Abstract
Background
Since October 2021, multiple paediatric cases of severe acute hepatitis of unknown aetiology (SAHUA) not caused by hepatitis A–E viruses have been reported by multiple countries. As of 14 September 2022, approximately 1296 probable cases of SAHUA in 37 countries and regions had been reported.
Objectives
The purpose of this study was to present a complete picture of this outbreak, including its origin, current cases, clinical signs, possible hypotheses, and potential treatments.
Methods
A thorough search for literature from October 2021 to September 2023 was performed in the PubMed and Medline databases. Additional websites, including the WHO, CDC, ECDC, and the UKHSA, were searched for further relevant data.
Results
Common clinical symptoms include jaundice, vomiting, pale stools, diarrhoea, abdominal pain, and nausea, whereas fever is infrequent. Elevated AST and ALT are prevalent, and most cases test positive for adenovirus. However, immunohistochemical staining on liver tissue often yields negative results for adenovirus, thus challenging the hypothesis that adenovirus is a definitive cause. A recent compelling hypothesis has implicated AAV-2 as a likely etiologic agent of SAHUA in paediatric cases involving abnormal AAV-2 replication products and immune-mediated hepatic disease. Evidence of low immunogenicity, tissue tropism, and immune responses supports this hypothesis. SARS-CoV-2's role has also been explored. Some SAHUA cases have SARS-CoV-2 IgG positivity even when PCR tests are negative, thereby suggesting silent prior infections. Cidofovir, a suggested treatment for severe human adenovirus infection in immunocompromised patients, has not decreased adenoviral load in two cases. Notably, 29 deaths have been reported, and 55 cases have required or received liver transplant.
Conclusion
SAHUA in children presents a complex challenge with potential involvement of AAV-2 and immune-mediated factors. SARS-CoV-2 may affect disease severity—a possibility warranting further investigation. Treatment options include diagnostics, supportive care, antivirals, and immunosuppression. Prevention relies on infection control measures, and management requires advanced diagnostics and international collaboration. SAHUA remains an enigma, thus underscoring the need for continued research and adaptability to emerging infectious threats.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Hepatitis is a medical condition characterized by inflammation of the liver, which can result in serious health consequences, including liver cirrhosis, liver cancer, and death [1]. Five types of hepatitis viruses are known to cause this infection: hepatitis A virus (HAV), hepatitis B virus (HBV), hepatitis C virus (HCV), hepatitis D virus (HDV), and hepatitis E virus (HEV) [1]. HAV and HEV are typically transmitted through ingestion of contaminated food and/or water, whereas HBV, HCV, and HDV are transmitted through contact with infected bodily fluids [2].
In 2021, a new and concerning form of hepatitis emerged in children worldwide, and cases were reported in multiple countries. This severe acute hepatitis of unknown aetiology (SAHUA) is not caused by the common hepatitis A–E viruses [3]. The first cases were reported in a children's hospital in Alabama in October to November of 2021 [4]. Five months later, in early April 2022, more cases were reported across Central Scotland [5]. Since then, cases have spread throughout Europe, thus making the disease a worldwide issue and a concerning trend. Consequently, healthcare providers were encouraged by a health advisory from the Centers for Disease Control and Prevention (CDC) to report any cases in children younger than 10 years diagnosed with hepatitis of unknown aetiology to public health authorities [6]. As of July 2022, the World Health Organization (WHO) has reported 1010 cases of SAHUA in 35 countries [7]. More recently, as of 14 September 2022, approximately 1296 probable cases of acute hepatitis with an unknown cause have been reported from 37 countries and regions [8].
In the face of a new outbreak, understanding multiple aspects is crucial for implementing effective measures to eradicate disease spread and prevent further harm. Although previous studies have explored the potential aetiologies of this SAHUA and the number of reported cases [9,10,11,12], gaps exist in understanding of this form of hepatitis in children in the past several decades, as well as the recommended hospital care and potential management and treatment options. Therefore, the purpose of this review was to comprehensively assess the current outbreak, its origin, past and present cases, clinical manifestations, and available management and treatment options, to fill in gaps in the understanding of this serious public health concern.
2 Methods
We conducted a comprehensive review focusing on the period from October 2021 to September 2023 to examine the epidemiological aspects of the current severe acute hepatitis in children. Our aim was to gather the most current information available during this specific timeframe. We used a rigorous strategy for searching the PubMed and Medline databases. The search string used was ((hepatitis [MeSH] AND acute disease [MeSH]) OR acute hepatitis OR acute viral hepatitis OR liver failure, acute [MeSH]) AND (unknown OR idiopathic) AND (children OR child OR pediatric OR paediatric OR adolescent OR adolescence).
The inclusion criteria for the articles in our review were as follows: (1) studies focusing on the new strain of severe acute hepatitis in children; (2) studies relevant to acute hepatitis in children, encompassing epidemiological and clinical characteristics, diagnosis, and treatment; (3) original articles, such as case reports, case series, and prospective and retrospective studies, as well as previous reviews; (4) articles published in English between October 2021 and September 2023; and (5) studies from all countries. The exclusion criteria were as follows: (1) articles focused on the adult population; (2) articles focused on hepatitis cases of known origin; and (3) articles focused on hepatitis cases before October 2021.
Given the limited availability of primary research studies specifically focused on acute hepatitis in children, we extended our search to other reputable sources, including the WHO, the CDC in the United States, the European Centre for Disease Prevention and Control (ECDC), and the UK Health Security Agency. Our review process was completed on 7 September 2023, to ensure that the most current information was considered for our study during this specific timeframe.
3 Results
Through this comprehensive approach, we identified and analysed 62 articles that strictly adhered to our inclusion criteria. Six were case reports/series that met the case definition, which we subjected to a separate analysis.
We classified our findings into five main categories: (1) case definitions, (2) epidemiology of the disease, (3) symptoms and laboratory findings, (4) hypotheses regarding possible etiologic agents/factors, and (5) case reports/series between October 2021 and August 2023.
