Abstract
Introduction
Sepsis associated acute kidney injury (SAKI) is a common complication of sepsis with high incidence and mortality around the world. SAKI characterized by low survival rate, poorlong-term prognosis and quality of life of patients, causes huge economic burden to family and society. A large amount of evidence indicates that early diagnosis and necessary treatment of SAKI can effectively improves the prognosis of patients. However, at present, laboratory indicators for early diagnosis of SAKI are limited. Therefore, understanding the risk factors associated with SAKI is crucial for early prediction of SAKI.
Method
The meta-analysis was conducted with PRISMA statement. All studies are collected from PubMed, Web of Science, Cochrane library, Wiley online library and CNKI databases, and all published from the initiation of the database to Feb 11, 2022, were included.
Result
A total of 25 studies were included in this meta-analysis, with statistically significant risk factors as follows: diabetes [1.79 (1.43 2.24)], hypotension (MAP < 65 mmHg) [2.25 (1.88 2.70)], coagulation dysfunction [1.14 (1.04 1.24)], liver disease [1.68 (1.28 2.20)], heart disease [1.89 (1.54 3.31)], high APACHEII scores [1.25 (1.02 1.53)], lactic acidosis [1.65 (1.38 1.97)], oliguria [ 1.45 (1.01 2.08), high serum creatinine (> 88 mol/l) [3.84 (2.10 7.04)].
Conclusion
Diabetes, hypotension (MAP < 65 mmHg), coagulation dysfunction, liver disease, heart disease, high APACHEII score, lactic acidosis, oliguria, high serum creatinine are the risk factors of SAKI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Sepsis is a common life-threatening clinical syndrome in the intensive care units, affecting 20–30 million people worldwide each year. Severe sepsis can directly lead to multi-organ dysfunction and is the leading cause of death in ICU patients. Acute kidney injury (AKI) is a common and serious complication of sepsis. The incidence rate of Sepsis associated acute kidney injury (SAKI) is up to 47.5% [1].
SAKI is an acute organ dysfunction syndrome and is a common complication in critically ill patients. There are approximately 6 million cases worldwide each year [2]. SAKI is associated with long hospital stays, high mortality rates and high medical costs in ICU patients. It has imposed a huge economic burden on society. The pathogenesis of SAKI includes hemodynamic disorder, endothelial cell damaged by cytokines and oxygen free radicals, abnormal coagulation and energy metabolism. However, the pathogenesis of SAKI has not been fully elucidated [3]. Treatment for SAKI includes early fluid resuscitation, antibiotics and renal replacement. The pathogenesis of SAKI is complexity and early treatment is important, which indicates that early diagnosis of SAKI by clinicians is essential. Up to now, doctors generally judge whether patients have AKI by indicators such as serum creatinine and urine volume. However, serum creatinine and urine volume have some limitations in the diagnosis of AKI—elevated serum creatinine concentration is an insensitive indicator of kidney injury and is limited by the lack of baseline values in many patients [4]. Oliguria may be nonspecific in SAKI. This meta-analysis aims to analyze the risk factors for the occurrence of SAKI, so as to help the early prediction of SAKI.
2 Methods
2.1 Inclusion Criteria
Patients that met the following criteria were included: A. Meeting the diagnostic criteria for sepsis or septic shock (sepsis 1.0, sepsis 2.0, sepsis 3.0). B. Meeting the diagnostic criteria for AKI (KDIGO, AKIN, RIFLE). C. Original data provides OR value and 95%CI or data can be converted to OR value and 95% CI.
2.2 Exclusion Criteria
A. Pre-existing renal insufficiency or other renal disease. B. AKI not due to sepsis (eg. renal transplantation, use of nephrotoxic drugs or contrast agents, urinary obstruction). C. No risk factors in the outcome index. D. NOS quality score < 6. E. Repeated and reviewed literature.
2.3 Data Extraction
Taking Pubmed as an example, the search strategy is: ((Sepsis [MeSH]) OR (sepsis[Title/Abstract]) OR (infective shock [Title/Abstract]) OR (bloodstream infection[Title/Abstract]) OR (septic shock [Title/Abstract]) OR (pyemia [Title/Abstract]) OR (pyohemia [Title/Abstract]) OR (severe sepsis [Title/Abstract])) AND ((acute kidney injury [MeSH]) OR (acute kidney injury [Title/Abstract]) OR (acute renal injury [Title/Abstract]) OR (acute kidney failure [Title/Abstract]) OR (acute renal failure[Title/Abstract]) OR (acute renal insufficiencies[Title/Abstract])) AND ((risk factor) OR (factor) OR (influence factor) OR (relevant factor) OR (hazard)).
