Abstract
Infection remains a major cause of mortality in individuals diagnosed with hematologic malignancies, both in children and adults. Although the range of infections affecting these patients has undergone significant changes with the widespread use of antibiotics, it is accompanied by an increasing number of drug-resistant strains. To address these concerns, metagenomic next-generation sequencing (mNGS) has emerged as a promising diagnostic tool for detecting pathogens responsible for infectious diseases. At the same time, this approach has gained popularity as a means to identify infection etiology in hematologic disease patients. This review article focuses on the evolution of mNGS technology and its relevance in diagnosing hematologic diseases, discussing both the existing situation for microbial infections among such patients and traditional methods for detecting those infections. To examine the efficacy of this technique for hematologic disease patients, we compare the benefits and drawbacks of its application in light of relevant literature and clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
With the rapid development and cost reduction of metagenomic next-generation sequencing (mNGS), its clinical application in the field of hematology is becoming more and more extensive. In this review, we will describe the application of mNGS in hematologic malignancy through the following aspects: (a) history of mNGS development; (b) current clinical application of mNGS in hematologic malignancy;(c) the spectrum of infections in patients with hematologic malignancies; (d) advantages and limitations of using mNGS; (e) development prospects of mNGS technology.
2 Development and Current Application of mNGS
Known as high-throughput sequencing, next-generation sequencing (NGS) is a DNA sequencing technology based on PCR and gene chip. NGS has significantly transformed the field of genomic research and has been widely used in various medical fields, including personalized drug therapy, clinical diagnosis of diseases, microbiology, oncology, and many more [1].
2.1 The Development of mNGS
NGS can be divided into two major categories: metagenomics next-generation sequencing (mNGS) and targeted amplicon sequencing (TAS). They include the extraction of nucleic acid from various specimens, enrichment of the DNA and RNA, library preparation, high-throughput sequencing, and data analysis via bioinformatics. The goal of mNGS is to identify the entire DNA and RNA (reverse transcribed into cDNA) sequences using an unbiased approach to identify pathogens. It has the capability to detect all viruses, bacteria, fungi, and parasites, all in a single run. mNGS originally emerged from early metagenomics research in the 1990s, with a primary focus on studying microbial communities in environmental samples [2]. Researchers employed traditional molecular biology methods and Sanger sequencing technology in attempts to decipher the genetic information of these microorganisms. Later, in the 2000s, with the development of NGS technologies, it became feasible to conduct large-scale gene sequencing from complex samples. Subsequently, as NGS technology continued to advance, the depth and flexibility of mNGS research further strengthened. We use the form of timeline to list and describe the important literature reflecting the development of mNGS during recent twenty years (Fig. 1, [3,4,5,6,7,8]). In 2013, the case that leptospira was detected in the cerebrospinal fluid of a boy with combined immunodeficiency through NGS indicated the broad clinical application prospects of NGS [7]. The development of mNGS technology has greatly expanded our ability to study microbial communities in various environments, including the human body, and has had a profound impact on fields such as environmental science, clinical research, and microbial ecology.
2.2 The Current Application of mNGS
Currently, there are many platforms used in clinical practice, and different platforms have different detection procedures and different interpretation methods [9]. Nowadays, the most popular platforms for NGS are the MiSeq (Illumina), the Ion PGMTM (ThermoFisher) and MGISEQ. mNGS has been implemented primarily for genotyping highly resistant microorganisms and epidemic research since its application in standard diagnostics in 2014 [10]. In hematology research, mNGS was used in disease diagnosis, clinical classification, hospital-acquired infection detection, pathogen diagnosis, and resistance detection (Fig. 2). In the following, we will describe its application in pathogen diagnosis in detail.
2.3 The Bottleneck of Traditional Methods for Detecting Pathogens
Traditional methods for detecting pathogens in patients with hematologic malignancy include techniques such as the culture method, G/GM test, and PCR [11]. Culture methods rely on cultivating microbial pathogens, which usually take at least 48 h for common pathogen and longer for less common species [12]. More time is required if antibiotic susceptibility tests and identification are performed [11]. The disadvantage of PCR is that it cannot efficiently identify new or uncommon infectious species as it is a hypothesis-driven technique aimed at identifying known pathogens. Compared with the traditional methods, mNGS offers several advantages such as easy operation with a small sample size, fast detection, less risk for contamination, strong sensitivity and precise identification of marginal microorganisms that cannot be detected using traditional methods. For instance, previous research form Shenzhen Children’s Hospital has demonstrated that utilizing mNGS can significantly boost the identification of pathogens in children suffering from severe non-response pneumonia, thereby increasing the sensitivity of the pathogen identification [13].