3.1 Case Definition
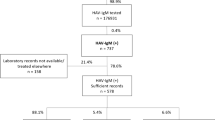
Figure 1 shows the case definition for suspected cases of SAHUA in children. Currently, the most common case definitions of SAHUA (non-hepatitis A–E) are those provided by the WHO and the ECDC. No definitions are currently available for confirmed cases; however, probable cases were described as “child with acute hepatitis (non-hepatitis A, B, C, D, and E viral infection) and serum transaminase (ALT or AST) > 500 IU/L, age ≤ 16 years old, since 1 October 2021” [3]. Additionally, an epidemiologically linked case was reported as “a person of any age with acute hepatitis (non-hepatitis A, B, C, D, and E viral infection) who had close contact with the probable case since 1 October 2021” [3].
The American CDC has also provided a case definition of “children < 10 years of age with elevated aspartate aminotransferase (AST) or alanine aminotransferase (ALT) (> 500 U/L) who have an unknown aetiology for their hepatitis” [6]. The case definition provided by the UK Health Security Agency (UKHSA) for a confirmed case is “the presence of acute hepatitis with elevated level(s) of ALT or AST higher than 500 IU/L, and negativity for viral hepatitis (A–E) in children aged 10 years or less any time from 1 January 2022” [13]. Furthermore, a probable case has been described as “the presence of acute hepatitis with elevated level(s) of ALT or AST higher than 500 IU/L, and negativity for viral hepatitis (A–E) in those aged between 11 and 16 years any time from 1 January 2022” [13]. An epidemiologically linked case has been described as “the presence of acute hepatitis in a person who has been in close contact with a probable case of acute non-hepatitis A–E hepatitis, any time from 1 January 2022” [11, 13].
The main differences among case definitions relate to the definition of a child. The WHO defines children as people 16 years or younger, whereas the CDC and UKHSA defines children as people 10 years or younger [6, 7, 13]. The WHO also has not provided a confirmed case definition for acute hepatitis.
3.2 Epidemiology of the Disease
Instances of children presenting to hospitals with acute hepatitis of unknown origin began in October 2021 in the United States [4]. A significant increase in the average annual number of cases was reported, with an average of 16.3 cases in 2018–2021, compared with a twofold increase (33 cases) in 2021–2022 [14]. A CDC report by Baker et al. has identified five cases of SAHUA (non-hepatitis A–E) occurring between October and November 2021 at a children’s hospital in Alabama, and an additional four cases between November of 2021 and 1 February 2022 [4]. No epidemiological links were found among these cases, and the median age of onset was 2 years and 11 months [4]. Seven of nine patients were girls, and none were immunocompromised. No deaths were reported; however, two liver transplantations were necessary because of acute liver failure [4]. According to the WHO’s most recent report, as of 8 July 2022, 1010 cases of acute hepatitis of unknown aetiology have been reported in 35 countries, among which 17 countries have reported five or more probable cases [7]. Most probable cases have occurred in the United States (n = 346), United Kingdom (n = 277), Canada (n = 27), and Europe (n = 242 across 20 countries), and cases have also been reported in Central and South America, the Western Pacific Region, Southeast Asia, and the eastern Mediterranean [7, 15]. In addition, 48% of cases were in boys, whereas 76% of cases were in children under 6 years of age [7]. Previous studies have also demonstrated that cases have occurred primarily in children 1 month to 16 years of age, most of whom have been younger than 10 years [4, 5, 7, 13, 16,17,18]. Three studies have reported a median age between 3 and 5 years [5, 11, 19]. Furthermore, 22 fatalities have occurred, and 46 (5%) of children have required liver transplantation [7]. More recently, as of 14 September 2022, approximately 1296 probable cases of acute hepatitis with an unknown cause have been reported from 37 countries and regions [8].
3.3 Symptoms and Laboratory Findings
The most common clinical symptoms in children experiencing acute hepatitis include jaundice, vomiting, pale stool, diarrhoea, abdominal pain, and nausea, whereas fever is absent in most cases [4, 12, 19,20,21,22]. Laboratory examinations and findings demonstrate elevated levels of AST and ALT, and most cases test positive for adenovirus DNA with real-time polymerase chain reaction (PCR) [4, 12, 19,20,21,22,23]. According to the CDC, a laboratory analysis from an outbreak in Alabama has found that some affected children tested positive for a specific type of adenovirus, adenovirus type 41 [24]. This type of adenovirus is known to cause severe stomach illness in children but is not considered a common cause of hepatitis in healthy children [24]. Moreover, adenovirus infection has been detected in 45% of 299 patients tested for adenovirus on any specimen type (blood, respiratory, or stool specimens) [6]. The ECDC and UKHSA, in contrast, have found adenovirus positivity in more than half of patients (53.9% and 64.7%, respectively) [13, 25]. In England and Scotland, almost 50% of patients presenting with acute hepatitis have tested positive for human adenoviruses [19, 21].
With respect to detection of hepatitis A, B, C, and E, several reviews conducted in different countries, such as the United States and other European countries, have reported hepatitis A, B, C, and E negativity in all observed cases [4, 19, 23]. For SARS-CoV-2 infection, positive PCR tests have been observed in 10.6% of 273 cases and 17% of 196 cases in ECDC and UKHSA reports, respectively [13, 25]. Another study by Frediansyah et al. has reported SARS-CoV-2 infection positivity in 18% (24 of 132) of patients [19].
3.4 Hypotheses Regarding Possible Aetiologic Agents/Factors
Since the emergence of acute hepatitis in children in 2022, most studies in the broader literature have explored possible aetiologies and causes of the outbreak. Several possible explanations have been suggested, given the ambiguity of causes of acute hepatitis. Over time, the definitive diagnosis of different types of hepatitis (e.g., hepatitis A, B, C, D, or E) has usually been based on the detection of specific immunoglobulin antibodies through serological testing. However, laboratory testing to detect hepatitis A–E viruses in children presenting with SAHUA has yielded negative results [26]. Therefore, the exact aetiology remains unknown, and further investigations and laboratory testing remain necessary. Previous studies have suggested the following aetiologies, which remain under investigation.
3.4.1 Adenovirus
The aetiology most frequently reported by several studies conducted in the United States, United Kingdom, Scotland, and other European countries is human adenovirus infection [5, 26,27,28]. According to an updated report by the joint European CDC and the WHO Regional Office for Europe, of the 364 children presenting with acute hepatitis who were tested for human adenovirus in any specimen type, 192 (52.7%) tested positive [25]. Similar results have been reported by the CDC, in which 45% of 252 cases tested for adenovirus had a positive result [6]. In further investigations, demographic factors, such as the age, sex, race, ethnicity, region, previous SARS-CoV-2 infection history, and medical history of these children, have been collected. None of these factors have been associated with this new outbreak, and no epidemiological links among children have been identified [26].
