Abstract
Background
The Procalcitonin (PCT) and C-reactive protein (CRP)/albumin ratio have recently been used to predict early prognosis for intensive care unit (ICU) patients and patients undergoing major surgery. But there were few clinical studies in patients after lung transplantation (LTX).
Aim/Purpose
The purpose of this study was to identify the association between PCT combined with CRP/albumin ratio and 30-day mortality and predict the accuracy of PCT combined with CRP/albumin ratio for 30-day mortality in patients after LTX.
Method
From January 1, 2016 to December 1, 2020, the clinical data of 77 patients undergoing LTX who died within 30 days were retrospectively collected, we randomly collected 87 patients survived more than 30 days after LTX. ROC curve was used to evaluate the prognostic value of PCT combined with CRP/albumin in predicting mortality at 30 days after ICU admission, Cox proportional hazard model analysis was used to identify risk factors, subgroup analyses was conducted.
Results
Postoperative PCT, CRP, albumin, CRP/albumin ratio, atrial fibrillation, primary graft dysfunction (PGD) grade, the hours of postoperative mechanical ventilation (MV) and length of ICU stay between survivor and non-survivor had a significant difference. On Cox proportional hazard regression analysis, both PCT [HR 1.02 (1.00–1.05), P = 0.037] and CRP/albumin ratio [HR 1.438 (1.26–1.65), P < 0.001] were independent predictors of 30-day mortality. In all patients after LTX, the area under the curve (AUC) of PCT combined with CRP/albumin ratio for predicting 30-day mortality was 0.76 (95% CI 0.69–0.83). In subgroup analysis, the AUC of PCT combined with CRP/albumin ratio for predicting 30-day mortality was 0.83 (95% CI 0.75–0.91) in patients undergoing LTX for interstitial pulmonary fibrosis (IPF).
Conclusion
The PCT combined with CRP/albumin ratio could be a predictor of the outcomes in patients undergoing LTX. The predictive efficacy was better in patients undergoing LTX for IPF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Lung transplantation (LTX) is now an alternative treatment for many end-stage lung disease patients [1]. With the development of LTX, early postoperative survival is improving, but there is still some gaps than other solid organ transplant patients [2]. There is a need to predict the prognosis of patients after LTX to determine the direction of treatment. Many biomarkers are used for the prediction of prognosis in patients after LTX [3]. A simple and accessible parameter is needed to confirm treatment response and predict mortality in patients after LTX. Procalcitonin (PCT) is primarily used as aids in diagnosis bacterial infections and to guide antimicrobial therapy [4]. Furthermore, several studies have evaluated PCT as a marker for predicting graft outcome and survival, showing that high PCT levels predict poor outcomes in heart, liver, renal and lung transplant recipients without clinical signs of infection [5,6,7]. High C-reactive protein (CRP) levels have been shown to be associated with various conditions, including severe sepsis, heart failure, cerebral disease, and other inflammatory diseases [8]. Furthermore, CRP has been used as a prognostic marker in the critical care setting [9]. Albumin levels can provide nutritional status. Malnutrition is usually correlated with immune dysfunction, inflammatory procedures, and wound healing delay or failure that directly increases the incidence of postoperative complications [10]. The CRP/albumin ratio, a combination of markers for systemic inflammation and nutritional status, has been extensively studied as an independent prognostic marker in patients with infection, malignancy, and other diseases [11]. However, there are relatively few studies in patients after LTX. Patients after LTX have severe lung disease and generally poor nutritional status before surgery [12] and experience Ischemia–reperfusion injury and surgical trauma during surgery, primary graft dysfunction (PGD) occurs within 72 h after transplant. The highest grade of PGD, grade 3, increased 90-day and 1-year mortality compared to absent or lower grades of PGD [13]. These factors may influence the prognostic effectiveness of PCT and CRP/albumin ratio. This study intends to further investigate the predictive value of postoperative PCT, CRP/albumin ratio and PCT combined with CRP/albumin ratio in the 30-day mortality of patients after LTX.
