Abstract
Purpose
With the improvement of people’s life expectancy, the incidence of stroke is high in the world. Post-stroke Dysphagia seriously affects people’s quality of life, among which malnutrition and pulmonary infection are the most common complications of post-stroke Dysphagia. At this point, it is very important to choose the right enteral and parenteral feeding mode. Current nutrition methods commonly used in patients with dysphagia after stroke include Intermittent oral to esophageal tube feeding (IOE), Nasogastric tube (NG), Nasal Jejunal feeding tubes (NJ), Percutaneous endoscopic gastrostomy (PEG).The purpose of this meta-analysis was to study the prognosis of patients with dysphagia after stroke who chose different nutritional methods.
Methods
We conducted a systematic review and meta-analysis of randomized controlled trials (RCTS) to examine the effects of different nutritional modalities on outcomes in patients with post-stroke dysphagia. We searched the Cochrane Library, PubMed, Medline, China National Knowledge Infrastructure (CNKI), Wanfang, and the VIP database. The search period is from the library's establishment to December 31, 2021.At least 2 reviewers independently assessed eligibility criteria, extracted data, and assessed the risk of bias. Standardized mean difference (SMD), relative risk (RR), and odds ratio (OR) were calculated using a random-effects model.
Results
Fourteen studies were identified across six databases that met the inclusion criteria, The results of meta-analysis showed that Intermittent oral to esophageal tube feeding (IOE) could improve the nutritional levels of patients better than nasogastric tube (NG) (MD 1.95, 95%CI 1.22–2.67, P < 0.00001, I2 = 0%), and reduced the incidence of aspiration pneumonia (RR 0.39, 95%CI 0.23–0.66, P = 0.0004, I2 = 0%), improved swallowing function (OR 3.92, 95%CI 2.15–7.14, P < 0.00001, I2 = 0%). Although Percutaneous endoscopic gastrostomy (PEG) can improve the nutrition of patients in the short term, the long-term prognosis remains to be discussed. In addition, the Nasal Jejunal feeding tubes (NJ) significantly reduced the incidence of post-stroke pneumonia compared with NG (RR 0.51, 95%CI 0.29–0.92, P = 0.03, I2 = 0%).
Conclusions
According to the results of meta-analysis, IOE can better improve the nutritional level of patients and reduce the incidence of complications. However, due to the lack of popularity and small target clients, patients who do not accept IOE enteral feeding for various reasons and choose nasal feeding can consider using NJ as a long-term enteral feeding method, and guard against adverse events when performing supplementary nutrition.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Background
Stroke is common in the world [1], about 2 million people in China suffer from stroke each year, and 70–80% of them are left with significant disabilities that prevent them from living a normal life [2].Acute stroke patients often have severe impairment of consciousness and swallowing. Dysphagia occurs in 51–73% of stroke patients [3, 4].It can directly affect the intake and utilization of nutrients, leading to malnutrition, infection disease, concurrent infection and other aggravating conditions, delaying the recovery of neurological function5.It has been reported that the incidence of nutritional disorders in stroke is about 15%, and the incidence of nutritional disorders rises to 30% one week after stroke, affecting the prognosis of patients [6, 7].One US forecast predicts stroke-related medical costs will exceed $183 billion a year by 2030 [8], malnutrition can further worsen the health status of stroke patients, increase the cost of treatment, and prolong the length of hospital stay [9].The mortality rate of dysphagia patients after cerebral infarction was 29–37%, among which, the mortality rate of cerebral infarction patients caused by pulmonary infection was about 10%, and aspiration pneumonia was the main cause of death, accounting for 1/3 of all pneumonia deaths in the elderly [10].