The CDC therefore hypothesized that a new strain of adenovirus might have emerged and caused this unique type of hepatitis [29]. Human adenovirus is a common infectious agent that spreads through respiratory droplets, close personal contact, or fomites. It infects primarily the respiratory tract and is a self-limiting disease. Less commonly, it causes other illnesses such as conjunctivitis, gastroenteritis, cystitis, and, more rarely, neurological diseases. Among its many immunological types, serotypes 40 and 41 have been associated with gastroenteritis, fever, vomiting, and diarrhoea, the most common presenting symptoms [29]. Among the small number of samples tested in the United Kingdom and Alabama, human adenovirus type 41 (HAdV-F41) was detected in 27 of 35, and 5 of 9 samples, respectively [4, 26, 30]. In previous cases, hepatitis caused by adenovirus had been reported in only immunocompromised patients; in contrast, in current outbreaks (October 2021 to July 2022), it has been recurrently detected among immunocompetent patients. Moreover, the association between HAdV-F41 and hepatitis in healthy individuals had not been previously described in the literature [12]. Consequently, these findings presented new opportunities for researchers.
Interestingly, viral metagenomic studies of clinical samples from SAHUA in 2022 and 2023 revealed that a substantial portion of affected children test positive for adenovirus, specifically HAdV-F41, the most common adenovirus type in these cases [31,32,33,34,35,36,37]. Equally intriguingly, adeno-associated virus-2 (AAV-2) has been found to be present in most SAHUA cases [38, 39]. AAV-2 typically relies on a ‘helper virus’ for replication, such as adenovirus (particularly HAdV-F41) or human herpesvirus 6B (HHV-6B), as proposed in some cases [31, 32, 36, 38,39,40,41,42]. AAV-2 is usually considered harmless and does not cause disease. Thus, its association with severe liver disease prompted questions as to why it elicited such symptoms.
The association of both HAdV-F41 and AAV-2 with this hepatitis outbreak challenged conventional understanding. Researchers have used VirScan, a high-throughput antibody profiling technology, to investigate potential viral causes of acute hepatitis in children [40]. Elevated antibody responses against adeno-associated dependoparvovirus A (AAV-A) have been observed in SAHUA cases compared with controls [40]. Antibody responses specific to AAV-2 have been found to be conserved in seven of nine cases at Children’s of Alabama, but have rarely been observed in paediatric and adult controls [40]. Another study has detected AAV-2 infection in both plasma and liver samples from a substantial majority of cases (26 of 32; 81%) but in only 5 of 74 (7%) samples from unaffected individuals [41]. Liver biopsy samples have indicated the presence of AAV-2 within ballooned hepatocytes, together with substantial T-cell infiltrate [41]. Similarly, high levels of AAV-2 DNA have been detected in the liver, blood, plasma, or stool samples of 27 of 28 cases in the United Kingdom, whereas AAV-2 was rarely detected and, if so, was present at low levels in the blood or liver samples of control children, including those with adenovirus present and those who were significantly immunosuppressed [42]. In Ireland, a strong correlation has been detected between the circulation of HAdV-F41 and AAV-2 in the community, in wastewater samples, and the occurrence of SAHUA clinical cases [32, 43]. Environmental analysis has indicated elevated community prevalence of both HAdV-F41 and AAV-2 during the outbreak of SAHUA, thus supporting the potential roles of these viruses in SAHUA [32, 43]. Possible mutations in HAdV-F41 and AAV-2 have been suggested to account for their unusual behaviour. Some patients have been found to have specific genetic markers that might have affected their susceptibility to viral infections [31].
A remarkable study in May 2023 [44] has revealed that SAHUA in children is intricately associated with co-infections, and AAV-2 has emerged as a critical player, along with one or more auxiliary viruses. Intriguingly, alongside the detection of AAV-2, this study highlighted the presence of co-infections involving Epstein-Barr virus, human herpesvirus 6, and/or enterovirus A71 in most cases, thereby suggesting that a complex web of interactions contributes to the severity of SAHUA [44].
3.4.2 SARS-CoV-2
Because of the COVID-19 pandemic and the inability to attribute the severity of the clinical manifestations of the current acute hepatitis entirely to the presence of adenovirus, the co-occurrence of COVID-19 and acute hepatitis has been considered as a possible aetiology. Countries with higher frequencies of Omicron SARS-CoV-2 infection have been found to have a greater likelihood of experiencing SAHUA [45]. Studies have emphasized the relationship of SARS-CoV-2 with liver injury, which is characterized by elevated serum liver biochemistry analytes. Possible explanations for this finding include immunological reactions, direct cytotoxicity of the pathogen, anoxia, drug induced injury, and reactivation of pre-existing liver disease [46]. SARS-CoV-2 has been suggested to play a role in SAHUA by triggering multisystem inflammatory responses through immune activation [45]. Thus, the immune response to SARS-CoV-2 superantigens might lead to liver immunopathology, particularly in children [36, 45, 47]. On the basis of this hypothesis, the CDC and WHO have called for further testing and evaluation of SARS-CoV-2 infection co-occurring with acute hepatitis. Currently, SARS-CoV-2 has been detected in 34 of 196 United Kingdom cases of acute hepatitis after hospital admission [13]. Moreover, an ECDC report has demonstrated 10.9% positivity in COVID-19 tested samples [25]. In contrast, none of the nine cases of acute hepatitis in children admitted to a children’s hospital in Alabama had COVID-19 positivity, and the SARS-CoV-2 results were negative in 8 of 13 cases of acute hepatitis in Scotland [4, 5]. In the European region, the rate of SARS-CoV-2 positive acute hepatitis cases is 16%. Consequently, among 335 acute hepatitis cases for which PCR testing results were available, 54 had confirmed SARS-CoV-2 positivity [45]. In another retrospective observational study conducted in India among all paediatric patients with acute hepatitis, the authors discussed a possible interaction between newer COVID-19 variants (e.g., Delta and Omicron) and hepatitis, resulting in a transient form of hepatitis [48]. This new hepatitis might be induced by COVID-19 complications, such as multisystem inflammatory syndrome in children (MIS-C). Interestingly, no cases had any underlying medical conditions. Another study in India has detected antibodies to SARS-CoV-2 in a substantial proportion of cases of acute hepatitis (75%) developing acute liver failure, thus indicating a potential connection between this virus and SAHUA presenting as acute liver failure [49]. Similar results have been found in a case report by Brisca et al., describing a 10-month-old boy who tested positive for COVID-19 and had elevated liver transaminases and ferritin [50]. However, the CDC has stated that hepatic involvement is rarely seen in patients presenting with MIS-C after SARS-CoV-2 infection, and fewer than 1% of these patients develop liver failure [6]. Notably, some patients have positive results for both adenovirus and SARS-CoV-2, thus suggesting that COVID-19 might alter host immunity and result in severe adenovirus infection. In contrast, a study on 40 children with SAHUA in Japan identified none with SARS-CoV-2 infection. However, the proportion of acute hepatitis cases during the COVID-19 era (88%) was higher than that in the pre-COVID-19 era (56%) [51]. At the country level, Nishiura et al. [52] have observed a correlation between countries with higher rates of SARS-CoV-2 Omicron variant infections and higher reported cases of SAHUA, thereby suggesting a potential association between prior exposure to the Omicron variant and the likelihood of children developing severe hepatitis [52].