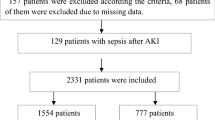
Firstly, the titles and abstracts of all retrieved articles were read to exclude irrelevant articles. Secondly, Read the full text, articles that did not meet the criteria were excluded according to the inclusion and exclusion criteria (Fig. 1). Finally, data were extracted from the included studies, including author's name, country or region, year of publication, research design, sample size, data of SAKI patients and other information (Table 1). Extract study results including relevant risk factors, OR values, 95% CI and P values.
2.4 Quality Analysis
All included studies were examined by the NOS quality assessment scale, which is available at http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. NOS score ≥ 6 was considered high-quality articles and were included in the study, and exclude the low-quality articles.
2.5 Statistical Analysis
After extracting data of the 25 included studies, the OR values and 95% CI of risk factors were imported into Stata SE 16.0 software. Heterogeneity test was performed on the study data first. If I2 ≥ 50%, inter-group data were considered to be heterogeneous, the combined amount was calculated using random effect model. If I2 < 50%, the fixed-effect model is adopted (Table 2). Pooled OR and 95%CI were finally obtained. P ≤ 0.05 were considered to be statistically significant. The relevant data of each risk factor obtained were summarized and drawn the forest map (Fig. 2).
3 Result
3.1 Literature Search Process and Results
By 2022.02 we retrieved 3,323 studies from Pubmed, Web of Science, Cochrane library, Wiley online library and CNKI databases. After reading the titles and abstracts, excluding irrelevant and duplicate studies, we included 51 studies. We finally included 25 studies in 8 countries by reading the full text.
3.2 Basic Information of the Included Literature and Quality Evaluation Results
There were 8 case–control studies, 12 retrospective cohort studies, 4 prospective cohort studies, and 1 RCT study among the 23 included papers. The quality of all included study articles was good according to the NOS quality evaluation scale.
3.3 Results of Meta-Analysis of Risk Factors in the Literature Related to SAKI
Meta-analysis of 13 related risk factors for SAKI (including general factors, comorbidities, and laboratory examination results) revealed statistically significant risk factors (P < 0.05) are as follow: diabetes, hypotension(MAP < 65 mmHg), coagulation dysfunction, liver disease, heart disease, high APACHEII score, lactic acidosis, oliguria, high serum creatinine (> 88 mol/l) (Table 3).
3.4 Sensitivity Analysis
Sensitivity analyses were performed by changing the analysis model and re-combining the statistics after excluding each study in turn, and none of the results changed from one side to the other, suggesting more stable results. Sensitivity analysis of the study results was performed by changing the analysis model and excluding literature with large sources of heterogeneity or weights to observe the stability of the study results.
3.5 Publish Bias Analysis
Funnel plots were drawn for risk factors (diabetes mellitus, lactic acidosis) with ≥ 7 studies, we found the funnel plots are asymmetrical. The result suggests that publication bias exists in the theses two risk factors (Fig. 3, 4).
4 Discussion
SAKI, a kind of renal hypoperfusion and inflammatory factor response storm caused by sepsis or septic shock, further causes necrosis of renal tubular epithelial cells, resulting in acute renal function damage. The long hospital stay, high mortality rate and high medical expenses of this disease have imposed a huge economic burden on society and families, arousing extensive concern from medical researchers. The pathogenesis of SAKI is so complex that it has not been elucidated. At present, the treatment effect of SAKI is still not ideal, and the mortality rate is high. The main treatment methods include early fluid resuscitation, anti-infection and renal replacement for hypoperfusion of tissues and organs. The earlier the treatment of SAKI is carried out, the higher the survival rate of patients. At present, the diagnosis of SAKI is mainly based on creatinine and urine volume per hour. In the Paper, the purpose of meta-analysis was to analyze the risk factors leading to SAKI and provide help for early identification and prompt treatment of SAKI. We found that the main risk factors for SAKI include diabetes, hypotension (MAP < 65 mmHg), and high serum creatinine (> 88 mol/l). Secondary risk factors include coagulation disorder, liver disease, heart disease, high APACHEII score, lactic acidosis, and oliguria. Our results are generally consistent with other studies, but there are some differences. Such as hypertension, mechanical ventilation, WBC and PCT.
