Abstract
Background
The use of veno-arterial extracorporeal membrane oxygenation (V-A ECMO) for cardiorespiratory support is increasing. However, few criteria for hemodynamic management have been described yet in V-A ECMO patients.
Method
We performed a review of hemodynamic management during V-A ECMO in CS patient based the literature published. We discuss how to optimize hemodynamic management.
Results
Patients on V-A ECMO require special hemodynamic management. It is crucial to maintain an adequate tissue oxygen supply and demand balance. Hemodynamic optimization is essential to support LV decompression and improve end-organ function and should be initiated immediately after initiating V-A ECMO support, during which more positive fluid balance is associated with worse outcomes.
Conclusion
The hemodynamic management of CS patients with V-A ECMO are complex and involves various aspect. Clinicians who care for patients on VA ECMO should combined use many availability indicators to guide hemodynamic management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Cardiogenic shock (CS) is a physiologic state of low cardiac output (CO) leading to end-organ hypoperfusion despite adequate fluid resuscitation. Venoarterial extracorporeal membrane oxygenation (VA-ECMO) provides both respiratory and cardiac support and adequate blood flow to vital organs in shock patients. Accepted indication for VA-ECMO includes patients with cardiogenic shock caused by acute myocardial infarction, myocarditis, end-stage dilated cardiomyopathy, postcardiotomy, or posttransplantation [1,2,3,4]. According to different situations, V-A ECMO provides support of cardiopulmonary to CS patients as a bridge for myocardial recovery, durable mechanical circulation support or heart transplant [5, 6]. When circulation dependent on ECMO completely, blood flow is directly dependent on the vascular factors that determine venous return, e.g. vascular closing conditions, pressure vascular volume and the elastance and resistive properties of vessels [7].In addition, CS and post-resuscitation syndrome patients may experience systemic capillary leakage due to damage to endothelial cells, often presenting as sepsis-like syndrome, therefore may develop systemic capillary leakage, which can induce intravascular hypovolemia [8,9,10].V-A ECMO itself is also a cause of inflammation, which can lead to severe vascular paralysis due to extensive blood exposure to non-endothelial substances [11, 12].To date, there are few reviews of hemodynamic management during V-A ECMO in CS patient. Hemodynamic management in patient with CS during V-A ECMO is summarized in this review.
2 Pathophysiology and Hemodynamics of CS
The pathophysiology of CS is poorly understood due to a paucity of high-quality clinical data. In general, CS leads to a spiral decrease in stroke volume (SV), an increase in ventricular diastolic pressure and wall stress, which reduces coronary perfusion. In addition, left ventricular (LV) dysfunction and ischemia increase diastolic stiffness and left atrial pressure (LAP), worsen pulmonary congestion, hypoxia, and ischemia [13]. Initial compensatory mechanisms led to activation of the sympathetic nervous system and the renin–angiotensin–aldosterone system, which leads to salt and water retention, increasing the burden of preload and decompensatory heart failure. Local and systemic catecholamine release transiently increases myocardial chronotropy and inotropy at the cost of arrhythmias and increased peripheral vasoconstriction rates, increased afterload, and mismatched myocardial perfusion. Hemodynamic changes include macrohemodynamics and microhemodynamics, the latter reflecting the patient's perfusion and metabolic status [14]. Blood pressure (BP), systemic vascular resistance (SVR), central venous pressure (CVP), CO, and pulmonary capillary wedge pressure (PCWP) are the key parameters of macro hemodynamics. Central venous saturation and arterial lactate are the important parameters of micro hemodynamics [14, 15]. Hyperlactatemia is a non-specific global indicator of tissue hypoxia, and serum lactate is an indirect method for clinical evaluation of microcirculation in patients with CS. The change of manifested as an elevated serum lactate level is indicator of the micro hemodynamics change in CS patients [16].Recovery of hemodynamic parameters, reflecting normalization of the macro circulation, does not always result in recovery of the microcirculation [17].Microcirculatory changes are particularly evident in the lungs, kidneys, liver, gastrointestinal tract, brain and heart, creating a vicious cycle of persistent cascade [18,19,20,21].Although the exact pathophysiology of this multifactorial, hemodynamically diverse population remains poorly understood, early identification and intervention to interrupt the devastating ‘CS spiral’ is critical to survival [22](Fig. 1).
The downward spiral of refractory cardiogenic shock. The downward spiral of cardiogenic shock results from severe cardiac dysfunction leading to ongoing systemic and coronary hypoperfusion. A commonly observed systemic inflammatory response might lead to vasodilatation and further contribute to ongoing cardiac dysfunction and end-organ insult. Cardiogenic shock will inevitably lead to death if the cycle of damage is not interrupted. NOS nitric oxide synthase, NO nitric oxide.