3.4.3 Autoimmune Hepatitis
Autoimmune hepatitis (AIH), an uncommon progressive liver disease in children, is characterized by elevated IgG levels and autoantibodies, such as antinuclear antibody (ANA), anti-smooth muscle antibody (ASMA), anti-actin antibody (AAA), and anti-mitochondrial antibody (AMA). AIH has a histopathological pattern of interface hepatitis that differentiates it from acute hepatitis. The disease is activated primarily in genetically susceptible individuals after exposure to triggers including toxins, drugs, viruses, and vaccines, thus eventually mediating a T-cell immune response against liver autoantigens [53]. According to the existing literature, both SARS-CoV-2 and adenovirus may be pathogens potentially inducing post-infectious AIH by initiating self-perpetuating immune-mediated liver inflammation [9]. Interestingly, a previous report from an Israeli liver specialist has highlighted cases in which AIH appeared as a sequela of COVID-19 [54]. In those cases, hepatitis symptoms emerged approximately 3.5 months after the initial coronavirus infection, thus suggesting a potential link between COVID-19 and autoimmune hepatitis [54]. Hong et al., in their report of the case of a 54-year-old man infected with SARS-CoV-2 1 month before admission presented with abdominal pain and pruritus, have suggested that clinicians should be aware of COVID-19 as a trigger of severe AIH. After further evaluation, the laboratory results were consistent with the characteristics of AIH [55]. Notably, several previous case reports have suggested an association between AIH and COVID-19 vaccination rather than infection itself [56,57,58]. However, this observation is not applicable in this outbreak, because most cases have occurred in children not vaccinated against COVID-19 [20, 27].
3.4.4 Other Viruses, Toxins, and Environmental Exposures
Although no cases appeared to be epidemiologically related, and no associations have been found among exposure to pets, food, medication, toxins, or other environmental factors, all factors should be considered potential aetiologies requiring further investigation [6, 26].
3.5 Case Reports/Series in 2021–2023
In this section, we review original case reports and case series reporting cases occurring between 2021 and 2022. Only six case report/series studies were found. Table 1 summarizes the main findings of these included studies.
The six studies (Table 1) describe different cases of acute hepatitis of unknown origin in children and young adults. The studies were conducted in various countries, including Portugal, China, Japan, the Netherlands, and the United States [59,60,61,62,63,64]. The studies included both case reports and case series in 19 boys and girls 7 months to 10 years of age. Symptoms varied across studies but primarily comprised jaundice, abdominal pain, vomiting, diarrhoea, fever, lethargy, and anorexia. The duration of symptoms ranged from 4 days to 2 weeks. The studies used various diagnostic methods, including blood work, COVID-19 history, and hepatitis serologies. Elevated liver enzymes, including ALT > 56 U/L, AST > 40 U/L, and LDH > 170 U/L, were reported in all cases. Some cases also had elevated total bilirubin levels > 1.2 mg/dl [62,63,64]. The COVID-19 PCR test was negative on arrival at the hospital in most cases [59, 60, 62, 63], whereas two cases tested positive [59], one case experienced previously self-limiting COVID-19, and three cases had prior infection according to serological testing [61, 64]. No patient had positive hepatitis A–E serology, and one study detected the Torque Teno Virus [60, 64]. Complementary investigations, such as imaging and liver biopsy, were performed in all studies to help identify the cause of the acute hepatitis, and revealed a pattern of mild to severe liver inflammation and necrosis.
The treatment strategies varied with the cause and severity of the acute hepatitis. Some children were treated with only supportive care [59, 63], whereas others received antiviral medication, steroid pulse therapy, plasmapheresis, lipid-soluble vitamins, or reduced glutathione [60, 61, 63]. All children showed improvements in their symptoms and laboratory findings, and most fully recovered within 2 months. In six cases, urgent evaluation for liver transplantation was required, and the transplantations were successful and had good outcomes [62, 64]. All studies reported that the children ultimately fully recovered or had improved liver function after treatment.
4 Discussion
The purpose of this review was to provide a comprehensive overview of SAHUA, including documented cases, their distributions, symptoms and laboratory results, and possible hypotheses/aetiologies. Although several hypotheses exist regarding the aetiology of SAHUA in children, determining the origin or cause of this new strain that emerged in 2021 is challenging.
Our analysis, as detailed in Table 1, revealed a consistent pattern in which many cases tested positive for adenovirus in various specimen types (e.g., nasopharyngeal aspirate, blood, or stool samples), whereas none displayed positive staining for adenovirus on immunohistochemical analysis in liver biopsies [62, 63]. In agreement with this finding, Deep et al. have examined eight cases of children who developed acute liver failure, all of whom tested positive for adenovirus DNA in whole blood specimens [20]. Nevertheless, none of these children exhibited positive adenoviral staining in immunohistochemical analysis of liver biopsies [20]. A similar scenario has been observed in a cohort of paediatric acute hepatitis cases in Germany in 2022, wherein no clear evidence of linked adenovirus infection was documented [65]. These findings cast doubt on adenovirus as a definitive cause of SAHUA in children and underscore the need for further research to explore alternative contributing factors.