A lot of studies shown that hypotension, high APACHEII score and oliguria are the risk factor of SAKI. (a) Hypotension is a risk factor for SAKI. Because of when patients are in shock, continuous hypotension will lead to severe renal blood insufficiency, which will directly result in renal tubular necrosis, thus causing renal function damage [30]. (b) The assessment items for APACHEII score include age, severe organ dysfunction and immune impairment, GCS score and physiology-related indicators, through which the general situation of patients can better be reflected and the expected mortality of patients can also be evaluated. The higher APACHEII score of patients with sepsis, the worse the basic vital signs and general conditions of patients, and the poorer the body’s self-regulation ability and immune response to infection. According to the research by Cheng Xiaoying et al. [31]. APACHEII score ≥ 19 is an independent risk factor for AKI in patients with sepsis. (c) Oliguria and anuria are also risk factors for the occurrence of SAKI. Systemic hemodynamic instability and reduced renal blood perfusion of patients with sepsis and septic shock lead to renal tissue ischemia and hypoxia and renal tubular damage, resulting in serious reduction of glomerular filtration rate. The decrease of urine volume per hour is a sensitive indicator of renal function damage, which can better predict the occurrence of SAKI.
-
a.
Diabetes is a risk factor for SAKI, with unclear mechanism. The possible reasons are that the infection degree of patients with sepsis complicated with diabetes is more serious, and inflammatory factor storm induces the occurrence of AKI. In addition, after severe infection, the incidence of stress hyperglycemia in patients with diabetes increases, and hyperosmolar state induced by high glucose also affects renal function [32].
-
b.
Coagulation dysfunction is a risk factor for SAKI. The consumption of coagulation factors and platelets reduces the synthesis of coagulation factors, which promotes the hyperfibrinolysis and leads to the significant extension of PT, APTT and TT and the significant reduction of FIB level, thus resulting indiffuse intravascular coagulation that impairsrenal function. Coagulation dysfunction not only promotes the occurrence of SAKI [33], but also increases the mortality rate of patients with SAKI. Other comorbid factors include heart disease (coronary heart disease and heart failure) and liver disease.
In this study, it is showed that the risk factors of laboratory test for SAKI are lactic acidosis and serum creatinine level. Serum lactic acid level, an important indicator of microcirculation perfusion, can better evaluate the hypoxia state of tissues and organs when it is increased. The increase of creatinine level is a risk factor for SAKI. Creatinine, a macromolecule solute in the body, is a metabolite of creatine, which mainly discharged through glomerular filtration. AKI can be diagnosed when the serum creatinine level of patients with sepsis increases by more than 1.5 times the baseline level, which is of certain value for the early prediction of the occurrence of SAKI [34]. According to the research by Hoste et al. [10], the risk for the development of AKI was increased 7.5 times when serum creatinine level was greater than 1.0 mg/dL (88 mol/L). However, in the process of clinical diagnosis and treatment, the baseline creatinine level of patients is often difficult to be obtained, and the baseline creatinine level at admission does not represent the actual baseline creatinine value. Therefore, the prediction of baseline value of serum creatinine and the degree of elevation in SAKI remains to be studied.
In this study, it is showed that hypertension, invasive mechanical ventilation, WBC and PCT have no statistical significance (P > 0.05). WBC, a traditional infection indicator, is still widely used in the early diagnosis of patients with sepsis, especially bacterial infection. However, there are many factors affecting WBC, and the degree of its elevation may not accurately reflect the severity of sepsis.PCT, an important inflammatory indicator, has higher specificity than other indicators in the early diagnosis of bacterial systemic infection, so it can more accurately assess the severity of the disease. WBC and PCT reflect the severity of sepsis to a certain extent rather than the renal function damage, without predictive value for SAKI. The application of invasive mechanical ventilation should not be used as an indicator reflecting renal function damage. However, the study of Shen Hejin et al. [35] showed that after 24 h of invasive mechanical ventilation, the glomerular filtration rate, urea and creatinine clearance rates of patients decreased significantly. The reason may be that improper use of ventilator, thus resulting in reduced renal blood perfusion and renal failure. At the same time, for patients who use invasive mechanical ventilation for a long time, if the degree of analgesia and sedation is insufficient, the activation of RAAS system can be stimulated by sympathetic nerve excitation and the renal blood flow can be reduced, thus resulting in renal function damage. In the process of clinical treatment, improper use of ventilator rarely occurs. If ventilator parameters are out of the normal range, they will be promptly adjusted.