3 Configurations of V-A ECMO and Harlequin Syndrome
V-A ECMO drains blood from the venous access and returns oxygenated blood directly into the arterial circulation. Within V-A ECMO, there are a few different configurations with the two principle strategies being peripheral and central V-A ECMO used in the setting of CS. Peripheral V-A ECMO consists of the femoral drainage cannula and returns oxygenated blood through the common femoral artery [23]. The peripheral configuration provides retrograde flow up the descending aorta that mixes with anterograde blood flow from the left ventricle [24, 25]. The competition of the retrograde and anterograde flow can lead to LV overload and Harlequin syndrome (North–South syndrome). North–South syndrome is a complication unique to peripheral V-A ECMO [26]. It may develop under circumstances when native cardiac function recovers pulsatility, yet pulmonary function remains inadequate. The location of the mixing cloud depends on the native cardiac function and the level of competing ECMO flow. All organs perfused by the anterograde flow are at risk for ischemia, including the brain and the myocardium. Therefore, arterial oxygen saturation and arterial blood gases should always be monitored using samples obtained from the right radial artery as the innominate artery is the first branch to receive deoxygenated blood from the proximal aortic arch. The main advantage of peripheral cannulation is its ability to be finished at the bedside, even during active chest compressions. Central V-A ECMO need surgical placement of both venous and arterial cannulas [23, 27]. The venous cannula is traditionally placed in the right atrium, with the arterial return cannula placed in the ascending aorta. The central V-A ECMO minimizes the risk of North–South syndrome and allows for better cardiac decompression [23]. With the inflow cannula returning blood to the ascending aorta, there is less competition of retrograde and anterograde blood flow than in peripheral V-A ECMO, minimizing the risk of upper body hypoxemia [24]. Surgical placement of inflow and outflow cannulas limits the ability of central V-A ECMO to be implemented in emergent setting and is often best utilized in patients with postcardiotomy CS [28]. Risks of bleeding and resultant surgical reexploration and mediastinitis are all increased risks for patients undergoing central V-A ECMO [23, 29].
4 The Pathophysiology and Hemodynamic of V-A ECMO
By drawing blood directly from the systemic venous system, V-A ECMO reduced the RV preload. Due to the opposite flow in the aorta, peripheral V-A ECMO increased LV afterload [30, 31].In the presence of hypotension and CS, the increase in mean artery pressure (MAP)after initiation of V-A ECMO was associated with a significant increase in PCWP and a decrease in LV SV, which counteracted the ventricular emptying and its work [32]. When V-A ECMO is established for CS due to right ventricle failure, PCWP is usually low and the LV is relatively insensitive to afterload. Thus, the shift in the Starling curve with increasing systemic pressure is slight, and a modest increase in PCWP would be accompanied by an increase in LV afterload, assuming no significant change in LV SV [32].When V-A ECMO is used for CS due to acute LV failure, the shift in the starling curve is substantial due to the LV afterload sensitivity and influenced by the magnitude of systemic pressure changes. In this situation, if PCWP is already high and LV contractility does not improve significantly, PCWP is expected to increase dramatically with LV dilation(LVD) [32].
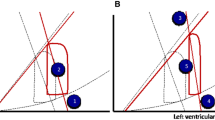
The overall effect of reduced volume work and increased pressure work depends on the “dose” of V-A ECMO, as well as on myocardial function and its response to these phenomena. In the presence of fixed and significantly decreased LV contractility, the effect of ECMO flow on right-and left-sided parameters is as follows: for each increment of ECMO flow from baseline conditions (from 1 to 4.75 L/min), right atrial pressure decreased and aortic pressure increased; however, at the same time, LV volumes increased, LV SV decreased, whereas left ventricular end-diastolic pressure(LVEDP), LV end-systolic pressure, left atrium (LA) and pulmonary artery pressure (PAP)rise [26]; therefore, ECMO can induce or exacerbate preexisting pulmonary edema. At the same time, as the flow rate increased, the arterial pressure increased and the pulse pressure decreased, indicating a gradual decrease in the LV SV and decreased gradually and a shortened aortic valve opening duration. On the pressure–volume diagram, these are shown as rightward/upwards shifts of the pressure–volume loop along the end-diastolic pressure–volume relationship and a narrowing of the loop. At the highest ECMO flow rate (4.75 L/min), the aortic valve barely opens, which may lead to blood stasis in the LV ventricle. Stasis of blood in the LV maylead to thrombosis of the LV, aortic and lung, which can lead to stroke, peripheral embolism, pulmonary embolism, and, in many cases, is fatal [33].
In combination with an increased afterload and LV diastolic pressure, LV dilation decreases the gradient of trans coronary perfusion and may impair coronary perfusion, leading to or worsening myocardial ischemia [34].Overall, inadequate LV unloading is considered the main cause of poor LV recovery and failure to wean from V-A ECMO in at least one series [35]. In conclusion, LV distention, pulmonary edema, and blood stasis in the LV and aortic root are highly relevant events. Finally, one of the physiological factors is ECMO-associated inflammatory response, similar to the systemic inflammatory response syndrome. The inflammatory response occurs immediately when blood is exposed to the non-endothelailized surface of ECMO circuit, leading to activation of the innate immune system [36].
5 Hemodynamic Monitoring of V-A ECMO
Patients on V-A ECMO require special volume management. Insufficient volume status may lead to a dangerous inhalation of V-A ECMO cannulas on the wall of vessel, resulting in reduced V-A ECMO output. Volume optimization is essential to support LV decompression and improve end-organ function and should be initiated immediately after initiating V-A ECMO support, during which more positive fluid balance is associated with worse outcomes [37]. Optimal fluid status can be achieved with renal replacement therapy (RRT) [38]. Because modern centrifugal pumps are preload-dependent and afterload-sensible, preload monitoring should be checked several times a day. The purpose of the hemodynamic monitoring in V-A ECMO patients is to provide information about the adequacy of organs and peripheral perfusion [39]. Patients with severe cardiac dysfunction receiving V-A ECMO support are at high risk of developing low CO syndrome due to the presence of underlying CS or V-A ECMO. Adequate hemodynamic monitoring should provide information about either the underlying cardiac disease evaluating the patient’s cardiac performance or the effectiveness of the ECMO support [40]. For patients with V-A ECMO, both non-invasive (focused echocardiography) and invasive (pulmonary artery catheter (PAC)) hemodynamic monitoring should be performed [41].