2 Methods
2.1 Study Population
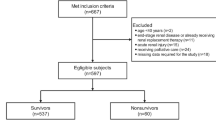
This single-center, retrospective cohort study included 180 successive patients who underwent LTX at Wuxi People’s Hospital between 01-01-2016 and 12-01-2020. The clinical data of 90 patients undergoing LTX who died within 30 days were collected, we randomly collected 90 patients survived within 30 days undergoing LTX. Inclusion criteria: (1) age ≥ 18 years; (2) LTX patients; (3) survival time ≥ 72 h post-transplantation. Exclusion criteria: (1) undergoing secondary LTX; (2) combination with other solid organ transplant patients; (3) incomplete history data.
2.2 Data Extraction
All patients included were classified as survivors or non-survivors based on post-LTX survival status. Groups were compared for the following baseline characteristics: age, sex, primary disease, smoking history, hypertension, diabetes, coronary heart disease, pulmonary hypertension; hemoglobin, platelets, alanine aminotransferase (ALT), aspartate aminotransferase (AST) and serum creatinine within 48 h before surgery; application of intraoperative extracorporeal membrane oxygenation (ECMO), type of transplant operation, operation time; PCT, lactic acid (Lac), CRP and albumin 24 h postoperatively. We compared the complications during postoperative intensive care unit (ICU) hospitalization in the surviving and non-surviving groups, atrial fibrillation and PGD grade at 72 h after surgery, atrial fibrillation was defined by electrocardiogram (ECG), The PGD grade was determined using the International Society for Heart and Lung Transplantation consensus definition [14]. The primary outcome were as follows: survival at 30 days after lung transplantation. The secondary outcome included the hours of postoperative mechanical ventilation (MV) and length of ICU stay.
2.3 The Procedure for Collecting Data and How It Was Protected
During normal clinical care, all parameters were regularly gathered into a database. Checking was done manually. Data was collected on a safe hospital computer and was deidentified and stored.
2.4 Statistical Analysis
Categorical variables were presented as absolute frequency and percentage, and continuous variables were presented as mean ± standard deviation. The clinical characteristics of the two groups, survivors and non-survivors, were compared using the Pearson’s chi-squared test or Fisher’s exact test for categorical variables, and the Student’s t-test for continuous variables. The Cox proportional hazard regression analysis was used to evaluate the association between variables and mortality. The effect of PCT, CRP/albumin ratio, atrial fibrillation, and PGD was evaluated using Cox proportional hazard models, with an adjusted P-value < 0.05 considered statistically significant. Hazard ratios (HRs) and 95% CIs were calculated. Analysis of the receiver operating characteristic (ROC) curves and the area under the ROC curves (AUC) were performed to evaluate PCT, CRP/albumin and PCT combined with CRP/albumin ratio as predictive values for mortality in patients after LTX. In addition, we compared the ROC curves between all patients after LTX and patients undergoing LTX for interstitial pulmonary fibrosis (IPF). A P-values < 0.05 were considered statistically significant. All statistical analyses were performed with IBM SPSS software version 25.0
3 Results
3.1 Patient Characteristics
5 patients underwent second LTX, 2 patients underwent combined cardiopulmonary transplantation, 2 patients survived less than 72 h after surgery, 4 patients had incomplete clinical data. In the survival group, 3 patients were younger than 18 years old. Finally, 164 patients were included in the analysis and data on laboratory result were accurately recorded for all admitted patients. All enrolled 164 patients were divided into two groups: survivors and non-survivors. Table 1 compares the basic features and postoperative condition. There were no significant differences in age, sex, primary disease, smoking, hypertension, diabetes, coronary heart disease, pulmonary hypertension, Hb, platelets, ALT, AST, serum creatinine, intraoperative ECMO application, transplant type, operation time and Lac (P > 0.05), and there were significant differences in PCT, CRP, albumin, CRP/albumin ratio, atrial fibrillation, PGD grade, the hours of postoperative MV and length of ICU stay.