Deglutition can be divided into 4 stages, respectively for preparation period, oral period, pharyngeal period and esophageal period, any stage of disease can lead to deglutition difficulties. Initiation of swallowing is a voluntary activity and requires the integrity of sensorimotor areas of the cerebral cortex [11].The nerve controlling the swallowing process mainly includes three parts: ① the higher cortex is responsible for initiating and regulating autonomous swallowing; ② reflex coordination of the brain stem deglutition center; ③ Afferent and efferent nerves. The cortical activity associated with swallowing is multidimensional, involving brain regions that process motor, sensory, and attention/emotion tasks [11]. At present, the deglutition cortex centers mainly on the central gyrus, premotor cortex, anterior cingulate gyrus and anterior insula, among which insula, motor area/premotor area control oral voluntary movement and oral deglutition muscle group activity, while posterior inferior frontal gyrus controls tongue and oral movement [12]. In the study of the correlation between the site of cerebrovascular injury and the stages of dysphagia, it is suggested that anterior circulation vessel occlusion is related to oropharyngeal dysphagia, while posterior circulation vessel occlusion and white matter lesions are related to pharyngeal dysphagia [13].
Dysphagia is often manifested as choking on drinking water, difficulty in eating and complications such as aspiration pneumonia, dehydration and malnutrition, and even be life threatening in serious cases [14]. The choice of feeding mode has an important influence on the progress of patients' disease. Feeding mode can be divided into enteral nutrition and parenteral nutrition. Parenteral nutrition is to provide patients with nutrients including amino acids, fats, carbohydrates, vitamins and minerals via vein. Enteral nutrition refers specifically to the administration of enteral nutrition agents through the digestive tract (including oral and tube feeding) [15].Common enteral nutrition methods include nasogastric tube feeding, oral to esophageal tube feeding and gastrostomy. Two systematic reviews on the treatment of stroke with dysphagia were reported several years ago [16, 17]. However, the complications of different nutritional modes and the later recovery of patients’ swallowing function have not been described in a unified manner, and the study scope is narrow. In order to comprehensively evaluate the impact of different feeding techniques on the prognosis of stroke patients with dysphagia, a meta-analysis was conducted.
2 Materials and Methods
This systematic review was conducted based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. All analyses were based on previous published studies, thus no ethical approval and patient consent are required. The review protocol was prospectively developed and registered on the INPLASY website (https://inplasy.com). The DOI number is https://doi.org/10.37766/inplasy2022.2.0014.
2.1 Data Sources and Search Strategy
We searched the Cochrane Library, PubMed, Medline, China National Knowledge Infrastructure (CNKI), Wanfang, and the VIP database. The search period is from the library’s establishment to December 31, 2021.The search terms we used were as following: (stroke OR cerebral apoplexy OR Ischemic stroke OR cerebral ischemic stroke OR ischemic cerelral infarction OR ischemic cerebral stroke) AND (dysphagia OR deglutition disorders OR deglutition OR swallowing disorders) AND (Nasogastric Tube OR Percutaneous Endoscopic Gastrostomy OR tube feeding OR gastric tube OR enteric tube OR enteral nutrition OR feeding OR nutrition support). The search strategy was developed first in MEDLINE (via PubMed) and later adapted to all databases.
2.2 Inclusion and Exclusion Criteria
Inclusion criteria: ① Participants: The diagnosis of the included stroke patients met the diagnostic criteria related to stroke, and the dysphagia was confirmed by internationally recognized and promoted swallowing assessment tools such as the water swallow test; ② Intervention: During the study, the experimental group adopted completely different nutritional methods from the control group. Other treatments were the same as the control group; ③ Study: The trial was limited to randomized controlled trial (RCT).
Exclusion criteria: ① Non-Chinese or English articles; ② the whole article cannot be queried; ③ the data of the article is incomplete and the NOS score is lower than 6; ④ Repeated articles; ⑤ animal trials.
2.3 Paper Quality Evaluation
The risk of bias for each study was assessed using the Cochrane Risk of Bias Scale [46], which took into account aspects of bias related blindness, allocation hiding, and selective reporting of results. Among the 14 included studies, 13 were at medium risk, and 1 study was judged to be at high risk due to incomplete presentation of results (loss to follow-up), as shown in Fig. 5 for details. These assessments were made by two authors, In the above process, any differences between reviewers are discussed or a third reviewer.
2.4 Data Extraction
Two researchers independently screened the literature, extracted the data and cross-checked against inclusion and exclusion criteria. Differences, if any, will be resolved through discussions or negotiations with third parties.