6 Cardiac Output
CO measurement by thermodilution method and measurement of mixed venous oxygen saturation (ScvO2) are often overestimated because venous blood reaching the right atrium is primarily withdrawn by the therein located venous cannula. In addition, CO measurements based on pulse-profile analysis should not be used in the absence of pulsation. In the absence of natural CO, non-pulsatile arterial pressure profile, loss of aortic valve opening and closing properties, and loss of cardiac contraction were detected. For these reasons, echocardiography has become increasingly important in hemodynamic monitoring [42]. As standard hemodynamic monitoring in patients with V-A ECMO, The pump function of LV and RV and the size of all four heart chambers were assessed daily [43].If myocardial contraction increases during V-A ECMO through better pump function and more regular aortic valve opening, then V-A ECMO flow rate decreases slowly with hemodynamics and clinical status. Transesophageal echocardiography findings such as an improvement of ejection fraction (EF), an LV outflow tract velocity–time integral greater than 10 cm, absence of LV dilation, and increased aortic valve opening could indicate recovery of LV function [44].
7 Arterial Pressure
While maintaining blood flow is critical to the care of patients on V-A ECMO, attention should also be paid to MAP, as end organs require both CO and perfusion pressure for optimal function and low venous pressure. A target MAP > 65 mmHg can be used as a starting point, but can be adjusted higher or lower depending on individual circumstances, keeping in mind that MAP and LAP differences are drivers of organ perfusion and function. A recent paper showed an inverse relationship between mortality and MAP in V-A ECMO [45]. Many different policies exist to manage arterial pressure during V-A ECMO: one issue of concern is the equivalence of MAP for patients with or without pulsation. Physiologic autoregulation is key to end-organ perfusion, especially in the brain and kidney. Many studies addressed ideal MAP value for patients in Intensive care unit (ICU), the most definitive of which is a threshold of 65 mmHg, which is usually sufficient if the study shows that a MAP values of 75-85 mmHg is protective against acute kidney injury (AKI) in patients with a history of hypertension [46]. However, to our knowledge, only a handful of studies have examined optimal MAP in ECMO patients, and the evidence supporting each practice remains weak. The heart is in a dynamic parallel circulation with ECMO to achieve equilibrium and drain the blood flow from the ECMO circuit. The amount of workload may often be incompatible with cardiac failure in most V-A ECMO patients. If a lower MAP justifies allowing the heart to resist lower resistance and reduced the myocardial oxygen demand, the clinical impact of hypotension on CS patients must be carefully judged. Furthermore, it may not be appropriate to compare MAP in patients with and without pulsatile,as non-pulsatile patients may require higher MAP for end-organ perfusion. Although usually interpreted as are covery LV function, the presence of pulsation in the arterial waveform, signifying an increase in LV contractility, may reflect either improved LV contractility or worsening volume overload; these two mechanisms can be distinguished by follow-up PCWP or repeat echocardiographic assessment [32].
8 Tissue Perfusion and Microcirculation
In critically ill patients on V-A ECMO, it is crucial to maintain an adequate tissue oxygen supply and demand balance. The extracorporeal mechanical device should provide optimal tissue perfusion in the management of different pathophysiological variables encountered during ECMO support [47].
Measurement of venous oxygen saturation (SvO2) in the pulmonary artery using the Swan-Ganz catheter has been widely recognized as a good indicator of the global tissue perfusion provided by the patient’s cardiac function and the extracorporeal support [48]. During ECMO, the continuous variation of the hemodynamic parameters, the hemoglobin content or the arterial blood oxygenation makes the trend of the SvO2 values a better indicator of the match between the oxygen delivery (DO2) and the oxygen consumption (VO2) than an absolute value of ScvO2 [49]. While measurement of the SvO2 during ECMO usually accurately reflects the efficacy of tissue perfusion, sometimes SvO2 values could not adequately represent overall perfusion. Although the SvO2 expresses a match between DO2 and VO2, calculating SVO2values in the pulmonary artery trunk does not reflect the ultimate regional distribution of blood flow and the different perfusion in different body regions. It should be considered that low coronary and/or cerebral flow may occur during V-A ECMO due to a certain degree of deoxygenation and oxygenation of the blood mixture at the descending thoracic aorta.
Although hyperlactatemia is nonspecific marker of global tissue hypoxia, in clinical practice, evaluating serum lactate is an indirectly method to assess microcirculation for CS patients with V-A ECMO. The early lactate measurements (particularly lactate clearance), as an index of macrocirculation and microcirculation, after ECMO support have a high correlation with in-hospital mortality [50].The absolute level of lactate with ECMO support is more important for prognosis than a pre-ECMO level or the magnitude of decline from pre-ECMO to on-ECMO [51].
Capillary refill time (CRT) refers to the time it takes the nail bed of a distal phalange to return to its normal color after pressure has been applied with the extremity at heart level [52,53,54]. CRT is a tool to evaluate tissue perfusion which is easily available, easy to perform, and has no additional cost for patients with CS. CRT was first introduced by Beecher et al. in 1947 as a way of evaluating circulatory status and perfusion in critically injured soldiers, in order to evaluate and predict the severity of their injuries [55]. Importantly, CRT was not correlated with macrohemodynamics such as cardiac index or systemic blood pressure. Merdji and colleagues [56]present findings from a two-center observational cohort study of 59 patients with cardiogenic shock evaluating the association between peripheral tissue perfusion and clinical outcomes. Poor peripheral perfusion, such as prolonged (> 3 s) CRT, were associated with the composite of 90-day all-cause mortality or receipt of V-A ECMO support, which occurred in 42% of participants.