3 Infection Status and application of the mNGS in Patients with Hematologic Malignancies
3.1 The Infection Status of Patients with Hematologic Malignancies
Patients with hematologic diseases often experience infections which can be a major contributing factor to their mortality. Based on the current research, primary causes for infection in hematologic patients include chemotherapy-induced neutropenia, invasive medical procedures, and blood transfusions [14, 15]. Infection of the bloodstream and respiratory system are the most prevalent types in these individuals. Traditional methods to identify the source of an infection are limited to detecting local infections such as ulcers, nodules or tissue necrosis in the skin or mucous membranes. However, recent studies have indicated that bacterial translocation from the gut is a significant cause of bloodstream infections due to damages in the intestinal barrier and associated lymphoid tissues in these patients [16]. Thus, a growing field of research focusing on the role of gut microbes in infections is quickly developing.
Patients with hematologic malignancies are at higher risk of developing infections, highlighting the importance of early detection of the specific pathogenic microorganisms responsible for causing such infection [17]. Proper and timely administration of effective anti-infection medications can significantly reduce patient mortality [18]. The mNGS technique has emerged as a promising tool to traditional methods for detecting infections due to its higher sensitivity and specificity, shorter detection time, and lower cost [19]. The hematology field has greatly increased the clinical application of mNGS, particularly in patients with bloodstream or respiratory infections.
3.2 Different Factors of Infection in Patients with Several Hematologic Malignancies
For patients with multiple myeloma, a pronounced depression in their primary antibody responses and anti-myeloma therapy are generally the reason for immunodeficiency. Such immunodeficiency can lead to infection, which is the primary cause for early deaths among these patients [20]. According to a Danish study, independent risk factors for bloodstream infection in multiple myeloma patients were tumor burden and aggressive disease (ISS-III and high LDH), immune dysfunction (immunoparesis) and renal impairment (high creatinine) [21]. In myelodysplastic syndromes, infection is the leading cause of death, followed by acute myeloid leukemia (AML) transformation and bleeding. Pneumonia is the most common infection observed in myelodysplastic syndrome (MDS), caused by bacteria, fungi, and viruses [22, 23]. Similarly, infection is the leading cause of death among patients with acute leukemia. Chemotherapy drugs and cancer-related immune deficiency are significant factors that increase the risk of bacterial and fungal infections in patients with acute leukemia. Almost 80% of patients undergoing chemotherapy for acute leukemia experience neutropenia symptoms, typically defined as an absolute neutrophil count (ANC) of less than 0.5 × 109/L or with a predicted decline to less than 0.5 × 109/L within the next 48-h period [24]. In individuals with AML, the occurrence rate of infection sites, ranking from the most to the least common, were the upper respiratory tract, lungs, gastrointestinal tract, perianal area, oral cavity, skin, urinary system, perineum, liver and spleen. Notably, the location of infection is more prone to match those of the previous occurrences. In cases of pulmonary infections, there is a noteworthy possibility of mixed infections, with a likelihood of up to 20.5% [25]. Hematopoietic stem cell transplantation (HSCT) is an effective treatment method for hematologic malignancies. However, infection is a frequent and recurring problem in children with acute lymphocytic leukemia (ALL) or AML, both with and without HSCT treatment. This includes infections in the respiratory and urinary tracts. Children who survive treatment have a much higher risk of death from infection when compared to the healthy children [26]. Similarly, infections are the leading cause of mortality and morbidity in adult patients following allogeneic hematopoietic stem cell transplantation(allo-HSCT) [27].