3.2 The Prognosis Factors and Mortality
Univariate and multivariate Cox regression analysis affecting survival after LTX (Table 2). Univariate Cox analysis showed that PCT, CRP/albumin ratio, atrial fibrillation, and PGD had statistically significant effects on survival time. Multivariate Cox analysis showed that PCT [HR = 1.023 (95% CI 1.001–1.046; P = 0.037)], CRP/albumin ratio [HR = 1.438(95% CI 1.257–1.645; P < 0.001)], atrial fibrillation [HR = 2.417 (95% CI 1.360–4.296; P = 0.003)], and PGD [HR = 2.034 (95% CI 1.464–2.828; P < 0.001)] had a statistically significant effect on survival time.
3.3 ROC Curve Analysis
In predicting 30-day mortality, ROC curve comparisons showed that the AUROC of PCT + CRP/albumin ratio (0.758) was the highest among predictors (Table 3, Fig. 1), followed by CRP/albumin ratio (0.743) and PCT (0.622), Moreover, the PCT + CRP/albumin ratio was with the highest sensitivity (84.4%) and negative predictive value (NPV) (80.3%), which highlighted the prediction performance of PCT + CRP/albumin ratio.
3.4 Subgroup Analysis
Patients who underwent LTX for IPF were divided into two groups: survivors and non-survivors. Table 4 compares the basic features and postoperative condition. There were no significant differences in age, sex, primary disease, smoking, hypertension, diabetes, coronary heart disease, pulmonary hypertension, Hb, platelets, ALT, AST, serum creatinine, intraoperative ECMO application, transplant type, operation time, Lac and atrial fibrillation (P > 0.05). And there were significant differences in PCT, CRP, albumin, CRP/albumin ratio, PGD grade, the hours of postoperative MV and length of ICU stay.
3.5 ROC Curve Analysis of Patients Who Underwent LTX for IPF
In predicting 30-day mortality, ROC curve comparisons showed that the AUROC of PCT + CRP/albumin ratio (0.830) was the highest among predictors (Table 5, Fig. 2), followed by CRP/albumin ratio (0.762) and PCT (0.753), Moreover, the PCT + CRP/albumin ratio was with the highest specificity (91.8%) and positive predictive value (PPV) (88.9%), which highlighted the prediction performance of PCT + CRP/ALB.
4 Discussion
An easily available parameter is needed to predict the early survival of patients after LTX to better identify high-risk patients to increase the attention and initial management of these patients, ultimately clinicians achieve the goal of further reducing the early mortality of high-risk patients after LTX. In this study, PCT, CRP/albumin and PCT combined with CRP/albumin were selected to predict the 30-day survival of patients after LTX, and the results showed that both PCT and CRP/albumin were independent risk factors for death at 30 days after LTX.
PCT is mainly produced in the liver by macrophages and neuroendocrine cells [15]. Studies have shown plasma PCT levels rise after liver transplantation, peaking on day 1 and gradually decreasing over the next 7 days [16]. We also found that a significant increase in PCT after LTX, with PCT of 1.97 ng/ml in the survival group and 3.5 ng/ml in the non-survival group (P = 0.007). Mechanism for increasing the level of the PCT after LTX is related to graft hypoxia and use of intraoperative ECMO. Possible explanations include (1) Ischemia–reperfusion injury increases inflammatory factors (e.g., IL-6, IL-8, and IL-10). (2) On the one hand, the use of ECMO causes the destruction of cells and leads to the release of cytokines, on the other hand, it may cause a decrease in renal blood flow, leading to a decrease in renal clearance of PCT. Other study found that PCT = 2 ng/ml within 24 h was used as a cut-off value, The AUC for predicting mortality was 0.74 (95% CI 0.61–0.88). Moreover, the occurrence of grade 3 PGD at 72 h could be excluded at PCT < 2 ng/ml, and the PCT rate for predicting ICU mortality at 24 h was better than that at 48 h and 72 h [17]. In our study, the cut-off value of PCT = 2.81 at 24 h predicted survival at 30 days after LTX, The AUC for predicting 30-day mortality was 0.62 (95% CI 0.54–0.71). The immunosuppressants used in this research center have no effect on the catabolism of PCT, All patients initially received a triple-drug regimen including cal-cineurin inhibitors (cyclosporine or tacrolimus), antimetabo-lites (mycophenolate mofetil or mycophenolate sodium), and corticosteroids.