In addition to perfusion “pressure” (MAP), perfusion “flow” plays a key role in adequate organ perfusion and microcirculation. Perfusion flow or pump minute volume is determined by the following formula: flow = body surface (m2) × cardiac index (CI) (L/min/m2). Therefore, perfuse flow is dependent on body surface and CI of approximately 3–5 l/min. Control of perfusion flow should be performed in conjunction with volume management and catecholamine therapy as necessary.MAP is regulated by perfusion flow and total peripheral vascular resistance. Reducing pump minute volume according to peripheral vascular resistance leads to a decrease of MAP and vice versa. If pump minute volume is inadequate, bedside echocardiography is required to assess the hemodynamic status [57].
9 Identify Patients at Risk of Developing LV Distention and Pulmonary Edema
As mentioned above, dilatation of the left ventricle and pulmonary veins can rapidly lead to massive acute pulmonary edema and left heart blood stasis, with a serious risk of thrombus formation. Identifying LV dilatation and pulmonary edema during V-A ECMO support is very important for patient management. There are several clinical indicators that can be used to monitor and identify patients at risk [58]. In the simplest terms, the presence and extent of aortic valve opening can be detected in arterial pulse pressure tracings. As ECMO flow increases, MAP increases, while pulse pressure and SV decrease, reflecting a decrease in the degree of aortic valve opening. Second, echocardiography can directly show the extent and duration of aortic valve opening. In principle, echocardiography can also be used to assess changes in LV dimension; however, echocardiography may be particularly insensitive in the assessment of LV dilation because the nonlinearity of the LV end-diastolic pressure–volume relationship and pericardial constraints may limit changes in LV dimensions despite significant changes in LV end-diastolic pressure. In addition, LV size measured during ECMO support may be misinterpreted as an indicator of ventricular dilation, LV end-diastolic pressure, and PCWP due to different premorbid conditions. Third, a progressive hypoxia in blood exiting the LV, which can be measured from the right radial artery or by cerebral oximetry, may signal the perfusion of deoxygenated blood into the superior circulation due to worsening pulmonary edema. Fourth, chest x-rays showing worsening pulmonary edema may worsening PCWP. However, this may be a late finding and non-specific, as radiographic findings may also be caused by other diseases, such as acute respiratory distress syndrome or infection. Fifth, assessment the maintained Starling relationship may help predict ventricular distension during ECMO support. Since LV afterload before ECMO is related to systemic arterial pressure, and the Starling curve generated before ECMO initiation can predict the filling pressure of any target SV under systemic pressure. Increasing ECMO flow or alterations in SVR solely, does not change the relationship between filling pressure and native LV SV [32]. Sixth, pre-initiation EF can be used to predict the risk of ventricular distention after initiation of V-A ECMO, because the risk of ventricular distension after initiation of V-A ECMO is associated with the pre-initiation EF in a setting of high afterload sensitivity due to decreased contractility. Even a slight decrease in pre-ECMO EF values (less than 50%) may predict high PCWP after V-A ECMO regime because of a sudden increase in systemic pressure and afterload upon completion of peripheral cannulation [32]. Each of these 6 measures are straight forward for detecting or predicting aortic valve opening and LV loading but provide only indirect indicators for monitoring increases in PCWP for that PCWP is determined by LVEDP, pulmonary artery diastolic pressure is assumed to be close to the LAP (as a PCWP surrogate), which is an important parameter for monitoring LV filling pressure in the absence of pulmonary catheter wedges) [26]. The most direct and timely way to detect LV loading and pulmonary congestion progression is with the use of PAC. Many experts argue that all patients on V-A ECMO should be managed with PAC, as many high-volume centers do [59].