3.3 The Empiric Antibiotic Therapy in Patients with Infection
The intensity and persistence of neutropenia are closely linked to the risk of infection, particularly invasive fungal infections. As less than half of neutropenic patients exhibit a microbiologically verified illness as the root cause of their fever, empiric broad-spectrum antibiotic (BSA) therapy is the primary approach to treat febrile neutropenia (FN) [28]. Empiric BSA regimens for FN are often developed to target virulent microorganisms capable of producing life-threatening infections and those most commonly identified as the cause of fever. The coverage of resistant bacteria in the surrounding region, hospital, and department must also be considered until accurate etiological results are obtained. In pediatric leukemia patients, constant monitoring of bacteria that cause microbiotically defined bloodstream infections and their respective antibiotic sensitivity is crucial for adjusting empiric antibiotic therapy during FN episodes [20, 21]. Despite its usefulness, the use of empiric BSA therapy is not without drawbacks. Empirical medication failures are reported to be higher than before, while the application of empiric BSA leads to even more severe bacterial resistance. Prophylactic use of antibiotics has been suggested to benefit infectious complications and is linked to a clinically significant reduction in mortality [29, 30]. Furthermore, any delay in the delivery of antibiotics is associated with an extended hospital stay and a higher 30-day death rate [31].
3.4 The Application of the mNGS in Patients
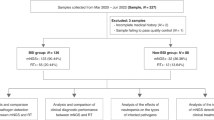
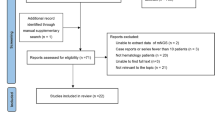
Based judge pathogenic bacteria by analyzing the DNA/RNA content and the abundance of microorganisms in mNGS specimens, it is expected to improve the sensitivity of pathogen detection, identify the bacterial drug resistance characteristics, shorten the detection time, and provide advantages in the diagnosis of rare pathogen infection. By reviewing nine articles on the pathogen detection of hematologic malignancies (Table 1), it is evident that mNGS has greater sensitivity than traditional pathogen detection methods. Therefore, mNGS is considered to be the ultimate approach to detect all microorganisms in a clinical sample [10]. This method can be used for patients who are negative for traditional culture methods and ineffective for empirical antibiotics. If pathogenic evidence is obtained, targeted drugs will benefit the patient's survival. Timely administration of antimicrobial therapy is essential for successfully managing bacterial infections. However, improper use of antibiotics can increase mortality, bacterial resistant strains, medical costs, and cause side effects. A cohort study of pediatric leukemia patients showed that antibiotic medication deescalation depending on antibiotic susceptibilities did not cause adverse complications [32].
4 The Spectrum of Infection in Patients with Hematologic Diseases
4.1 The Change of Pathogen Spectrum of Infection in Patients
In FN patients, there has been a shift in the types of bacteria responsible for infections over time. During the 1960s and 1970s, Gram negative bacteria like Escherichia coli, Klebsiella pneumoniae, and Pseudomonas aeruginosa were the primary pathogens responsible for bacteremia in these patients [33]. However, from the 1980s to the 2000s, Gram-positive bacteria became more common globally, replacing Gram-negative bacteria as the most frequent pathogens in most hospitals and institutions in Western nations [34,35,36]. However, in the 2010s, Gram-negative bacteria became a major flora of infection in FN patients with hematologic diseases again, with increased drug resistance [37]. The primary bacteria detected through traditional culture methods include Pseudomonas aeruginosa, Klebsiella pneumoniae, Escherichia coli, and so on. Moreover, neutropenic and non-neutropenic patients in the same ward significantly differ in the epidemiology and biological features of bacteria [14]. Nevertheless, the primary bacteria in both groups of patients were still mostly Gram-negative bacteria. In neutropenic childhood leukemia with fever, Gram-negative bacteria remain a significant contributor to bacterial infections, with Escherichia coli making up the largest proportion. Additionally, in a study of neutropenic patients with hematologic malignancies in Australia, Escherichia coli was also the most predominant Gram-negative bacteria, while Viridans streptococci were the most common organisms among Gram-positive bloodstream infections in neutropenic patients [38].
