A, Vahedian-Azimi A, Fathi Jouzdani A, Rahimi-Bashar F. Effect of specific training course for competency in professional oral hygiene care in the intensive care unit: a quasi-experimental study for developing a standardized learning curve. BMC Anesthesiol. 2022;22(1):171. https://doi.org/10.1186/s12871-022-01709-2.
World Medical Association Declaration of Helsinki. ethical principles for medical research involving human subjects. J Am Coll Dent. 2014;81(3):14–8.
Groemping U. Relative importance for linear regression in R: the Package relaimpo. J Stat Softw. 2006;17(1):1–27. https://doi.org/10.18637/jss.v017.i01.
Khaleghi S, Sadeghi Moghaddam A, Abdolshahi A, Shokri A, Raei M, Kavari SH. Training needs assessment of nurses working at intensive care unit with the aim of designing the in-service training program. Iran J Public Health. 2020;49(11):2225–6. https://doi.org/10.18502/ijph.v49i11.4744.
Choudhary A, Gupta V. Teaching communications skills to medical students: introducing the fine art of medical practice. Int J Appl Basic Med Res. 2015;5(Suppl 1):S41–4. https://doi.org/10.4103/2229-516X.162273.
Nelson JE, Cortez TB, Curtis JR, Lustbader DR, Mosenthal AC, Mulkerin C, et al. Integrating palliative care in the ICU: the nurse in a leading role. JHPN. 2011;13(2):89–94. https://doi.org/10.1097/NJH.0b013e318203d9ff.
Howard NM, Cook DA, Hatala R, Pusic MV. Learning curves in health professions education simulation research: a systematic review. Simulat Healthc. 2021;16(2):128–35. https://doi.org/10.1097/sih.0000000000000477.
Manuel-Palazuelos JC, Riaño-Molleda M, Ruiz-Gómez JL, Martín-Parra JI, Redondo-Figuero C, Maestre JM. Learning curve patterns generated by a training method for laparoscopic small bowel anastomosis. Adv Simul (Lond). 2016;1:16–16. https://doi.org/10.1186/s41077-016-0017-y.
LeFlore JL, Thomas PE. Educational changes to support advanced practice nursing education. J Perinat Neonatal Nurs. 2016;30(3):187–90. https://doi.org/10.1097/JPN.0000000000000201.
Bosse HM, Mohr J, Buss B, Krautter M, Weyrich P, Herzog W, et al. The benefit of repetitive skills training and frequency of expert feedback in the early acquisition of procedural skills. BMC Med Educ. 2015;15:22–22. https://doi.org/10.1186/s12909-015-0286-5.
Berndtsson I, Dahlborg E, Pennbrant S. Work-integrated learning as a pedagogical tool to integrate theory and practice in nursing education—an integrative literature review. Nurse Educ Pract. 2020;42: 102685. https://doi.org/10.1016/j.nepr.2019.102685.
Thomas CM, Kellgren M. Benner’s novice to expert model: an application for simulation facilitators. Nurs Sci Q. 2017;30(3):227–34. https://doi.org/10.1177/0894318417708410.
Barrington MJ, Viero LP, Kluger R, Clarke AL, Ivanusic JJ, Wong DM. Determining the learning curve for acquiring core sonographic skills for ultrasound-guided axillary brachial plexus block. Reg Anesth Pain Med. 2016;41(6):667–70. https://doi.org/10.1097/aap.0000000000000487.
Nguyen BV, Prat G, Vincent JL, Nowak E, Bizien N, Tonnelier JM, et al. Determination of the learning curve for ultrasound-guided jugular central venous catheter placement. Intensive Care Med. 2014;40(1):66–73. https://doi.org/10.1007/s00134-013-3069-7.
Farokhzadian J, Jouparinejad S, Fatehi F, Falahati-Marvast F. Improving nurses’ readiness for evidence-based practice in critical care units: results of an information literacy training program. BMC Nurs. 2021;20(1):79. https://doi.org/10.1186/s12912-021-00599-y.
Farokhzadian J, Nayeri ND, Borhani F, Zare MR. Nurse leaders’ attitudes, self-efficancy and training needs for implementing evidence-based practice: is it time for a change toward safe care? Br J Med Med Res. 2015;7(8):662–71. https://doi.org/10.9734/bjmmr/2015/16487.
Kronenfeld M, Stephenson PL, Nail-Chiwetalu B, Tweed EM, Sauers EL, McLeod TCV, et al. Review for librarians of evidence-based practice in nursing and the allied health professions in the United States. J Med Libr Assoc. 2007;95(4):394–407. https://doi.org/10.3163/1536-5050.95.4.394.
Acknowledgements
The study was supported by Vice-chancellor for Research and Technology, Hamadan University of Medical Sciences. Moreover, thanks are due to the support, guidance, and advice from the “Clinical Research Development Unit of Baqiyatallah Hospital
Funding
The research has received a research grant by clinical research development center of Hamadan University of Medical Sciences, Hamadan, Iran. The research center has no role in the design of the study or collection, analysis, and interpretation of data.
Author information
Authors and Affiliations
Contributions
Concept and design by AV-A and VP; Acquisition of data by FR-B and KG-M; Drafting of the manuscript: VP, AA-H, and SS-C and Critical revision of the manuscript for important intellectual content by All authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose related to this study.
Ethical approval
The study protocol was approved by the Ethics Committee of Hamadan University of Medical Sciences, Hamadan, Iran (IR.UMSHA.REC.1400.603), in accordance with the Declaration of Helsinki of the World Medical Association. Further, the study was introduced with research ethics committee of Tehran University of Medical Sciences (TUMS), and the research package was explained clearly to hospital authorities.
Informed consent
Expressing ethical such as the principles of confidentiality, confidentiality of personal information and privacy of the subjects, the objectives of the study will be explained to all participants (newly registered ICU nurses) and written informed consent will be obtained from the nurses who agree to participate in this study by well-trained research assistants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pandian, V., Rahimi-Bashar, F., Gohari-Moghadam, K. et al. Impact of Evidence-Based Standardized Training on Competencies in Critical Care Nurses: A Quasi-Experimental Study Series Protocol on the Behalf of International Developing Standardized Learning Curve Team. Intensive Care Res 4, 72–79 (2024). https://doi.org/10.1007/s44231-024-00057-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44231-024-00057-8