A notable point of consideration is the technical note issued by the Pan American Health Organization/WHO, suggesting that adenovirus might not be the primary cause of the outbreak but a coincidental finding [66]. In contrast, a compelling hypothesis has proposed AAV-2 as a likely etiologic agent for SAHUA in paediatric cases [31, 40, 41]. This hypothesis suggests that abnormal AAV-2 replication products, facilitated by HAdV and sometimes HHV-6B, may trigger immune-mediated hepatic disease in genetically and immunologically predisposed children [31, 32, 36, 38,39,40,41,42]. Furthermore, recent research has supported the pathogenesis of AAV-2 infections in SAHUA cases, characterized by low immunogenicity and broad tissue tropism [67]. Evidence has indicated that the liver injury observed in paediatric patients with AAV-2 infection is immune-mediated, as supported by observations of infiltrated activated T lymphocytes around AAV-2 infected hepatocytes and an increase in T-cell-response-associated cytokines [67]. Helper viruses, such as HAdV, human herpesvirus 6 (HHV-6), or Epstein-Barr virus, are often detected in cases of paediatric hepatitis with AAV-2 infection and are likely to enable AAV-2 replication. These findings imply that immune-mediated pathogenesis and genetic susceptibility play crucial roles in SAHUA [67]. The COVID-19 pandemic and disrupted exposure and immunity patterns may also contribute to disease severity and involve multiple viruses working together. Nevertheless, further investigation is necessary to understand the complex interactions among HAdV-F41, AAV-2, mutations, immune responses, and other factors.
In an investigation of the potential association between SARS-CoV-2 and SAHUA, Deep et al. have found that two of eight cases of acute hepatitis testing negative for SARS-CoV-2 by PCR involved prior SARS-CoV-2 infection, and six cases had SARS-CoV-2 IgG positivity [20]. Similarly, three reported cases of acute hepatitis of unknown aetiology in children in Portugal and Japan showed IgG spike protein positivity, whereas two had no known history of SARS-CoV-2 infection [59, 61]. These findings reflect those of Mahallawi et al., in a study in which 60% of acute hepatitis cases had no history of SARS-CoV-2 infection or vaccination, and tested positive for SARS-CoV-2 anti-S IgG antibody [68]. These findings suggest that these cases might have had a silent source of SARS-CoV-2, in agreement with the CDC’s finding that 68% of 78 confirmed SARS-CoV-2 positive paediatric cases presented with no symptoms of fever, cough, or shortness of breath and were reported to be asymptomatic [69]. Together, these findings support an important role of SARS-CoV-2 in the pathogenesis of severe hepatitis despite negative PCR tests in some cases. One possible explanation may be that those cases involved a previous asymptomatic SARS-CoV-2 infection that was neither detected at the time nor recalled by the patients themselves. Another explanation is that lockdowns during the COVID-19 pandemic might have disrupted normal patterns of exposure and immunity, thus making individuals more susceptible to viral coinfection [36].
Regarding laboratory tests and examinations, our review indicated that more than half of the patients requiring liver transplantation in the United Kingdom and the Netherlands had evidence of positive serology suggestive of prior SARS-CoV-2 infection, although most had negative PCR tests [20, 64]. In contrast, the reported cases in Alabama were tested for SARS-CoV-2 only through PCR but did not undergo additional serologic testing to rule out the role of SARS-CoV-2 in the pathogenesis of acute hepatitis in children, given that liver biopsies from these patients revealed no viral inclusions, no immunohistochemical evidence of adenovirus, and no viral particles identified by electron microscopy [63]. Therefore, these investigations underscore the importance of performing SARS-CoV-2 IgG tests rather than relying solely on PCR tests.
Notably, previous cases might have provided insufficient information regarding laboratory findings, because not all recommended/required examinations were performed. For instance, liver biopsy with additional analysis of specimens by electron microscopy or immunohistochemical staining was not performed on all reviewed cases of acute hepatitis in children [59, 63]. Additionally, cases were tested for adenovirus in differing specimen sources, including PCR of whole blood, plasma, stool, nasopharyngeal aspirates, or liver tissue, regardless of the accuracy and the sensitivity of the performed tests [59,60,61,62,63,64]. A previous report from the CDC has shown that PCR testing whole blood is more sensitive than PCR testing plasma or serum, and therefore is preferable for adenovirus detection [70]. This finding underscores the importance of performing accurate and highly sensitive diagnostic testing for adenovirus and other viral infections.
Regarding the management of severe acute hepatitis cases in children, supportive treatment has generally been provided to children who did not develop liver failure [59, 63], whereas liver transplantation is the most successful treatment for children with liver failure [62,63,64]. Other treatments have been proposed in the literature, on the basis of the likely aetiology of the outbreak, such as steroid treatments. Interestingly, in Japan, a case with negative chemistry panel findings for most known infectious agents responded to steroids after development of acute hepatitis [61]. Although the IgG spike protein peaked after steroid treatment [61], steroids can be inferred to be a suitable treatment, particularly for patients with immune infiltrates on liver biopsy. Such cases could benefit from immunosuppressive treatments such as steroids to prevent the deterioration of liver function or the need for liver transplantation.
Overall, clinical researchers and caregivers should consider whether any additional therapeutic modalities might slow disease progression. Recommended treatments for various potential causes are described below.
4.1 Management and Treatments
Because the definitive aetiology of current acute hepatitis outbreaks is not well established, treatment options are limited to modalities described in prior hepatitis literature. The existing literature has established that the treatment of hepatitis is mainly supportive and directed towards symptom management, including preventing severe complications, avoiding excessive protein consumption, and achieving adequate rest [12]. Patients in a hospital setting should be continually monitored, because they are likely to develop liver problems. If further complications, such as constipation, hypoproteinaemia, electrolyte imbalance, hypovolemia, hypoglycaemia, or gastrointestinal bleeding, develop, they should be managed as soon as possible [12].
The following treatment strategies have been suggested according to the hypothesized possible aetiologies:
4.1.1 Adenovirus
According to previous case reports, approximately 65% of adenovirus hepatitis cases occur in children [71], and a history of liver transplantation is the most common risk factor. Acute hepatitis in immunocompetent children is not a new phenomenon and has often been associated with adenovirus infection. A report in 2008 described the case of an immunocompetent 18-month-old child who developed acute liver failure presumably caused by adenovirus infection [72]. However, such cases are not limited to children; Khalifa et al. have reported acute hepatitis in immunocompetent adults testing positive for adenovirus [71]. Consequently, adenovirus infection should be considered a differential diagnosis in healthy children with acute hepatitis.