4.2 The Bacterial Profiles of Patients After the Application of mNGS
The recent applications of mNGS resulted in changes to the bacterial profiles as demonstrated by multiple researches. In one study published in 2019, it was found that Pseudomonas had the highest prevalence of infections under mNGS, with Acinetobacter, Klebsiella, Staphylococcus, and Xanthomonas following in proportion. On the contrary, Neisseria, Millella, Helicobacter pylori, and Mycobacterium tuberculosis were infrequent [39]. A retrospective study of 53 patients has indicated infection spectrum in which the most common group of Gram-positive bacteria was Propionibacterium acnes, Staphylococcus epidermidis, Staphylococcus hominis, the most common Gram-negative bacteria were Acinetobacter johnsonii, Burkholderia vietnamiensis [40]. The reasons for the differences observed in bacterial profiles among various studies may be due to the differences in regions and hospitals, or different methods for interpretation of mNGS results and technical processes.
4.3 The Fungal Profiles of Patients in Hematologic Malignancies
Compared to bacterial infections, fungal infections in hematologic malignancies have a lower and more stable incidence over time. However, invasive fungal disease (IFD) is common among patients with hematologic malignancies and in hematopoietic cell transplantation (HCT) recipients. Yeasts and molds are common players for causing IFD in children and teenagers undergoing intense myelo suppressive chemotherapy and in some pediatric hematopoietic stem-cell transplantation recipients. Candida and Aspergillus species are the most frequent pathogens [24]. In a study conducted in four Brazilian hematologic centers, invasive aspergillosis was found to be the leading cause of IFD, followed by invasive candidemia and fusariosis. Among all types of hematologic malignancies, AML and ALL have a high frequency of IFD burden [41]. A similar study conducted in Italy yielded identical results [42]. Though rare, there have been studies on the use of mNGS to detect invasive fungal infection in hematologic malignancies. mNGS has proven to be more sensitive than conventional microbiological tests in pulmonary IFD [43]. For instance, histopathology or the culture method is the gold standard for the diagnosis of Mucormycosis [44]. However, frequent sampling of tissue biopsy and poor positive rate of the culture create challenges for the patients, leading to a low diagnosis rate. The detection rate can be greatly improved through mNGS in peripheral blood and alveolar lavage fluid [45].
4.4 The Virus Infection of Patients with Hematologic Malignancies
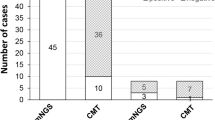
Compared to bacterial and fungal infections, hematologic malignancy patients experience lower incidence and mortality rates associated with viral infections. A widely used method for detecting viral infections is the multiplex-polymerase chain reaction (PCR), but this technique does not offer virome characterization [46]. However, NGS has become a well-established technology in viral diagnosis and is used to examine viral infections and transmission events, detect treatment sensitivity or resistance, and reveal previously unrecognized viruses [47]. Metagenomic sequencing has higher sensitivity levels for detecting low levels of viral samples. Herpes simplex and influenza viruses are primarily detected using traditional testing methods in AML patients. A study has revealed that the virus commonly detected through mNGS in patients suffering from hematologic malignancies is usually Cytomegalovirus (CMV), Epstein-Barr virus(EBV), various types of torque teno virus(TTV) [40]. This trend was also observed in patients who underwent HSCT. Another study focused on virus infection in children with acute leukemia, where articles published in English from 2000 to 2019 were analyzed. The findings showed a lower viral load in children with AML compared to those with ALL [48]. Furthermore, the mNGS method had a higher positive virus detection rate than the culture method, G/GM Test, and PCR detection. The difference between mNGS and traditional methods was statistically significant.
5 Advantages and Limitations of Using mNGS
5.1 The Advantages of the Application of mNGS
mNGS technology has various benefits such as ease of use, the capability to analyze small sample sizes, quick detection, reduced contamination risk, and the detection of microorganisms that cannot be identified through traditional methods. This technology was introduced in 2004, and since then, the cost has significantly reduced, making it an affordable and practical approach to identify and classify microorganisms in clinical patient samples [49]. The entire DNA sequence of a bacterial genome can be determined via NGS, providing information on bacteria typing, resistance and virulence, which is useful in outbreak investigations. mNGS is especially advantageous in the diagnosis of rare pathogens and those challenging to diagnose by conventional methods, for example in the detection of leishmaniasis [50]. As shown in Table 2, there are more and more reports on the diagnosis of infectious pathogens using mNGS, which highlights the importance of mNGS in the diagnosis of rare pathogens and pathogens difficult to be diagnosed by traditional methods. Additionally, this technology enables healthcare providers to understand the patient's current condition promptly and accurately, allowing for more timely antibiotic adjustments to benefit the patient's survival. It also helps to avoid the misuse of antibiotics, a prevalent problem in the healthcare industry [51].