Data extracted in this meta-analysis included first author, publication year, age, sample size, intervention measures, intervention duration, and intervention outcomes. The intervention results included hemoglobin, total serum protein, BMI, VGF and the number of effective patients with improved swallowing function. Among them, the improvement of dysphagia was effectively defined as “the swallowing function of patients after intervention was improved compared with that before intervention according to the data such as water swallow test or VFSS score”. Standardized mean difference (SMD), relative risk (RR), and odds ratio (OR) were calculated using a random-effects model.
2.5 Statistical Analysis
All statistical analyses were performed using RevMan software 5.4 (The Cochrane Collaboration, Oxford, UK) [18]. We considered I2 < 30% low statistical heterogeneity, ≥ 30% to < 50% moderate heterogeneity, ≥ 50% to < 75% substantial heterogeneity, and ≥ 75% considerable heterogeneity.
3 Results
3.1 Study Selection and Study Characteristics
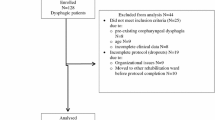
We found that 17 studies satisfied our inclusion criteria, but 3 were considered to contain insufficient data. Due to their age, we could not obtain complete data, so they were excluded from this study [19,20,21]. In the end, we identified 14 studies that provided all the data needed for the analysis. The PRISMA flow chart is shown in Fig. 1, and the details of the included studies are shown in Table 1.
The 14 studies included a total of 1115 patients. 3 of the studies did not mention whether the patients were diagnosed with cerebral infarction or cerebral hemorrhage [22,23,24], and the remaining 11 studies showed specific numbers of cerebral infarction and cerebral hemorrhage. What is worth mentioning that among the 16 studies included in this meta-analysis, there was no significant difference between the basic situation of the experimental group and the control group before the implementation of intervention measures (P ≥ 0.05).
3.2 Meta-analysis Outcomes
Only studies with the same outcome indicators ≥ 2 were pooled.
3.2.1 IOE VS NG
3.2.1.1 Hemoglobin Level
3 studies [22, 25, 26] included hemoglobin as an outcome measure, and pooled data from four randomized controlled trials showed that IOE significantly increased hemoglobin levels in stroke patients with dysphagia (MD 5.64, 95%CI 2.65–8.63, P = 0.0002, I2 = 39%; Fig. 2a).
3.2.1.2 Serum Albumin
3 studies22,25,26 included hemoglobin as an outcome measure, and pooled data from four randomized controlled trials showed that IOE significantly increased Serum albumin levels in stroke patients with dysphagia (MD 1.95, 95%CI 1.22-2.67, P<0.00001, I2= 0%; Fig. 2b).
3.2.1.3 Pneumonia
4 studies [23, 27,28,29] included the number of pulmonary infections as an outcome indicator, and pooled data from five randomized controlled trials showed that compared with NG, IOE can significantly reduce the incidence of pulmonary infection. (RR 0.39, 95%CI 0.23–0.66, P = 0.0004, I2 = 0%; Fig. 2c).
3.2.1.4 Swallowing Function
5 studies [23, 26,27,28,29] included the number of swallowing function as an outcome indicator, Swallowing function was graded according to the Wa Tian drinking water test [30]. The pooled data from five randomized controlled trials showed that compared with NG, IOE can significantly improved swallowing function. (OR 3.92, 95%CI 2.15–7.14, P < 0.00001, I2 = 0%; Fig. 2d).
3.2.2 NJ VS NG
3.2.2.1 Pneumonia
3 studies [31,32,33] included the number of pulmonary infections as an outcome indicator, and pooled data from five randomized controlled trials showed that compared with NG, NJ can significantly reduce the incidence of pulmonary infection. (RR 0.51, 95%CI 0.29–0.92, P = 0.03, I2 = 0%; Fig. 3).
3.2.3 PN VS NG
3.2.3.1 Pneumonia
3 studies [34,35,36] included the number of pulmonary infections as an outcome indicator, and pooled data from five randomized controlled trials showed that compared with PN, NG can significantly reduce the incidence of pulmonary infection. (RR 0.53, 95%CI 0.36–0.79, P = 0.001, I2 = 0%; Fig. 4).