For patients testing positive for adenovirus, supportive management is required [12]. As noted by Campigotto A & Ng VL, most children in the United States tend to make a complete recovery with supportive treatment, although instances of liver transplantation have been documented [15]. Cidofovir is another treatment used to treat cases of acute hepatitis of unknown origin in children. Previous cases have been treated with cidofovir when the viral load of adenovirus was high [63]. However, in some cases, the treatment was not effective and did not decrease the viral load, thus eventually leading to liver failure and a need for transplantation [63]. Although previous studies support the use of cidofovir to treat the severe form of adenovirus infection, particularly in immunocompromised patients [73,74,75], randomized clinical trials remain necessary. Moreover, the efficacy of cidofovir in immunocompetent patients remains unknown, and thus more trials are warranted [73].
4.1.2 SARS-CoV-2
Another hypothesis suggests a potential role of SARS-CoV-2 as a possible aetiology. Importantly, the guidelines for managing SARS-CoV-2 infection in children published by several health institutes, such as the CDC, WHO, and NIH, agree that supportive management is the core treatment for SARS-CoV-2 infection [76,77,78]. To date, remdesivir, an antiviral drug that has been tested in clinical trials and has demonstrated efficacy in shortening recovery time in adults hospitalized with SARS-CoV-2 [79], is currently approved by the US Food and Drug Administration for the treatment of SARS-CoV-2 infection in adults and children 28 days old or older, regardless of hospitalization, and in patients with mild-to-moderate symptoms and complications [80]. However, its safety and effectiveness have not yet been formally evaluated in children [76]. Furthermore, a previous retrospective study in India has suggested that SARS-CoV-2-associated hepatitis may be part of MIS-C, a serious illness requiring hospitalization and aggressive multi-specialty management. In addition to the SARS-CoV-2 regimen, anti-inflammatory drugs, such as immunoglobulin and steroids, should be included in the treatment of patients also presenting with MIS-C [81].
4.1.3 Autoimmune Hepatitis
Alvarez et al. have emphasized the importance of considering the possibility of AIH even if circulating autoantibodies are negative, because 10% of children test positive for seronegative AIH [82]. This is significant because a delay in recognizing this condition could postpone treatment and elevate the risk of liver failure. Therefore, if the heightened immune response contributes to the disease's severity, it suggests the consideration of immunosuppressive treatment [10].
4.1.4 Other Viruses, Toxins, and Environmental Exposures
Liver transplantation is considered a last resort in patients with acute liver failure who do not respond to medical treatment or whose condition deteriorates rapidly. Nevertheless, no clear-cut, widely accepted criteria are available for liver transplantation in children with acute liver failure [12].
4.2 Prevention
Because of the absence of a confirmed aetiology, preventive measurements are limited to general infection prevention and control practices. According to the WHO, preventive measures should include frequent hand washing whenever possible with soap and water, or an alcohol (ethanol)-based hand sanitizer. Drinking clean water and practicing safe food handling and cooking methods are also crucial. Wearing a well-fitted mask that covers the mouth and nose, avoiding crowded places, and keeping a safe distance from others are all recommended precautions to decrease the transmission of the disease. Furthermore, in suspected or likely instances, health facilities should take routine measures, including contact and droplet precautions [26].
4.3 Learnings from Previous Case Reports, and Recommendations
-
1.
SAHUA in children is a challenging condition that requires close monitoring, because it can be caused by various unknown or novel pathogens, such as adenovirus or TTV. Because no specific treatment is currently available for these pathogens, supportive therapy remains the cornerstone of care. However, further research is needed to determine the most appropriate management strategies and to investigate the underlying disease mechanisms.
-
2.
Immunological dysfunction or activation may play major roles in SAHUA. In the case of SARS-CoV-2 infection, the virus may trigger autoimmune hepatitis-like conditions, which may require steroid therapy or other treatments to suppress the immune system. Further research is needed to determine the full extent of the effects of SARS-CoV-2 on immune system function.
-
3.
Potential links must be explored between various pathogens and the development of acute hepatitis in children. Some viruses may be relatively more prevalent in children, and their interaction with other viruses may increase the risk of developing the disease. Additionally, the lack of exposure to common pathogens during the COVID-19 pandemic might have contributed to an immunodeficiency-like state in children, thus increasing susceptibility to other viruses.
-
4.
Novel diagnostic tools such as metagenomic next-generation sequencing (NGS) and liver biopsy are essential to identify the underlying causes of SAHUA. These tools should be considered in the diagnostic work-up of children presenting with symptoms of acute hepatitis, particularly in cases in which viral hepatitis and autoimmune hepatitis have been ruled out.
-
5.
Further research is needed to fully understand the causes and mechanisms of SAHUA, particularly in cases with unknown origin. Additionally, the development of effective preventive and treatment strategies is crucial in decreasing the morbidity and mortality associated with this disease.
5 Conclusion
SAHUA in children poses a complex medical puzzle; 1% of cases result in mortality, and 6% of cases have a chance of progressing to life-threatening acute liver failure [83]. Our comprehensive review revealed inconsistencies in adenovirus detection and suggests that AAV-2 may be a potential culprit, and immune-mediated factors may be involved. SAHUA's connection to SARS-CoV-2 highlights the need for vigilance, because negative SARS-CoV-2 PCR tests may conceal prior infections. Consequently, SARS-CoV-2 has been suggested to affect host immunity and result in severe adenovirus infection. Therefore, further studies are needed to understand the relationship between prior SARS-CoV-2 infection and the severity of acute hepatitis potentially caused by adenovirus in children. Accurate diagnostics, supportive care, antiviral options, and immunosuppression strategies constitute the treatment landscape. Prevention currently relies on general infection control measures and heightened public health awareness. Early intervention, advanced diagnostic tools such as metagenomic NGS, and liver biopsy, international collaboration, and long-term patient follow-up are essential components for managing this condition. Overall, SAHUA remains a clinical enigma. Multidisciplinary collaboration, advanced diagnostics, international cooperation, and ongoing research are essential. The quest for effective prevention and treatment strategies continues, emphasizing adaptability in the face of emerging infectious challenges, to improve outcomes for affected children.
Data Availability
Not applicable.