5.2 Limitations of the Application of mNGS
Although reports of successful mNGS are available, there are several challenges that need to be addressed. These include differentiating colonization from infection, identifying extraneous sources of nucleic acid, standardizing methods, and ensuring data storage, protection, analysis, and interpretation [52]. Additionally, mNGS has revealed microbial nucleic acids in healthy individuals, raising concerns about potential contamination and the relevance of DNA found in plasma [53]. During library preparation, low-content sequences may not be amplified, leading to a loss of valuable information. Therefore, traditional PCR and cycle sequencing may be more practical for virus detection with low viral loads [9]. Illumina now produces the second-generation sequencer that is used in clinical settings the most, followed by Beijing Genomics Institute (BGI). They have different interpretation libraries of the sample data, which will cause the same sample to have different results, thus affecting the judgment of doctors. Furthermore, it has not yet been reported which indicator is most suitable for distinguishing between pathogens and colonizing/contaminant microorganisms that are present in the sample, the reagents, or the laboratory environment. Meanwhile, the majority of second-generation sequencers take more than 12 h of run time, which makes it impossible to get sequencing data in real-time [54]. The third-generation sequencing technology, which is also known as single-molecule sequencing technology, has overcome the limitation. It can detect ten nucleotides per second, which greatly reduces the time required for sequencing. Although the cost of sequencing has decreased in recent years, it is still much higher than those of conventional molecular methods and this should be taken into consideration. For example, resequencing a full viral genome by conventional cycle sequencing is generally less expensive than by using NGS methods. Likewise, detection of a known single nucleotide mutation by real-time PCR is less expensive than by using deep sequencing of amplicons [9].
6 Development Prospects of mNGS Technology
The use of mNGS may not fully replace the traditional pathogen detection methods, such as cell culture, molecular testing, and cycle sequencing. Instead, it is expected to complement these methods and serve as a powerful tool in tackling challenges associated with old and emerging pathogenic infections, which includes pathogen discovery, the analysis of intra- and inter-host pathogen variability to provide molecular epidemiology of pathogen infection, and the identification of host genetics and infectious disease susceptibility.
In the field of hematologic malignancies, mNGS technology may prove to be beneficial in determining the cause of infection and guiding treatment for patients with blood diseases. However, it should be noted that false positives and false negatives may still occur. Therefore, combining mNGS with other testing methods can reduce the risk of incorrect diagnoses.
Data Availability
Not applicable.
References
Chiu CY, Miller SA. Clinical metagenomics. Nat Rev Genet. 2019;20(6):341–55.
Schmidt TM, DeLong EF, Pace NR. Analysis of a marine picoplankton community by 16S rRNA gene cloning and sequencing. J Bacteriol. 1991;173(14):4371–8.
Rondon MR, et al. Cloning the soil metagenome: a strategy for accessing the genetic and functional diversity of uncultured microorganisms. Appl Environ Microbiol. 2000;66(6):2541–7.
Streit WR, Schmitz RA. Metagenomics – the key to the uncultured microbes. Curr Opin Microbiol. 2004;7(5):492–8.
Margulies M, et al. Genome sequencing in microfabricated high-density picolitre reactors. Nature. 2005;437(7057):376–80.
Structure, function and diversity of the healthy human microbiome. Nature, 2012. 486(7402): 207–214.
Wilson MR, et al. Actionable diagnosis of neuroleptospirosis by next-generation sequencing. N Engl J Med. 2014;370(25):2408–17.
Quick J, Quinlan AR, Loman NJ. A reference bacterial genome dataset generated on the MinION™ portable single-molecule nanopore sequencer. GigaScience. 2014;3:22.
Barzon L, et al. Next-generation sequencing technologies in diagnostic virology. J Clin Virol. 2013;58(2):346–50.