3.3 Publication Bias and Sensitivity Analyses
As shown in Figs. 5 and 6, of the 14 studies included, 1 study had one high-risk bias factor. Due to the large difference in the number of deaths between the intervention group and the control group, loss of follow-up bias was considered as high risk in 1 study [24]. All studies are defined as unclear bias because they fail to elaborate performance bias in the article.
A sensitivity analysis was also conducted, in which 1 study at a time was removed and the other analyzed estimate whether the results could have been affected markedly by a single study. This analysis confirmed the stability of our results.
4 Dicussion
The meta-analysis showed that 3 of the 14 included studies compared the prognostic effects of enteral nutrition and parenteral nutrition on dysphagia after stroke. The results showed that enteral nutrition was less likely to cause post-stroke pneumonia than parenteral nutrition in patients with post-stroke dysphagia. Hemoglobin and serum albumin were included in 2 of the 3 studies, which were not included in this meta-analysis due to the lack of research data. However, two studies [35, 36] indicated that enteral nutrition was better than parenteral nutrition in improving the nutritional level of patients. Enteral nutrition means that nutrients are absorbed through the intestine, which is in line with normal physiological functions of the human body, but requires the presence or partial presence of intestinal absorption function in patients. This relatively normal physiological function can further promote the recovery of intestinal function. In addition, frequent food stimulation can promote the growth of intestinal epithelial cells, maintain the intestinal acid–base balance, and reduce the occurrence of intestinal dysfunction [37].
Percutaneous endoscopic gastrostomy was first used as an alternative to enteral feeding in 1981 by Ponsky and Gauderer [38]. There have been many reports that PEG surgery has a very high success rate (about 95%) [39, 40] and a low mortality rate (0–1%) [41, 42]. However, with the in-depth study of PEG treatment, some studies have shown that PEG patients are more prone to medical complications (pneumonia, cardiac events, stroke progression) than NG patients, and death events are also more common in patients in the PEG group [19]. In this meta-analysis, only one randomized controlled study on PEG was included. During this study [24], statistics showed that the NG group lost about 22% of tube feeding nutrients compared with the PEG group. Among them, most of the patients who used PEG as a supplementary nutrition method took a small amount of oral feeding at the same time. On the contrary, 71% of the patients with nasogastric feeding tube lost about 1 day of food intake due to delayed feeding. This may be an important reason why the nutritional indicators of patients in NG group were significantly lower than those in PEG group. However, this study did not use the patient's pulmonary infection rate and recovery of swallowing function as outcome indicators, and the number of deaths in the study outcome was too large and the study time was short. Therefore, it is believed that PEG can indeed quickly restore the nutritional status of patients in a short period of time, but The long-term prognosis and survival rate of patients are still under discussion.
Campbell-Taylor et al [43] were the first to propose IOE as an alternative to PEG and NG as a feeding aid. IOE has many advantages [44]: ① The total time of using the tube is short, thus reducing the mental stress and adverse reactions of patients; ② Intermittent tube feeding can avoid the risk of gastroesophageal reflux, pharyngeal bacterial colonization and skin or mucosal ulcers; ③ Oral tube insertion can stimulate the oral cavity and pharynx and improve swallowing function.Results of 7 randomized controlled studies included in this study, 3 studies [22, 25, 26] analyzed nutritional indicators, 4 studies [23, 27,28,29] studied the occurrence of pneumonia, and 5 studies [23, 26,27,28,29] analyzed the recovery of swallowing function, all of which confirmed these advantages. Compared with NG, IOE can significantly increase serum albumin and hemoglobin levels, reduce the incidence of post-stroke pneumonia, and improve the swallowing function of patients. However, because IOE is suitable for patients with normal esophagus, stomach, and intestinal digestive functions, if the patient has esophageal obstruction (such as cancer of the middle and lower esophagus), gastrointestinal ulcer perforation, pyloric obstruction, short bowel syndrome, etc., the patient cannot absorb food normally. This method of eating does not apply. In addition, it should be noted that if the patient has serious disturbance of consciousness, the diastolic function of the lower esophagus will be limited in the recumbent position, and food will be trapped in the lower esophagus after the use of IOE. After the change of position, the risk of choking or even lung infection will increase.