Abbreviations
- AAA:
-
Anti-actin antibody
- AAV-2:
-
Adeno-associated virus-2
- AAV-A:
-
Adeno-associated dependoparvovirus A
- AIH:
-
Autoimmune hepatitis
- ALT:
-
Alanine aminotransferase
- AMA:
-
Anti-mitochondrial antibody
- ANA:
-
Antinuclear antibody
- ASMA:
-
Anti-smooth muscle antibody
- AST:
-
Aspartate aminotransferase
- CDC:
-
Centers for Disease Control and Prevention
- CMV:
-
Cytomegalovirus
- CT:
-
Threshold cycle
- CVVHDF:
-
Continuous venovenous haemodiafiltration
- DB:
-
Direct bilirubin
- EBER:
-
Epstein-Barr encoded RNA
- EBNA:
-
Epstein-Barr nuclear antigen
- EBV:
-
Epstein-Barr virus
- ECDC:
-
European Centre for Disease Prevention and Control
- GGT:
-
Gamma-glutamyl transferase
- HAdV-F41:
-
Human adenovirus type 41
- HAV:
-
Hepatitis A virus
- HBcAg:
-
Hepatitis B core antigen
- HBsAg:
-
Hepatitis B surface antigen
- HBV:
-
Hepatitis B virus
- HCV:
-
Hepatitis C virus
- HDV:
-
Hepatitis D virus
- HEV:
-
Hepatitis E virus
- HSV:
-
Herpes simplex virus
- IgG:
-
Immunoglobulin G (for SARS-CoV-2)
- INR:
-
International normalized ratio
- LDH:
-
Lactate dehydrogenase
- MIS-C:
-
Multisystem inflammatory syndrome in children
- NGS:
-
Next-generation sequencing (metagenomic)
- PCR:
-
Polymerase chain reaction
- SARS‐CoV:
-
Severe acute respiratory syndrome coronavirus
- TB:
-
Total bilirubin
- TTV:
-
Transfusion transmitted virus
- UKHSA:
-
United Kingdom Health Security Agency
- VCA:
-
Viral capsid antigen
- WHO:
-
World Health Organization
References
World Health Organization. Hepatitis. 2022: https://www.who.int/health-topics/hepatitis#tab=tab_1. Cited 11 Aug 2022.
World Health Organization. Hepatitis 2019; https://www.who.int/news-room/questions-and-answers/item/hepatitis. Cited 11 Aug 2022
World Health Organization. Multi-Country—acute, severe hepatitis of unknown origin in children. 2022. https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON376. Cited 11 Aug 2022.
Baker JM, Buchfellner M, Britt W, Sanchez V, Potter JL, Ingram LA, et al. Acute hepatitis and adenovirus infection among children—Alabama, October 2021–February 2022. MMWR Morb Mortal Wkly Rep. 2022;71(18):638–40.
Marsh K, Tayler R, Pollock L, Roy K, Lakha F, Ho A, et al. Investigation into cases of hepatitis of unknown aetiology among young children, Scotland, 1 January 2022 to 12 April 2022. Euro Surveill. 2022;27(15):2200318.
Centers for Disease Control and Prevention. Technical Report: Acute Hepatitis of Unknown Cause | CDC. 2022. https://www.cdc.gov/ncird/investigation/hepatitis-unknown-cause/technical-report.html. Cited 10 Aug 2022.
World Health Organization. Severe acute hepatitis of unknown aetiology in children—multi-country. 2022. https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON400. Cited 11 Aug 2022.
Gong K, Xu X, Yao J, Ye S, Yu X, Tu H, et al. Acute hepatitis of unknown origin in children: A combination of factors. Front Pharmacol. 2022;13:1056385.
Mendez-Sanchez N, Pal SC. Editorial: Acute hepatitis of unknown origin in children. Is autoimmunity at play? Med Sci Monit. 2022;28:e937371–4.
Gao S, Gong M, Song H. Acute severe hepatitis of unknown origin in children: considerations from the perspective of immunology. World J Pediatr. 2022;18(8):529–32.
Sallam M, Mahafzah A, Şahin GÖ. Hepatitis of unknown origin and etiology (acute non hepa-e hepatitis) among children in 2021/2022: review of the current findings. Healthcare. 2022;10(6):10060973.
Chen Y, Lou J, Yang Z, Chen Q, Hua C, Ye S, et al. Diagnosis, treatment, and prevention of severe acute hepatitis of unknown etiology in children. World J Pediatr WJP. 2022;18(8):538–44.
UK Health Security Agency. Investigation into acute hepatitis of unknown aetiology in children in England Technical briefing 3. 2022; https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1077027/acute-hepatitis-technical-briefing_3.pdf. Cited 6 Jun 2022.
Peters AL, Kim S, Mourya R, Asai A, Taylor A, Rogers M, et al. Recent increase in incidence of severe acute hepatitis of unknown etiology in children is associated with infection with adenovirus and other nonhepatotropic viruses. J Pediatr. 2023;259:113439.
Campigotto A, Ng VL. Severe acute hepatitis of unknown cause in children. CMAJ. 2022;194(31):E1089.
van Beek J, Fraaij PL, Giaquinto C, Shingadia D, Horby P, Indolfi G, et al. Case numbers of acute hepatitis of unknown aetiology among children in 24 countries up to 18 April 2022 compared to the previous 5 years. Euro Surveill. 2022;27(19):2200370.
Kambhampati AK. Trends in acute hepatitis of unspecified etiology and adenovirus stool testing results in children—United States, 2017–2022. MMWR Morb Mort Wkly Rep. 2022;71:797–802.
Şahin GÖ, Mondelli MU, Matičič M, Sandulescu O, Irving W. Acute severe hepatitis of unknown aetiology in children: a new non-A–E hepatitis virus on horizon? Clin Microbiol Infect. 2022;28(9):1300–1.
Frediansyah A, Sallam M, Yufika A, Sharun K, Iqhrammullah M, Chandran D, et al. Acute Severe Hepatitis of Unknown Etiology in Children: A Mini-Review. Narra J 2022;05–27.
Deep A, Grammatikopoulos T, Heaton N, Verma A, Dhawan A. Outbreak of hepatitis in children: clinical course of children with acute liver failure admitted to the intensive care unit. Intensive Care Med. 2022;48(7):958–62.