10 LV Unloading and V-A ECMO
It is increasingly recognized that V-A ECMO, particularly peripheral V-A ECMO, can significantly increase LV afterload by retrograde arterialized blood infusion into the descending aorta [60]. This may lead to an increase in LVEDP, leading to an increase in LVD, which may be associated with impaired myocardial recovery or other signs of LV pressure overload, such as loss of arterial pulsatility, ventricular arrhythmia, pulmonary edema or intracardiac thrombosis [61, 62]. The main risk factors for LV distention in patients on V-A ECMO include: (1) Severe LV failure [28, 61]. Through increasing LV afterload, which can cause systolic closure of the aortic valve, V-A ECMO exacerbates LV failure; (2) Aortic insufficiency [63].Any degree of aortic sufficiency can exacerbate LV overload. Although mitral regurgitation alleviates LV pressure overload, it exacerbates pulmonary edema [61, 64, 65]; (3) High ECMO flow. Increased afterload caused byV-A ECMO is related to pump flow [63]; (4)Intravascular volume overload caused by excessive fluid infusion, which may lead to elevated LV filling pressures [28]. Besides simply reducing V-A ECMO flow, there are at least 7 methods of LV unloading during V-A ECMO have been used, including positive inotropic drugs, pharmacologic afterload reduction, intra-aortic balloon pump(IABP), atrial septostomy, left atrial venting, surgical LV venting, and various Impellas. Most patients with V-A ECMO receive pharmacologic therapy as standard of care, but these methods tend to increase myocardial workload and VO2 and should be used with caution. For nearly two decades, IABP has been used as an adjunct to V-A ECMO to generate pulsatile blood flow and reduce afterload, with more than 2500 patients reported in the literature [66].When aiming to reduce a PCWP by 20 mmHg or less, consider initiating IABP. Impella is a percutaneously deployed, micro-axial flow pump that pumps blood from LV to aortic root, thereby reducing LV afterload and consistently decreasing LV end-diastolic and pulmonary venous pressures [67,68,69]. When more unloading is required, Impella should be added to V-A ECMO, as increasingly reported recently [70, 71].Of all other options, Impella appears to offer the largest and most direct form of LV decompression, while providing additional active blood flow to systemic circulation at the same time [72].Indications for LV venting are generally considered to include:(1) closure of aortic valve due to high risk of ventricular stasis and thrombosis [28]; (2)severe aortic regurgitation that exacerbates LV overload and distention on V-A ECMO [28]; (3) severe refractory pulmonary edema secondary to LV overload [28];and (4) patients who are not candidates for early left ventricular assist device (LVAD) support. Rupprecht et al. [28]suggested that V-A ECMO with LV venting be recommended for patients with high recovery potential, whereas early LVAD implantation should be considered for patients with low recovery potential. Notably, in many centers, LV unloading is used early in the stage of ECMO therapy, not only to avoid elevated PCWP, but also to actively unloading the LV, often deploying the unloading device and ECMO sequentially during the same procedure. Although the study did not demonstrate any benefit of prophylactic left heart decompression (LHD) on myocardial recovery, it identified an association between prophylactic LHD and higher rate of successful bridging to heart transplantation or LVAD and improved survival [73]. Concurrent percutaneous transseptal LA drainage at the onset of ECMO was associated with lower early mortality and increased likelihood of successful bridging to cardiac replacement therapy. Prevention or early LHD can improve clinical outcomes in patients at high risk of LVD. However, the study had several inherent biases in the retrospective observational study design. Prospective randomized controlled studies are needed to provide reasonable recommendations for prophylactic LHD [73].LA venting catheter insertion is a commonly performed procedure for LHD in patients with V-A ECMO. However, the LA venting procedure may cause process-related complications, especially when a large catheter is inserted, whereas a small catheter can lead to inadequate LHD. Therefore, the catheter size for the procedure should be selected carefully [74]. In this study, we report the efficacy of LHD with an 8-Fr Mullins sheath in patients who received V-A ECMO and developed LVD. Pulmonary edema was significantly improved in the majority of patients, and all patients were successfully weaned from ECMO. This implies that even a small amount of LA drainage, closely monitored for catheter fluency and effectiveness, may be effective in relieving distended LV and improving patient prognosis. LHD with a small catheter may be an option without mechanical complications, especially for patients who expect LV function [74].
LV volume distention is an important problem in patients on V-A ECMO, with sequelae including myocardial ischemia, severe pulmonary edema, and intracardiac thrombosis. There is limited data on many important issues, including their incidence, diagnostic criteria and timing for intervention. Given the diversity of surgical and transdermal treatment options available, more research is needed in all these areas, as well as in best practices for LHD. Predicting which patients will benefit from adjuvant interventions remains a clinical challenge because of their inherent procedural risks and predicting the expected degree of LV discharge can be cumbersome extremely when intervening in an individual patient.
11 Conclusion
The use of VA ECMO for cardiopulmonary support has escalated substantially over the past several years. The hemodynamic monitoring and volume management of CS patients with V-A ECMO are complex and involves various aspect. Clinicians who care for patients on VA ECMO should combined use many availability indicators for evaluating the volume status to guide volume management. Finally, there are still relatively few studies on this aspect, and large-scale clinical studies are needed to guide clinical practice.
Data availability
Not applicable.
Abbreviations
- CS:
-
Cardiogenic shock
- V-A ECMO:
-
Veno-arterial extracorporeal membrane oxygenation
- SV:
-
Stroke volume
- LAP:
-
Left atrial pressure
- LV:
-
Left ventricular
- SVR:
-
Systemic vascular resistance
- BP:
-
Blood pressure
- CVP:
-
Central venous pressure
- CO:
-
Cardiac output
- PAWP:
-
Pulmonary capillary wedge pressure;
- CRT:
-
Capillary refill time
- MAP:
-
Mean artery pressure
- LVEDP:
-
Left ventricular end-diastolic pressure
- LA:
-
Left atrium
- PAP:
-
Pulmonary artery pressures
- RRT:
-
Renal replacement therapy
- PAC:
-
Pulmonary artery catheter
- ICU:
-
Intensive care unit
- AKI:
-
Acute kidney injury
- ScvO2 :
-
Mixed venous oxygen saturation
- SvO2 :
-
Venous oxygen saturation
- DO2 :
-
Oxygen delivery
- VO2 :
-
Oxygen consumption
- SVR:
-
Systemic Vascular Resistance
- EF:
-
Ejection fraction
- LAP:
-
Left atrial pressure
- IABP:
-
Intra-aortic balloon pump
- SAPS-II:
-
Simplified acute physiology score II
- SAVE:
-
The survival after veno-arterial-ECMO
- LVAD:
-
Left ventricular assist device
- LHD:
-
Left heart decompression
References
Guglin M, Zucker MJ, Bazan VM, et al. Venoarterial ECMO for adults: JACC scientific expert panel. J Am Coll Cardiol. 2019;73(6):698–716.