Most stroke patients end up with aspiration pneumonia, which seriously affects the disease progression of patients. Results of 3 studies included in this meta-analysis showed that NJ was less likely to cause post-stroke pneumonia than NG during long-term nasal feeding. The nasoenteric tube passes through the duodenal curved ligament, and the sphincter can effectively reduce the occurrence of reflux and the possibility of aspiration pneumonia. Among these 3 studies, 2 of them took relevant nutritional indicators as the research results, and 3 of them took aspiration pneumonia as the research outcome. Due to incomplete research data, nutritional indicators were not included in this meta-analysis. However, in the two studies [32, 33], it was expounded from different perspectives that NJ can significantly improve the nutritional level of dysphagia patients after stroke compared with NG.
There are some limitations to this study. First, the inclusion criteria for this study were limited to Chinese and English literature, which limited the number of included studies to a certain extent. Second, most of the included studies (except for the study by Norton B et al.) selected intervention and control groups from the author’s own hospital, and there may be regional differences. In the future, new RCT trials can be conducted to establish a multi-center randomized controlled trial to narrow regional and population differences by adopting a whole-society approach of recruiting patients with post-stroke dysphagia.
It is worth mentioning that any nutritional method has its advantages and disadvantages. Patients with different levels of knowledge choose different nutritional methods. In the research report of Fang Lixuan et al. [45], it was suggested that the acceptance of IOE in patients was moderate, and the acceptance gradually decreased with age. It can be seen that patients who do not accept IOE enteral feeding and choose nasal feeding for various reasons can consider choosing NJ as a long-term enteral feeding method, and be alert to the occurrence of adverse events during supplementary nutrition.
Data Availability
Detailed Data can be found through “Data Sources and Search Strategy”.
References
Collaborators GN. Global, regional, and national burden of neurological disorders, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(5):459–80. https://doi.org/10.1016/s1474-4422(18)30499-x.
Zhang T, Zhao J, Li X, et al. Chinese Stroke Association guidelines for clinical management of cerebrovascular disorders: executive summary and 2019 update of clinical management of stroke rehabilitation. Stroke Vasc Neurol. 2020;5(3):250–9. https://doi.org/10.1136/svn-2019-000321.
Yanyan W. Research progress of deglutition training and acupoint massage in the treatment of dysphagia after stroke. J Nurs Sci. 2016;31(05):106–10.
Chunlian L, Yan Q, Xiaohong L, Fengxia W, Yuan Z, Lehua Y. Clinical observation on the treatment of stroke complicated with dysphagia by low frequency pulse electrical stimulation combined with swallowing function training. Chongqing Med J. 2012;41(22):2247–8.
Guomin J. Comprehensive rehabilitation nursing of dysphagia in acute cerebral apoplexy patients. Chin J Pract Neurol Dis. 2007;06:146.
Shaoshi W. Expert consensus on nutrition management of Stroke patients in China. Chin J Cerebrovasc Dis. 2007;(05):211–213.
Duncan P, Zorowitz R, Bates B, et al. Management of adult stroke rehabilitation care: a clinical practice guideline. Stroke. 2005;36(9):e100–43. https://doi.org/10.1161/01.Str.0000180861.54180.Ff.
Ovbiagele B, Goldstein L, Higashida R, et al. Forecasting the future of stroke in the United States: a policy statement from the American Heart Association and American Stroke Association. Stroke. 2013;44(8):2361–75. https://doi.org/10.1161/STR.0b013e31829734f2.
Cheung K, Lau V, Un K, Wong M, Chan K. Advance care planning for patients with advanced neurology diseases. J Ann Palliat Med. 2018;7(3):349–54. https://doi.org/10.21037/apm.2017.09.10.
Yunmei Y. Diagnosis and management of senile aspiration pneumonia. Chin J Crit Care Med. 2010;3(03):150–8.
Hamdy S, Mikulis D, Crawley A, et al. Cortical activation during human volitional swallowing: an event-related fMRI study. Am J Physiol. 1999;277(1):G219–25. https://doi.org/10.1152/ajpgi.1999.277.1.G219.