Although in this study, studies from multiple countries or regions were included, there is no detailed grouping for the distinction between different countries or regions, which may be due to the lack of relevant studies and data on the risk factors for AKI in patients with sepsis in the same country and region. In addition, the research included in this meta-analysis was not completely consistent with the inclusion criteria of the cases, which leads to the heterogeneity of the final results. We have attempted to reduce clinical and methodological heterogeneity by eliminating the weighty literature and conducting a more detailed subgroup analysis of the study, but the analysis effect was not significant and the forest map showed that heterogeneity remained high. In this study, highly heterogeneous data was analyzed by a randomized control model. However, the methods reduce the heterogeneity between studies remain to be studied. In this meta-analysis, publication bias analysis was performed on risk factors (diabetes mellitus, lactic acidosis) that included ≥ 7 articles. The reason of publication bias is that researchers are more likely to publish positive results because negative results have little significance for the study on risk factors. Another possible reason is that some negative studies are not included in databases or journals.
5 Conclusion
The results of this study suggest that the main risk factors for SAKI include diabetes, hypotension (MAP < 65 mmHg), and high serum creatinine (> 88 mol/l). Secondary risk factors include coagulation disorder, liver disease, heart disease, high APACHEII score, lactic acidosis, and oliguria.
Availability of Data and Material
The datasets analysed during the current study available from the corresponding author on reasonable request.
References
Xiaoli H. Progress of epidemiology and outcome for sepsis. Chin Crit Care Med. 2018;30(05):486–9.
Peerapornratana S, Manrique-Caballero CL, Gómez H, Kellum JA. Acute kidney injury from sepsis: current concepts, epidemiology, pathophysiology, prevention and treatment. Kidney Int. 2019;96(5):1083–99.
Zhixiong Z. Advances in the pathogenesis of acute kidney injury induced by sepsis. Chin J Lab Diagn. 2019;23(10):1853–7.
Chenhui L. Progress in the diagnosis and treatment of septic associate acute kidney injury. J Intern Intensiv Med. 2021;27(05):422–7.
Wang X, Jiang L, Wen Y, et al. Risk factors for mortality in patients with septic acute kidney injury in intensive care units in Beijing, China: a multicenter prospective observational study. Biomed Res Int. 2014;2014: 172620.
Liu J, Su Z, Zhang ZC. A multiplicity of morbidity and prognostic factors in patients with septic and acute kidney injury. Zhonghua Yi Xue Za Zhi. 2011;91(16):1112–4.
Fan C, Ding X, Song Y. A new prediction model for acute kidney injury in patients with sepsis. Ann Palliat Med. 2021;10(2):1772–8.
Suh SH, Kim CS, Choi JS, Bae EH, Ma SK, Kim SW. Acute kidney injury in patients with sepsis and septic shock: risk factors and clinical outcomes. Yonsei Med J. 2013;54(4):965–72.
Medeiros P, Nga HS, Menezes P, Bridi R, Balbi A, Ponce D. Acute kidney injury in septic patients admitted to emergency clinical room: risk factors and outcome. Clin Exp Nephrol. 2015;19(5):859–66.
Hoste EA, Lameire NH, Vanholder RC, Benoit DD, Decruyenaere JM, Colardyn FA. Acute renal failure in patients with sepsis in a surgical ICU: predictive factors, incidence, comorbidity, and outcome. J Am Soc Nephrol. 2003;14(4):1022–30.
Cobussen M, de Kort JM, Dennert RM, Lowe SH, Stassen PM. No increased risk of acute kidney injury after a single dose of gentamicin in patients with sepsis. Infect Dis (London, England). 2016;48(4):274–80.
Deng F, Peng M, Li J, Chen Y, Zhang B, Zhao S. Nomogram to predict the risk of septic acute kidney injury in the first 24 h of admission: an analysis of intensive care unit data. Ren Fail. 2020;42(1):428–36.
Gameiro J, Gonçalves M, Pereira M, et al. Obesity, acute kidney injury and mortality in patients with sepsis: a cohort analysis. Ren Fail. 2018;40(1):120–6.
Plataki M, Kashani K, Cabello-Garza J, et al. Predictors of acute kidney injury in septic shock patients: an observational cohort study. Clin J Am Soc Nephrol. 2011;6(7):1744–51.
Hsu YC, Hsu CW. Septic acute kidney injury patients in emergency department: the risk factors and its correlation to serum lactate. Am J Emerg Med. 2019;37(2):204–8.