CRP is an acute-phase protein synthesized by the liver, and its levels reflect the degree of inflammation [18]. On the one hand, LTX surgery causes tissue damage [19]. On the other hand, LTX leads to the occurrence of lung ischemia–reperfusion injury. The acute non-infectious inflammatory reaction caused by LTX leads to lung dysfunction, high expression of a variety of cytokines, release of inflammatory mediators, damage to vascular endothelial and alveolar epithelial cells, aggravate inflammation and induce inflammatory waterfall effect [20]. Therefore, as an inflammatory indicator, CRP has a certain correlation with the occurrence of PGD, which makes it possible to predict the early survival of LTX [21]. Albumin acts as the body’s major serum-binding protein and has a multitude of important physiological functions including maintenance of colloidal osmotic pressure and the binding of a wide variety of compounds [22]. Studies have shown that LTX recipients have a high incidence of nutritional risk and malnutrition, which seriously affects their early prognosis [23]. Hypoalbuminaemia is an independent risk factor for death after LTX [24]. CRP/albumin ratio may reflect both inflammation and nutrition status, and has been used to predict 30-day mortality in critically ill patients, severity of multiple organ dysfunction, and 90-day mortality in patients with sepsis [25,26,27]. Studies have shown that CRP/albumin ratio values at 24 h and 48 h postoperatively are predictive of postoperative complications [9]. Its diagnostic accuracy is higher than that of CRP and albumin alone [28]. Patients with a CRP/albumin ratio of > 2.0 on the third day after abdominal surgery have a higher incidence of postoperative complications [29]. In this review, the use of a CRP/albumin ratio = 1.68 as a cut-off at 24 h predicted survival at 30 days after LTX. The AUC for predicting 30-day mortality was 0.74 (95% CI 0.67–0.82). The predictive power of the CRP/albumin ratio was significantly higher than that of PCT and slightly lower than that of PCT combined CRP/albumin ratio [AUG = 0.76 (95% CI 0.69–0.83)].
Repeated abnormal repair after alveolar epithelial injury occurs in patients with IPF during the development of the disease, resulting in the production of a large number of fibrotic factors [30]. Cell analysis often shows an increase in neutrophils or eosinophils, and other factors lead to the release of pro-inflammatory cytokines [31]. It was speculated that the prognosis of this group of patients was more strongly correlated with the level of inflammation, and IPF accounted for the largest proportion of the primary disease. In subgroup analysis. The predictive power of PCT was significantly improved, and it was concluded that the cut-off value of PCT = 3.55 at 24 h predicted survival at 30 days after LTX, The AUC for predicting 30-day mortality was 0.75 (95% CI 0.66–0.85). There was no significant change in the predictive power of CRP/albumin ratio. The predictive performance of PCT combined with CRP/albumin ratio was significantly improved. The AUC for predicting 30-day mortality was 0.83 (95% CI 0.75–0.91), and significantly higher than PCT and CRP/albumin ratio alone. In patients undergoing LTX for IPF, PCT + CRP/albumin ratio was more effective in predicting 30-day mortality after surgery.
The results of our study had the potential to improve clinical practice. PCT and CRP/albumin ratio were an independent risk factor affecting survival. When patients with IPF after LTx had PCT > 3.55 ng/ml and CRP/albumin > 1.68, suggesting a poor prognosis, the clinician needed to find the cause of the elevated indicator and take treatment measures to intervene. However, further research was needed to confirm whether this intervention is effective.