Galovic M, Leisi N, Müller M, et al. Lesion location predicts transient and extended risk of aspiration after supratentorial ischemic stroke. Stroke. 2013;44(10):2760–7. https://doi.org/10.1161/strokeaha.113.001690.
Kim SY, Kim TU, Hyun JK, Lee SJ. Differences in Videofluoroscopic Swallowing Study (VFSS) findings according to the vascular territory involved in stroke. Dysphagia. 2014;29(4):444–9.
Maeshima S, Osawa A, Hayashi T, Tanahashi N. Factors associated with prognosis of eating and swallowing disability after stroke: a study from a community-based stroke care system. J Stroke Cerebrovasc Dis Off J Natl Stroke Assoc. 2013;22(7):926-930.e1.
Hanping S, Xiaolin W, Yun Y. Analysis of some terms in clinical nutrition. E J Tumor Metab Nutr. 2019;6(2):6.
Fangping D, Jinhui T, Huiju L. Meta-analysis of the effectiveness of different nutritional support methods in patients with dysphagia after stroke. Evid Based Nurs. 2019;5(03):203–11.
Shin H, Koo K, Hwang C. Intermittent oroesophageal tube feeding via the airway in patients with dysphagia. Ann Rehabil Med. 2016;40(5):794–805. https://doi.org/10.5535/arm.2016.40.5.794.
Higgins J, Thompson S, Deeks J, Altman D. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60. https://doi.org/10.1136/bmj.327.7414.557.
Hamidon B, Abdullah SA, Zawawi MF, Sukumar N, Raymond AA. A prospective comparison of percutaneous endoscopic gastrostomy and nasogastric tube feeding in patients with acute dysphagic stroke. Med J Malaysia. 2006;61(1):59–66.
Clarke J, Cranswick G, Dennis MS, Flaig R, Lewis SC. Effect of timing and method of enteral tube feeding for dysphagic stroke patients (FOOD): a multicentre randomised controlled trial. Dkgest World Latest Med Inf. 2005;365(9461):764–72.
Shaochun H, Haiyan C, Weibo S. Effect of two kinds of tube feeding on dysphagia after stroke. Chin J Rehabil Theory Pract. 2012;18(12):3.
Lin Y, Jun G, Ganghua G, Zhe L, Yingna W. Effect of intermittent oral and gastric tube feeding on dysphagia after stroke %J. Chin J Rehabil Med. 2021;36(04):426–30.
Aixia W. Application of intermittent oral tube feeding in stroke patients with dysphagia. master. Zhengzhou: Zhengzhou University; 2015.
Norton B, Homer-Ward M. A randomised prospective comparison of percutaneous. Br Med J. 1996;312:13–6.
Xiulin Z, Xuanyan Z, Yanhong D, Wenyuan C. Effects of oral intermittent tube feeding on nutritional status and quality of life in patients with dysphagia after stroke. Shanxi Med. 2017;46(12):4.
Xi Z, Dejun W, Liugen W, et al. Effects of intermittent oral nutrition tube assisted feeding on nutritional status of stroke patients with dysphagia. Chin J Phy Med Rehabil. 2011;09:703–5.
Minru Z, Ling P, Lane Z, Huiqiu Y, Lili W, Jingru M. Effect of intermittent tube feeding combined with swallowing training on patients with dysphagia after stroke. Chin J Phys Med Rehabil. 2017;39(12):932–3.
Juan W, Zhen H, Yan-Ying F, et al. A comparative study of two tube feeding methods in patients with dysphagia after stroke: a randomized controlled trial. J Stroke Cerebrovasc Dis Off J Natl Stroke Assoc. 2020;29(3): 104602. https://doi.org/10.1016/j.jstrokecerebrovasdis.2019.104602.
Mengling W, Chunxia L, Liqun Y, et al. Effect of intermittent transorogastric tube nasogastric feeding on dysphagia. Guangdong Med Coll. 2017;38(S1):57–9. https://doi.org/10.13820/j.cnki.gdyx.2017.s1.019.
Zulin D (2009). Evaluation and treatment of dysphagia. Evaluation and treatment of dysphagia.
Xiaohong C, Genying P. Effects of different gastrointestinal nutritional support modes on post-stroke associated pneumonia. Med Theory Pract. 2016;29(09):1155–7. https://doi.org/10.19381/j.issn.1001-7585.2016.09.016.