Kwong YD, Mehta KM, Miaskowski C, et al. Using best subset regression to identify clinical characteristics and biomarkers associated with sepsis-associated acute kidney injury. Am J Physiol Renal Physiol. 2020;319(6):F979-f987.
Song J, Wu W, He Y, Lin S, Zhu D, Zhong M. Value of the combination of renal resistance index and central venous pressure in the early prediction of sepsis-induced acute kidney injury. J Crit Care. 2018;45:204–8.
Yegenaga I, Hoste E, Van Biesen W, et al. Clinical characteristics of patients developing ARF due to sepsis/systemic inflammatory response syndrome: results of a prospective study. Am J Kidney Dis. 2004;43(5):817–24.
Bu X, Zhang L, Chen P, Wu X. Relation of neutrophil-to-lymphocyte ratio to acute kidney injury in patients with sepsis and septic shock: a retrospective study. Int Immunopharmacol. 2019;70:372–7.
Kim JH, Park YS, Yoon CY, et al. Delta neutrophil index for the prediction of the development of sepsis-induced acute kidney injury in the emergency department. Shock (Augusta, Ga). 2019;52(4):414–22.
Bagshaw SM, George C, Bellomo R. Early acute kidney injury and sepsis: a multicentre evaluation. Crit Care. 2008;12(2):R47.
Iglesias J, Marik PE, Levine JS. Elevated serum levels of the type I and type II receptors for tumor necrosis factor-alpha as predictive factors for ARF in patients with septic shock. Am J Kidney Dis. 2003;41(1):62–75.
Chawla LS, Seneff MG, Nelson DR, et al. Elevated plasma concentrations of IL-6 and elevated APACHE II score predict acute kidney injury in patients with severe sepsis. Clin J Am Soc Nephrol. 2007;2(1):22–30.
Yi D. Risk factors and prognosis of acute kidney injury in elderly patients with sepsis in ICU. Chin J Geriatr. 2015;34(06):641–4.
Laping C. Predictive value of complement and coagulation indicators in sepsis related acute kidney injury. Chin J Intern Med. 2020;59(11):854–9.
Aiying Z. Risk factors of acute kidney injury in patients with emergency sepsis. Pract Clin J Integr Tradit Chin West Med. 2019;19(07):115–6+163.
Miaoyi F. Risk factors for acute kidney injury in sepsis patients. Pract J Clin Med. 2017;14(05):52–5.
Zhou J, Bai Y, Wang X, et al. A simple risk score for prediction of sepsis associated-acute kidney injury in critically ill patients. J Nephrol. 2019;32(6):947–56.
Yazici Ozkaya P, Taner S, Ersayoğlu I, et al. Sepsis associated acute kidney injury in pediatric intensive care unit. Ther Apheresis Dial. 2022;27:73–82.
Guoping Z. Risk factors of acute kidney injury induced by hypotension in severe patients. China Health Care Nutrition. 2012;22(08):804–6.
Yingxiao C. The predictive value of APACHE II score combined with urine neutrophil gelatinase-associated apolipoprotein in sepsis complicated with acute kidney injury. Clin Misdiagn Misther. 2020;33(06):57–62.
Wenliang Z. Occurrence and prognosis of septic associated acute kidney injury in elderly diabetic patients in ICU. Med Recapitulate. 2017;23(19):3938–41.
Manqiu M. Correlation analysis of coagulation index and all-cause death in patients with septic associated acute kidney injury. Chin J Nephrol. 2019;10:758–64.
Xuying L. Diagnosis of acute kidney injury: creatinine or urine volume? Chin J Crit Care Intens Care Med (Electron Edn). 2017;3(01):9–13.
Hejin S. Effect of mechanical ventilation on renal function in chronic obstructive pulmonary disease. Chin J Aesthet Med. 2012;21(z1):146–7.
Funding
This work is supported by Natural Science Foundation of Shandong Province (ZR2020MH197) and Science and technology development program of Shandong Province (2019WS021).
Author information
Authors and Affiliations
Contributions
HL planned and designed the research; SH assisted in retrieving the data; XH tested the feasibility of the study; HL wrote the manuscript; all the authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical Approval and Consent of Participate
An ethics statement is not applicable because this study is based exclusively on published literature. Informed consent was obtained from all individual participants included in the study.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, H., Hou, S. & Tian, X. Risk Factors of Sepsis Associated Acute Kidney Injury in Patients with Sepsis: A Meta-Analysis. Intensive Care Res 3, 163–170 (2023). https://doi.org/10.1007/s44231-023-00034-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44231-023-00034-7