Our study had several limitations. First, this study is a single-center study, the adaptability in other centers is unknown. Second, PCT and CRP/albumin levels may also be influenced by other factors that are not discussed in this study. Third, the changes in PCT and CRP/albumin ratios over time were not continuously monitored. Fourth, the postoperative albumin level may not really reflect a patient's nutritional status to some extent, It may be affected by supplementation during surgery and treatment. But we want to communicate to anesthesiologists, intensive care physicians, and surgeons a way to explore early outcomes in patients after LTx using traditional prognostic indicators, and hope that future multicenter and prospective experiments will confirm these findings.
5 Conclusion
In summary, our findings further suggest that PCT, CRP/albumin ratio, atrial fibrillation, and PGD were an independent risk factor for death after LTX, postoperative PCT + CRP/albumin ratio had predictive value on the 30-day survival of patients after LTX, in patients undergoing LTX for IPF, PCT + CRP/albumin ratio was more effective in predicting 30-day mortality after surgery.
Availability of Supporting Data
The datasetsused and/or analyzed in the present study are available from the corresponding author on reasonable request.
References
Hartert M, Senbaklavacin O, Gohrbandt B, et al. Lung transplantation: a treatment option in end-stage lung disease. Dtsch Arztebl Int. 2014;111(7):107–16.
Nosotti M, Ferrari M. Nutritional status and lung transplantation: an intriguing problem. Ann Transl Med. 2020;8(3):44.
Bugge TB, Perch M, Rezahosseini O, et al. Post-transplantation anemia and risk of death following lung transplantation. Transplant Proc. 2022;54(8):2329–36.
Sammons C, Doligalski CT. Utility of procalcitonin as a biomarker for rejection and differentiation of infectious complications in lung transplant recipients. Ann Pharmacother. 2014;48(1):116–22.
Svaldi M, Hirber J, Lanthaler AI, et al. Procalcitonin-reduced sensitivity and specificity in heavily leucopenic and immunosuppressed patients. Br J Haematol. 2001;115(1):53–7.
Riera J, Senna A, Cubero M, et al. Primary graft dysfunction and mortality following lung transplantation: a role for proadrenomedullin plasma levels. Am J Transplant. 2016;16(2):634–9.
Dizdar OS, Ersoy A, Akalin H. Pneumonia after kidney transplant: incidence, risk factors, and mortality. Exp Clin Transplant. 2014;12(3):205–11.
Lelubre C, Anselin S, Zouaoui BK, et al. Interpretation of C-reactive protein concentrations in critically ill patients. Biomed Res Int. 2013;2013: 124021.
Donlon NE, Mohan H, Free R, et al. Predictive value of CRP/albumin ratio in major abdominal surgery. Ir J Med Sci. 2020;189(4):1465–70.
Ding Q, Chen W, Chen C, et al. Evaluation of nutritional status in lung transplant recipients and its correlation with post-transplant short-term prognosis: a retrospective study. Ann Transl Med. 2022;10(14):793.
Kalyon S, Gültop F, Şimsek F, et al. Relationships of the neutrophil-lymphocyte and CRP-albumin ratios with the duration of hospitalization and fatality in geriatric patients with COVID-19. J Int Med Res. 2021;49(9):3000605211046112.
Kim CY, Kim SY, Song JH, et al. Usefulness of the preoperative prognostic nutritional index score as a predictor of the outcomes of lung transplantation: a single-institution experience. Clin Nutr. 2019;38(5):2423–9.
Clausen E, Cantu E. Primary graft dysfunction: what we know. J Thorac Dis. 2021;13(11):6618–27.
Snell GI, Yusen RD, Weill D, et al. Report of the ISHLT working group on primary lung graft dysfunction, part I: definition and grading-A 2016 consensus group statement of the international society for heart and lung transplantation. J Heart Lung Transplant. 2017;36(10):1097–103.
Kan WC, Huang YT, Wu VC, et al. Predictive ability of procalcitonin for acute kidney injury: a narrative review focusing on the interference of infection. Int J Mol Sci. 2021;22(13):6903.