Nanyuan G, Ning C, Huayao L, Longhuan Z. Effect analysis of naso-enteral nutrition combined with swallowing rehabilitation training on cerebral apoplexy. Zhejiang Clin Med J. 2018;20(6):2.
Yuling G, Chengshuai Z, Juan X, Tingting D. Effect of enteral nutrition catheterization on short-term prognosis of severe stroke patients. Qilu Nurs J. 2020;26(19):3.
Xiangqun S, Shiyao B, Yunliang W. Effects of nasogastric enteral nutritional support on swallowing function and infection complications after acute stroke. Chin J Geriatr. 2003;22(8):2.
Rui C, Yixian L. Clinical observation of enteral nutritional support in convalescent stroke patients with dysphagia. Parenter Eteral Nutr. 2010;17(6):3.
Yali P. Nursing coordination of dysphagia assessment and nutritional support in stroke patients. Chin J Pract Neurol Dis. 2014;11:128–9.
Arai K, Sumi Y, Uematsu H, Miura H. Association between dental health behaviours, mental/physical function and self-feeding ability among the elderly: a cross-sectional survey. Gerodontology. 2003;20(2):78–83. https://doi.org/10.1111/j.1741-2358.2003.00078.x.
Ponsky J, Gauderer M. Percutaneous endoscopic gastrostomy: a nonoperative technique for feeding gastrostomy. Gastrointest Endosc. 1981;27(1):9–11. https://doi.org/10.1016/s0016-5107(81)73133-x.
Wolfsen H, Kozarek R, Ball T, Patterson D, Botoman V, Ryan J. Long-term survival in patients undergoing percutaneous endoscopic gastrostomy and jejunostomy. Am J Gastroenterol. 1990;85(9):1120–2.
Foutch P, Woods C, Talbert G, Sanowski R. A critical analysis of the Sacks-Vine gastrostomy tube: a review of 120 consecutive procedures. Am J Gastroenterol. 1988;83(8):812–5.
Larson D, Burton D, Schroeder K, DiMagno E. Percutaneous endoscopic gastrostomy. Indications, success, complications, and mortality in 314 consecutive patients. Gastroenterology. 1987;93:48–52.
Ponsky J, Gauderer M, Stellato T, Aszodi A. Percutaneous approaches to enteral alimentation. Am J Surg. 1985;149(1):102–5. https://doi.org/10.1016/s0002-9610(85)80017-9.
Campbell-Taylor I, Nadon GW, Sclater AL, Fisher R, Rosen I. Oro-esophageal tube feeding: an alternative to nasogastric or gastrostomy tubes. Dysphagia. 1988;2(4):220–1.
Nakajima M, Kimura K, Inatomi Y, et al. Intermittent oro-esophageal tube feeding in acute stroke patients – a pilot study. Acta Neurol Scand. 2006;113(1):36–9. https://doi.org/10.1111/j.1600-0404.2005.00534.x.
Lixuan F, Meilan Z, Shufang C, Xiaoyang L, Tianwen H. Investigation on the acceptance status of intermittent oral to esophageal tube feeding gastrointestinal nutrition in patients with dysphagia. Chin J Rehabil Med. 2020;35(3):3.
Acknowledgements
Thanks to everyone in the team for their hard work and thanks to Mr. Yue Xiu-xu for his language guidance.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
Study design, manuscript revision: Li Heping; Writing manuscripts, conduct retrieval, screen retrieved papers according to inclusion criteria, data extraction from selected papers, data analysis: Wang Shaowei; Performing literature search and eligible paper selection: Zeng Xi, Zhang Qiongshuai. All the authors approved the final version of the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest associated with this manuscript.
Ethical Approval
All analyses were based on previous published studies, thus no ethical approval and patient consent are required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, S., Zeng, X., Zhang, Q. et al. Effectiveness of Different Feeding Techniques for Post-stroke Dysphagia: An Updated Systematic Review and Meta-analysis. Intensive Care Res 2, 108–116 (2022). https://doi.org/10.1007/s44231-022-00022-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44231-022-00022-3