Pineton de Chambrun M, Brechot N, Combes A. Mechanical circulatory devices in acute heart failure. Curr Opin Crit Care. 2018; 24(4): 286–91.
Dangers L, Brechot N, Schmidt M, et al. Extracorporeal membrane oxygenation for acute decompensated heart failure. Crit Care Med. 2017;45(8):1359–66.
Mebazaa A, Combes A, van Diepen S, et al. Management of cardiogenic shock complicating myocardial infarction. Intensive Care Med. 2018;44(6):760–73.
Venkataraman S, Bhardwaj A, Belford PM, Morris BN, Zhao DX, Vallabhajosyula S. Veno-Arterial Extracorporeal Membrane Oxygenation in Patients with Fulminant Myocarditis: A Review of Contemporary Literature. Medicina (Kaunas) 2022; 58(2).
Telukuntla KS, Estep JD. Acute Mechanical Circulatory Support for Cardiogenic Shock. Methodist Debakey Cardiovasc J. 2020;16(1):27–35.
Moller PW, Hana A, Heinisch PP, et al. The effects of vasoconstriction and volume expansion on veno-arterial ECMO flow. Shock. 2019;51(5):650–8.
Frydland M, Ostrowski SR, Moller JE, et al. Plasma concentration of biomarkers reflecting endothelial cell- and glycocalyx damage are increased in patients with suspected ST-elevation myocardial infarction complicated by cardiogenic shock. Shock. 2018;50(5):538–44.
Heradstveit BE, Guttormsen AB, Langorgen J, et al. Capillary leakage in post-cardiac arrest survivors during therapeutic hypothermia - a prospective, randomised study. Scand J Trauma Resusc Emerg Med. 2010;18:29.
Adrie C, Adib-Conquy M, Laurent I, et al. Successful cardiopulmonary resuscitation after cardiac arrest as a “sepsis-like” syndrome. Circulation. 2002;106(5):562–8.
Al-Fares A, Pettenuzzo T, Del Sorbo L. Extracorporeal life support and systemic inflammation. Intensive Care Med Exp. 2019;7(Suppl 1):46.
Burgdorff AM, Bucher M, Schumann J. Vasoplegia in patients with sepsis and septic shock: pathways and mechanisms. J Int Med Res. 2018;46(4):1303–10.
Hajjar LA, Teboul JL. Mechanical circulatory support devices for cardiogenic shock: state of the art. Crit Care. 2019;23(1):76.
Joris PJ, Plat J, Bakker SJ, Mensink RP. Effects of long-term magnesium supplementation on endothelial function and cardiometabolic risk markers: a randomized controlled trial in overweight/obese adults. Sci Rep. 2017;7(1):106.
Baker WL. Treating arrhythmias with adjunctive magnesium: identifying future research directions. Eur Heart J Cardiovasc Pharmacother. 2017;3(2):108–17.
Jung C, Fuernau G, de Waha S, et al. Intraaortic balloon counterpulsation and microcirculation in cardiogenic shock complicating myocardial infarction: an IABP-SHOCK II substudy. Clin Res Cardiol. 2015;104(8):679–87.
Ince C. Hemodynamic coherence and the rationale for monitoring the microcirculation. Crit Care. 2015;19(Suppl 3):S8.
Jung C, Kelm M. Evaluation of the microcirculation in critically ill patients. Clin Hemorheol Microcirc. 2015;61(2):213–24.
Jung C, Jung F, Kelm M. The microcirculation in hypoxia: the center of the battlefield for oxygen. Clin Hemorheol Microcirc. 2016;63(3):169–72.
De Backer D, Creteur J, Dubois MJ, Sakr Y, Vincent JL. Microvascular alterations in patients with acute severe heart failure and cardiogenic shock. Am Heart J. 2004;147(1):91–9.
De Backer D, Ospina-Tascon G, Salgado D, Favory R, Creteur J, Vincent JL. Monitoring the microcirculation in the critically ill patient: current methods and future approaches. Intensive Care Med. 2010;36(11):1813–25.
van Diepen S, Katz JN, Albert NM, et al. Contemporary management of cardiogenic shock: a scientific statement from the american heart association. Circulation. 2017;136(16):e232–68.
Jayaraman AL, Cormican D, Shah P, Ramakrishna H. Cannulation strategies in adult veno-arterial and veno-venous extracorporeal membrane oxygenation: techniques, limitations, and special considerations. Ann Card Anaesth. 2017;20(Supplement):S11–8.
Le Gall A, Follin A, Cholley B, Mantz J, Aissaoui N, Pirracchio R. Veno-arterial-ECMO in the intensive care unit: from technical aspects to clinical practice. Anaesth Crit Care Pain Med. 2018;37(3):259–68.
Stulak JM, Dearani JA, Burkhart HM, Barnes RD, Scott PD, Schears GJ. ECMO cannulation controversies and complications. Semin Cardiothorac Vasc Anesth. 2009;13(3):176–82.
Rao P, Khalpey Z, Smith R, Burkhoff D, Kociol RD. Venoarterial extracorporeal membrane oxygenation for cardiogenic shock and cardiac arrest. Circ Heart Fail. 2018;11(9): e004905.
Camboni D, Philip A, Schmid C, Loforte A. Double, triple and quadruple cannulation for veno-arterial extracorporeal membrane oxygenation support: is there a limit? Ann Cardiothorac Surg. 2019;8(1):151–9.
Rupprecht L, Florchinger B, Schopka S, et al. Cardiac decompression on extracorporeal life support: a review and discussion of the literature. ASAIO J. 2013;59(6):547–53.