Desmard M, Benbara A, Boudinet S, et al. Post-operative kinetics of procalcitonin after lung transplantation. J Heart Lung Transplant. 2015;34(2):189–94.
Mazo C, Borgatta B, Pont T, et al. Procalcitonin accurately predicts lung transplant adults with low risk of pulmonary graft dysfunction and intensive care mortality. J Crit Care. 2018;44:142–7.
Thijs LG, Hack CE. Time course of cytokine levels in sepsis. Intensive Care Med. 1995;21(Suppl 2):S258-263.
Ticinesi A, Lauretani F, Nouvenne A, et al. C-reactive protein (CRP) measurement in geriatric patients hospitalized for acute infection. Eur J Intern Med. 2017;37:7–12.
Kao CC, Parulekar AD. Postoperative management of lung transplant recipients. J Thorac Dis. 2019;11(Suppl 14):S1782-s1788.
Harano T, Ryan JP, Morrell MR, et al. Extracorporeal membrane oxygenation for primary graft dysfunction after lung transplantation. ASAIO J. 2021;67(9):1071–8.
Labgaa I, Joliat GR, Kefleyesus A, et al. Is postoperative decrease of serum albumin an early predictor of complications after major abdominal surgery? A prospective cohort study in a European centre. BMJ Open. 2017;7(4): e013966.
Barnes L, Reed RM, Parekh KR, et al. Mechanical ventilation for the lung transplant recipient. Curr Pulmonol Rep. 2015;4(2):88–96.
Baldwin MR, Arcasoy SM, Shah A, et al. Hypoalbuminemia and early mortality after lung transplantation: a cohort study. Am J Transplant. 2012;12(5):1256–67.
Mao M, Wei X, Sheng H, et al. C-reactive protein/albumin and neutrophil/lymphocyte ratios and their combination predict overall survival in patients with gastric cancer. Oncol Lett. 2017;14(6):7417–24.
Wei XL, Wang FH, Zhang DS, et al. A novel inflammation-based prognostic score in esophageal squamous cell carcinoma: the C-reactive protein/albumin ratio. BMC Cancer. 2015;15:350.
Kinoshita A, Onoda H, Imai N, et al. The C-reactive protein/albumin ratio, a novel inflammation-based prognostic score, predicts outcomes in patients with hepatocellular carcinoma. Ann Surg Oncol. 2015;22(3):803–10.
Park JE, Chung KS, Song JH, et al. The c-reactive protein/albumin ratio as a predictor of mortality in critically ill patients. J Clin Med. 2018;7(10):333.
Basile-Filho A, Lago AF, Menegueti MG, et al. The use of APACHE II, SOFA, SAPS 3, C-reactive protein/albumin ratio, and lactate to predict mortality of surgical critically ill patients: a retrospective cohort study. Medicine (Baltimore). 2019;98(26): e16204.
Kapnadak SG, Raghu G. Lung transplantation for interstitial lung disease. Eur Respir Rev. 2021;30(161):210017.
George PM, Patterson CM, Reed AK, et al. Lung transplantation for idiopathic pulmonary fibrosis. Lancet Respir Med. 2019;7(3):271–82.
Acknowledgements
We are grateful to acknowledge Yachen Shi for his valuable suggestions and discussions.
Funding
No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
HX, JC, and CX participated in the design of the study. CX wrote the application for the ethical approval. DW, SW, JZ, JL, XL, and ML collected the data. CX analyzed the data. CX drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
Institutional Review Board provided ethical permission for the research (No. KY23003). The study is in compliance with the Helsinki Congress and the Declaration of Istanbul.
Consent to participate
As a consequence of the retrospective design and anonymization of patient identifiers, it did not involve informed consent.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xuan, C., Wang, D., Wang, S. et al. The Procalcitonin Combined with C-Reactive Protein/Albumin Ratio as a Predictor of Mortality in Patients After Lung Transplantation. Intensive Care Res 3, 221–228 (2023). https://doi.org/10.1007/s44231-023-00043-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44231-023-00043-6