Deurenberg RH, et al. Application of next generation sequencing in clinical microbiology and infection prevention. J Biotechnol. 2017;243:16–24.
Jorgensen JH, Ferraro MJ. Antimicrobial susceptibility testing: a review of general principles and contemporary practices. Clin Infect Dis. 2009;49(11):1749–55.
Cesarman E, Chadburn A, Rubinstein PG. KSHV/HHV8-mediated hematologic diseases. Blood. 2022;139(7):1013–25.
Wang H, et al. Clinical diagnostic application of metagenomic next-generation sequencing in children with severe nonresponding pneumonia. PLoS ONE. 2020;15(6): e0232610.
Zhu J, et al. Bacterial Pathogens Differed Between Neutropenic and Non-neutropenic Patients in the Same Hematological Ward: An 8-Year Survey. Clin Infect Dis. 2018;67:S174–8.
Ainley LI, Hewitt PE. Haematology patients and the risk of transfusion transmitted infection. Br J Haematol. 2018;180(4):473–83.
Song Y, Gyarmati P. Microbiota changes in a pediatric acute lymphocytic leukemia mouse model. Microbiologyopen. 2020;9(3): e982.
Pizzo PA. Management of patients with fever and neutropenia through the arc of time: a narrative review. Ann Intern Med. 2019;170(6):389–97.
Chen W, et al. Clinical characteristics, microbiology, and risk factors for mortality of pre-engraftment and post-engraftment bloodstream infection in hematopoietic stem cell transplantation recipients. Infect Drug Resist. 2022;15:6893–905.
He Y, et al. Enhanced DNA and RNA pathogen detection via metagenomic sequencing in patients with pneumonia. J Transl Med. 2022;20(1):195.
Huang CT, et al. Risk factors and characteristics of blood stream infections in patients with newly diagnosed multiple myeloma. BMC Infect Dis. 2017;17(1):33.
Sorrig R, et al. Risk factors for blood stream infections in multiple myeloma: A population-based study of 1154 patients in Denmark. Eur J Haematol. 2018;101(1):21–7.
Toma A, et al. Infections in myelodysplastic syndromes. Haematologica. 2012;97(10):1459–70.
Caira M, Latagliata R, Girmenia C. The risk of infections in patients with myelodysplastic syndromes in 2016. Expert Rev Hematol. 2016;9(6):607–14.
Freifeld AG, et al. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the infectious diseases society of america. Clin Infect Dis. 2011;52(4):e56-93.
Hardak E, et al. Polymicrobial pulmonary infection in patients with hematological malignancies: prevalence, co-pathogens, course and outcome. Infection. 2016;44(4):491–7.
Pelland-Marcotte MC, et al. Incidence of infections after therapy completion in children with acute lymphoblastic leukemia or acute myeloid leukemia: a systematic review of the literature. Leuk Lymphoma. 2019;60(9):2104–14.
Sahin U, et al. An overview of infectious complications after allogeneic hematopoietic stem cell transplantation. J Infect Chemother. 2016;22(8):505–14.
Averbuch, D., et al., European guidelines for empirical antibacterial therapy for febrile neutropenic patients in the era of growing resistance: summary of the 2011 4th European Conference on Infections in Leukemia. Haematologica, 2013. 98(12): p. 1826–35.
Young LS. The new fluorinated quinolones for infection prevention in acute leukemia. Ann Intern Med. 1987;106(1):144–6.
Owattanapanich W, Chayakulkeeree M. Efficacy of levofloxacin as an antibacterial prophylaxis for acute leukemia patients receiving intensive chemotherapy: a systematic review and meta-analysis. Hematology. 2019;24(1):362–8.
Daniels LM, et al. Impact of time to antibiotic on hospital stay, intensive care unit admission, and mortality in febrile neutropenia. Support Care Cancer. 2019;27(11):4171–7.
Reinecke J, et al. Blood Stream Infections and Antibiotic Utilization in Pediatric Leukemia Patients With Febrile Neutropenia. J Pediatr Hematol Oncol. 2019;41(4):251–5.
Singer C, Kaplan MH, Armstrong D. Bacteremia and fungemia complicating neoplastic disease. A study of 364 cases. Am J Med. 1977;62(5):731–42.