Mikus E, Tripodi A, Calvi S, Giglio MD, Cavallucci A, Lamarra M. CentriMag venoarterial extracorporeal membrane oxygenation support as treatment for patients with refractory postcardiotomy cardiogenic shock. ASAIO J. 2013;59(1):18–23.
Hekimian G, Jovanovic T, Brechot N, et al. When the heart gets the flu: fulminant influenza B myocarditis: a case-series report and review of the literature. J Crit Care. 2018;47:61–4.
Stevens MC, Callaghan FM, Forrest P, Bannon PG, Grieve SM. Flow mixing during peripheral veno-arterial extra corporeal membrane oxygenation—a simulation study. J Biomech. 2017;55:64–70.
Dickstein ML. The starling relationship and veno-arterial ECMO: ventricular distension explained. ASAIO J. 2018;64(4):497–501.
Weber C, Deppe AC, Sabashnikov A, et al. Left ventricular thrombus formation in patients undergoing femoral veno-arterial extracorporeal membrane oxygenation. Perfusion. 2018;33(4):283–8.
Hlavacek AM, Atz AM, Bradley SM, Bandisode VM. Left atrial decompression by percutaneous cannula placement while on extracorporeal membrane oxygenation. J Thorac Cardiovasc Surg. 2005;130(2):595–6.
Kurihara H, Kitamura M, Shibuya M, Tsuda Y, Endo M, Koyangi H. Effect of transaortic catheter venting on left ventricular function during venoarterial bypass. ASAIO J. 1997;43(5):M838–41.
Millar JE, Fanning JP, McDonald CI, McAuley DF, Fraser JF. The inflammatory response to extracorporeal membrane oxygenation (ECMO): a review of the pathophysiology. Crit Care. 2016;20(1):387.
Staudacher DL, Gold W, Biever PM, Bode C, Wengenmayer T. Early fluid resuscitation and volume therapy in venoarterial extracorporeal membrane oxygenation. J Crit Care. 2017;37:130–5.
Chen H, Yu RG, Yin NN, Zhou JX. Combination of extracorporeal membrane oxygenation and continuous renal replacement therapy in critically ill patients: a systematic review. Crit Care. 2014;18(6):675.
Porhomayon J, El-Solh A, Papadakos P, Nader ND. Cardiac output monitoring devices: an analytic review. Intern Emerg Med. 2012;7(2):163–71.
Guarracino F, Zangrillo A, Ruggeri L, et al. beta-Blockers to optimize peripheral oxygenation during extracorporeal membrane oxygenation: a case series. J Cardiothorac Vasc Anesth. 2012;26(1):58–63.
Beckmann A, Benk C, Beyersdorf F, et al. Position article for the use of extracorporeal life support in adult patients. Eur J Cardiothorac Surg. 2011;40(3):676–80.
Merkle J, Azizov F, Fatullayev J, et al. Monitoring of adult patient on venoarterial extracorporeal membrane oxygenation in intensive care medicine. J Thorac Dis. 2019;11(Suppl 6):S946–56.
Fitzgerald DC, Darling EM, Cardona MF. Staffing, equipment, monitoring considerations for extracorporeal membrane oxygenation. Crit Care Clin. 2017;33(4):863–81.
Hussey PT, von Mering G, Nanda NC, Ahmed MI, Addis DR. Echocardiography for extracorporeal membrane oxygenation. Echocardiography. 2022;39(2):339–70.
Tanaka D, Shimada S, Mullin M, Kreitler K, Cavarocchi N, Hirose H. What Is the optimal blood pressure on veno-arterial extracorporeal membrane oxygenation? Impact of mean arterial pressure on survival. ASAIO J. 2019;65(4):336–41.
Leone M, Asfar P, Radermacher P, Vincent JL, Martin C. Optimizing mean arterial pressure in septic shock: a critical reappraisal of the literature. Crit Care. 2015;19:101.
Chommeloux J, Montero S, Franchineau G, et al. Microcirculation evolution in patients on venoarterial extracorporeal membrane oxygenation for refractory cardiogenic shock. Crit Care Med. 2020;48(1):e9–17.
Grant C Jr, Richards JB, Frakes M, Cohen J, Wilcox SR. ECMO and right ventricular failure: review of the literature. J Intensive Care Med. 2021;36(3):352–60.
Chauhan S, Subin S. Extracorporeal membrane oxygenation, an anesthesiologist's perspective: physiology and principles. Part 1. Ann Card Anaesth 2011; 14(3): 218–29.
Li CL, Wang H, Jia M, Ma N, Meng X, Hou XT. The early dynamic behavior of lactate is linked to mortality in postcardiotomy patients with extracorporeal membrane oxygenation support: a retrospective observational study. J Thorac Cardiovasc Surg. 2015;149(5):1445–50.
Omar HR, Handshoe JW, Tribble T, Guglin M. Survival on venoarterial extracorporeal membrane oxygenation in cardiogenic shock: which lactate is most useful? ASAIO J. 2022;68(1):41–5.
Huber W, Zanner R, Schneider G, Schmid R, Lahmer T. Assessment of regional perfusion and organ function: less and non-invasive techniques. Front Med (Lausanne). 2019;6:50.
Kleinman ME, Chameides L, Schexnayder SM, et al. Pediatric advanced life support: 2010 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Pediatrics. 2010;126(5):e1361–99.
Pickard A, Karlen W, Ansermino JM. Capillary refill time: is it still a useful clinical sign? Anesth Analg. 2011;113(1):120–3.