Wisplinghoff H, et al. Current trends in the epidemiology of nosocomial bloodstream infections in patients with hematological malignancies and solid neoplasms in hospitals in the United States. Clin Infect Dis. 2003;36(9):1103–10.
Viscoli C, Castagnola E. Treatment of febrile neutropenia: what is new? Curr Opin Infect Dis. 2002;15(4):377–82.
Mebis J, et al. Long-term epidemiology of bacterial susceptibility profiles in adults suffering from febrile neutropenia with hematologic malignancy after antibiotic change. Infect Drug Resist. 2010;3:53–61.
Bassetti M, Righi E. Multidrug-resistant bacteria: what is the threat? Hematology Am Soc Hematol Educ Program. 2013;2013:428–32.
Carvalho AS, et al. Bloodstream infections in neutropenic patients with haematological malignancies. Infect Dis Health. 2020;25(1):22–9.
Li Y, et al. Microbiome profiling analysis on patients with hematological malignancies and infectious diseases by high-throughput sequencing. Chin J Experim Clin Infect Dis. 2020;14(2):99–103.
Ruli P, et al. The pathogen Spectra of infections with hematological diseaes detected using metagenomic next generation sequencing. Chinese General Practice. 2022;25(24):3022–8.
Souza L, et al. Epidemiology of invasive fungal disease in haematologic patients. Mycoses. 2021;64(3):252–6.
Pagano L, et al. The epidemiology of fungal infections in patients with hematologic malignancies: the SEIFEM-2004 study. Haematologica. 2006;91(8):1068–75.
Wang C, et al. Application of metagenomic next-generation sequencing in the diagnosis of pulmonary invasive fungal disease. Front Cell Infect Microbiol. 2022;12: 949505.
Guarner J, Brandt ME. Histopathologic diagnosis of fungal infections in the 21st century. Clin Microbiol Rev. 2011;24(2):247–80.
Zhang M, et al. Metagenomic next-generation sequencing for diagnostically challenging mucormycosis in patients with hematological malignancies. Infect Drug Resist. 2022;15:7509–17.
Ko FW, et al. Molecular detection of respiratory pathogens and typing of human rhinovirus of adults hospitalized for exacerbation of asthma and chronic obstructive pulmonary disease. Respir Res. 2019;20(1):210.
Liu B, et al. An Optimized Metagenomic Approach for Virome Detection of Clinical Pharyngeal Samples With Respiratory Infection. Front Microbiol. 2020;11:1552.
Buus-Gehrig C, et al. Systemic viral infection in children receiving chemotherapy for acute leukemia. Pediatr Blood Cancer. 2020;67(12): e28673.
Gu W, Miller S, Chiu CY. Clinical metagenomic next-generation sequencing for pathogen detection. Annu Rev Pathol. 2019;14:319–38.
Wang C, et al. Metagenomic next-generation sequencing clinches diagnosis of leishmaniasis. Lancet. 2021;397(10280):1213.
Zhang M, et al. The value of metagenomic next-generation sequencing in hematological malignancy patients with febrile neutropenia after empiric antibiotic treatment failure. Infect Drug Resist. 2022;15:3549–59.
Simner PJ, Miller S, Carroll KC. Understanding the promises and hurdles of metagenomic next-generation sequencing as a diagnostic tool for infectious diseases. Clin Infect Dis. 2018;66(5):778–88.
Gosiewski T, et al. Comprehensive detection and identification of bacterial DNA in the blood of patients with sepsis and healthy volunteers using next-generation sequencing method - the observation of DNAemia. Eur J Clin Microbiol Infect Dis. 2017;36(2):329–36.
Li N, et al. High-throughput metagenomics for identification of pathogens in the clinical settings. Small Methods. 2021;5(1):2000792.
Zhang P, et al. Metagenomic next-generation sequencing for the diagnosis of fever of unknown origin in pediatric patients with hematological malignancy. Clin Chim Acta. 2022;537:133–9.
Wang D, et al. Metagenomic next-generation sequencing successfully detects pulmonary infectious pathogens in children with hematologic malignancy. Front Cell Infect Microbiol. 2022;12: 899028.