Beecher HK, Simeone FA, et al. The internal state of the severely wounded man on entry to the most forward hospital. Surgery. 1947;22(4):672–711.
Merdji H, Curtiaud A, Aheto A, et al. Performance of early capillary refill time measurement on outcomes in cardiogenic shock: an observational, prospective multicentric study. Am J Respir Crit Care Med. 2022;206(10):1230–8.
Price S, Platz E, Cullen L, et al. Expert consensus document: Echocardiography and lung ultrasonography for the assessment and management of acute heart failure. Nat Rev Cardiol. 2017;14(7):427–40.
Ong CS, Hibino N. Left heart decompression in patients supported with extracorporeal membrane oxygenation for cardiac disease. Postepy Kardiol Interwencyjnej. 2017;13(1):1–2.
Rihal CS, Naidu SS, Givertz MM, et al. 2015 SCAI/ACC/HFSA/STS clinical expert consensus statement on the use of percutaneous mechanical circulatory support devices in cardiovascular care: Endorsed by the American Heart Assocation, the Cardiological Society of India, and Sociedad Latino Americana de Cardiologia Intervencion; Affirmation of Value by the Canadian Association of Interventional Cardiology-Association Canadienne de Cardiologie d’intervention. J Am Coll Cardiol. 2015;65(19):e7–26.
Broome M, Donker DW. Individualized real-time clinical decision support to monitor cardiac loading during venoarterial ECMO. J Transl Med. 2016;14:4.
Truby LK, Takeda K, Mauro C, et al. Incidence and implications of left ventricular distention during venoarterial extracorporeal membrane oxygenation support. ASAIO J. 2017;63(3):257–65.
Brechot N, Demondion P, Santi F, et al. Intra-aortic balloon pump protects against hydrostatic pulmonary oedema during peripheral venoarterial-extracorporeal membrane oxygenation. Eur Heart J Acute Cardiovasc Care. 2018;7(1):62–9.
Sidebotham D, Allen S, McGeorge A, Beca J. Catastrophic left heart distension following initiation of venoarterial extracorporeal membrane oxygenation in a patient with mild aortic regurgitation. Anaesth Intensive Care. 2012;40(3):568–9.
Meani P, Gelsomino S, Natour E, et al. Modalities and effects of left ventricle unloading on extracorporeal life support: a review of the current literature. Eur J Heart Fail. 2017;19(Suppl 2):84–91.
Lim HS. The effect of impella cp on cardiopulmonary physiology during venoarterial extracorporeal membrane oxygenation support. Artif Organs. 2017;41(12):1109–12.
Donker DW, Brodie D, Henriques JPS, Broome M. Left ventricular unloading during veno-arterial ECMO: a review of percutaneous and surgical unloading interventions. Perfusion. 2019;34(2):98–105.
Watanabe S, Fish K, Kovacic JC, et al. Left Ventricular Unloading Using an Impella CP Improves Coronary Flow and Infarct Zone Perfusion in Ischemic Heart Failure. J Am Heart Assoc 2018; 7(6).
Amin AP, Spertus JA, Curtis JP, et al. The evolving landscape of impella use in the united states among patients undergoing percutaneous coronary intervention with mechanical circulatory support. Circulation. 2020;141(4):273–84.
Lim HS. The physiologic basis and clinical outcomes of combined impella and veno-arterial extracorporeal membrane oxygenation support in cardiogenic shock. Cardiol Ther. 2020;9(2):245–55.
Pappalardo F, Schulte C, Pieri M, et al. Concomitant implantation of Impella((R)) on top of veno-arterial extracorporeal membrane oxygenation may improve survival of patients with cardiogenic shock. Eur J Heart Fail. 2017;19(3):404–12.
Eliet J, Gaudard P, Zeroual N, et al. Effect of impella during veno-arterial extracorporeal membrane oxygenation on pulmonary artery flow as assessed by end-tidal carbon dioxide. ASAIO J. 2018;64(4):502–7.
Schrage B, Burkhoff D, Rubsamen N, et al. Unloading of the left ventricle during venoarterial extracorporeal membrane oxygenation therapy in cardiogenic shock. JACC Heart Fail. 2018;6(12):1035–43.
Na SJ, Yang JH, Yang JH, et al. Left heart decompression at venoarterial extracorporeal membrane oxygenation initiation in cardiogenic shock: prophylactic versus therapeutic strategy. J Thorac Dis. 2019;11(9):3746–56.
Kim S, Kim JS, Shin JS, Shin HJ. How small is enough for the left heart decompression cannula during extracorporeal membrane oxygenation? Acute Crit Care. 2019;34(4):263–8.
Acknowledgements
None.
Funding
This study was supported by Tianjin Science and Technology Plan Project (18ZXDBSY00100, 21JCYBJC01200); Rui E (Rui Yi) Emergency Medicine Research Special Fund (R2019006); Tianjin Key Medical Discipline (Specialty) Construction Project (TJYXZDXK-035A).
Author information
Authors and Affiliations
Contributions
CY prepared the figures and contributed to the writing of the manuscript. LX designed and contributed to the writing of the manuscript. Both authors agree to be accountable for the content of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yin, C., Xu, L. Hemodynamic Management During Veno-Arterial Extracorporeal Membrane Oxygenation in Patients with Cardiogenic Shock: A Review. Intensive Care Res 3, 131–139 (2023). https://doi.org/10.1007/s44231-023-00039-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44231-023-00039-2