Sun H, et al. Diagnostic value of bronchoalveolar lavage fluid metagenomic Next-generation sequencing in pneumocystis jirovecii pneumonia in Non-HIV immunosuppressed patients. Front Cell Infect Microbiol. 2022;12: 872813.
Blauwkamp TA, et al. Analytical and clinical validation of a microbial cell-free DNA sequencing test for infectious disease. Nat Microbiol. 2019;4(4):663–74.
Schulz E, et al. Pathogen detection by metagenomic next-generation sequencing during neutropenic fever in patients with hematological malignancies. Open Forum Infect Dis. 2022;9(8):ofac393.
Zhang Y, et al. Metagenomic next-generation sequencing for detection of pathogens in children with hematological diseases complicated with infection. Mol Cell Probes. 2023;67: 101889.
Shen H, et al. Clinical assessment of the utility of metagenomic next-generation sequencing in pediatric patients of hematology department. Int J Lab Hematol. 2021;43(2):244–9.
He G-Q, et al. Case report: A rare case of pulmonary mucormycosis caused by Lichtheimia ramosa in pediatric acute lymphoblastic leukemia and review of Lichtheimia infections in leukemia. Front Oncol. 2022;12: 949910.
Hu Q, et al. Case report: first report of T-cell large granular lymphocytic leukemia with NPL-DHX9 gene fusion successfully treated with cladribine: clinical experience and literature review. Front Oncol. 2022;12: 824393.
Jin Y, et al. Case report: proven diagnosis of culture-negative chronic disseminated candidiasis in a patient suffering from hematological malignancy: combined application of mngs and CFW staining. Front Med (Lausanne). 2021;8: 627166.
Ma X, et al. Invasive pulmonary aspergillosis diagnosis via peripheral blood metagenomic next-generation sequencing. Front Med (Lausanne). 2022;9: 751617.
Zhou L, et al. The successful treatment of Enterocytozoon bieneusi Microsporidiosis with nitazoxanide in a patient with B-ALL: A Case Report. Front Cell Infect Microbiol. 2022;12:1072463.
Zhang Q, et al. Nasal and cutaneous mucormycosis in two patients with lymphoma after chemotherapy and target therapy: Early detection by metagenomic next-generation sequencing. Front Cell Infect Microbiol. 2022;12: 960766.
Zhou K, et al. Case report: metagenomic next-generation sequencing can contribute to the diagnosis and treatment of disseminated visceral kaposi sarcoma following allogeneic haematopoietic stem cell transplantation. Front Oncol. 2022;12: 848976.
Wang N, et al. Case report and literature review: disseminated histoplasmosis infection diagnosed by metagenomic next-generation sequencing. Infect Drug Resist. 2022;15:4507–14.
Garnica M, et al. Metagenomic next-generation sequencing (mNGS) for diagnostically challenging infectious diseases in patients with acute leukemia. Braz J Infect Dis. 2021;25(2): 101548.
Wang Z, et al. Tuberculosis infection related hemophagocytic lymphohistiocytosis diagnosed in patient with GZMB mutation: A case report and literature review. Medicine (Baltimore). 2022;101(35): e30283.
Shen M, et al. Mucor indicus caused disseminated infection diagnosed by metagenomic next-generation sequencing in an acute myeloid leukemia patient: A case report. Front Cell Infect Microbiol. 2023;13:1089196.
Liu K, et al. Diffuse large B-Cell lymphoma of the mandible diagnosed by metagenomic sequencing: a case report. Front Med. 2021;8: 752523.
Acknowledgements
We thank Yajun Liu of Rhode Island Hospital for reviewing and correcting the English grammar of this article.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
CW conceived of the presented idea. LS conducted the literature review and wrote the manuscript with support from TL, YH and YC. SW verified and supervised the findings of this work. All authors read and approved the final version of the manuscript, and ensured it is the case.
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Ethical Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
All authors consent to publish the manuscript in intensive Care Research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shi, L., Lei, T., Huo, Y. et al. A Review of the Application of mNGS in Hematologic Malignancy. Intensive Care Res 4, 9–18 (2024). https://doi.org/10.1007/s44231-023-00053-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44231-023-00053-4