Mücke MM, Zeuzem S. The recent outbreak of acute severe hepatitis in children of unknown origin—what is known so far. J Hepatol. 2022;77(1):237–42.
Khader S, Foster I, Dagens A, Norton A, Sigfrid L. Severe acute hepatitis of unknown aetiology in children—what is known? BMC Med. 2022;20(1):1–9.
Brodin P, Arditi M. Severe acute hepatitis in children: investigate SARS-CoV-2 superantigens. Lancet Gastroenterol Hepatol. 2022;7(7):594–5.
Centers for Disease Control and Prevention. Overview: children with hepatitis of unknown cause | CDC. 2022https://www.cdc.gov/ncird/investigation/hepatitis-unknown-cause/overview-what-to-know.html. Cited 18 Aug 2022.
ECDC, WHO. Joint ECDC-WHO Regional Office for Europe Hepatitis of Unknown Origin in Children Surveillance Bulletin. 2022. https://cdn.ecdc.europa.eu/novhep-surveillance/. Cited 10 Nov 2022.
Acute hepatitis of unknown aetiology in children—multi-country. 2022; https://www.who.int/emergencies/disease-outbreak-news/item/DON-389.
Centers for Disease Control and Prevention. Recommendations for Adenovirus Testing and Reporting of Children with Acute Hepatitis of Unknown Etiology. 2022; https://emergency.cdc.gov/han/2022/han00462.asp. Cited 10 Aug 2022.
Vidal AR, Vaughan A, Innocenti F, Colombe S, Nerlander L, Rachwal N, et al. Hepatitis of unknown aetiology in children–epidemiological overview of cases reported in Europe, 1 January to 16 June 2022. Eurosurveillance. 2022;27(31):2200483.
CDC Alerts Providers to Hepatitis Cases of Unknown Origin. 2016. https://www.cdc.gov/media/releases/2022/s0421-hepatitis-alert.html. Cited 10 Aug 2022.
Liang J, Kelly DR, Pai A, Gillis LA, Sanchez LHG, Shiau HH, et al. Clinicopathologic features of severe acute hepatitis associated with adenovirus infection in children. Am J Surg Pathol. 2023;10:1097.
Grand RJ. Pathogenicity and virulence of human adenovirus F41: possible links to severe hepatitis in children. Virulence. 2023;14(1):2242544.
Martin NA, Gonzalez G, Reynolds LJ, Bennett C, Campbell C, Nolan TM, et al. Adeno-associated virus 2 and human adenovirus F41 in wastewater during outbreak of severe acute hepatitis in children, Ireland. Emerg Infect Dis. 2023;29(4):751.
Namakin K, Naserghandi A, Allameh SF. Severe acute hepatitis of unknown etiology in children in 2022: a narrative review. New Microb New Infect. 2023;51: 101087.
Hakim MS. The recent outbreak of acute and severe hepatitis of unknown etiology in children: a possible role of human adenovirus infection? J Med Virol. 2022;94:4065–8.
Elsheikh R, Tien HT, Makram AM, Van NT, Le TTB, Vasanthakumaran T, et al. Acute hepatitis of unknown origin in children: Behind the statistics. Hepatology. 2022;77:2118–27.
Matthews PC, Campbell C, Săndulescu O, Matičič M, Ruta SM, Rivero-Juárez A, et al. Acute severe hepatitis outbreak in children: a perfect storm. What do we know, and what questions remain? Front Pharmacol. 2022;13:1062408.
Uwishema O, Mahmoud A, Wellington J, Mohammed SM, Yadav T, Derbieh M, et al. A review on acute, severe hepatitis of unknown origin in children: A call for concern. Ann Med Surg. 2022;81: 104457.
Pan L, Wang G, Zhong J, Fan X. Current knowledge about the outbreak of acute severe hepatitis of unknown origin among children. J Clin Transl Res. 2022;8(6):470.
Alexander EC, Deep A. Characterization of a hepatitis outbreak in children, 2021 to 2022. JAMA Netw Open. 2022;5(10): e2237091.
Mitchell MM, Leng Y, Boppana S, Britt WJ, Gutierrez Sanchez LH, Elledge SJ. Signatures of AAV-2 immunity are enriched in children with severe acute hepatitis of unknown etiology. Sci Transl Med. 2023;15(706): eadh9917.
Ho A, Orton R, Tayler R, Asamaphan P, Herder V, Davis C, et al. Adeno-associated virus 2 infection in children with non-A–E hepatitis. Nature. 2023;617(7961):555–63.
Morfopoulou S, Buddle S, Torres Montaguth OE, Atkinson L, Guerra-Assunção JA, Moradi Marjaneh M, et al. Genomic investigations of unexplained acute hepatitis in children. Nature. 2023;617(7961):564–73.
Reyne MI, Allen DM, Levickas A, Allingham P, Lock J, Fitzgerald A, et al. Detection of human adenovirus F41 in wastewater and its relationship to clinical cases of acute hepatitis of unknown aetiology. Sci Total Environ. 2023;857: 159579.
Servellita V, Sotomayor Gonzalez A, Lamson DM, Foresythe A, Huh HJ, Bazinet AL, et al. Adeno-associated virus type 2 in US children with acute severe hepatitis. Nature. 2023;617(7961):574–80.
Li J, Hu X, Yan X, Wu C, Nan Y. Clinical characteristics and possible etiology in children with acute severe hepatitis of unknown etiology. Chin Med J. 2022;135(24):3019–21.
Sun J, Aghemo A, Forner A, Valenti L. COVID-19 and liver disease. Liver Int. 2020;40(6):1278–81.
Pérez-Gracia MT, Tarín-Pelló A, Suay-García B. Severe acute hepatitis of unknown origin in children: what do we know today? J Clin Transl Hepatol. 2022;10(4):711.
Rawat SK, Asati AA, Jain A, Mishra N, Ratho RK. COVID-19 associated hepatitis in children (CAH-C) during the second wave of SARS-CoV-2 infections in Central India: is it a complication or transient phenomenon? Brit Med J 2021.
Lal BB, Sood V, Gupta E, Agarwal R, Khanna R, Alam S. Severe acute hepatitis of unknown etiology presenting as pediatric acute liver failure: analysis of likely etiology, clinical course and outcome. J Clin Exp Hepatol. 2023;13:912–6.
Brisca G, Mallamaci M, Tardini G, Martino L, Chianucci B, Ricci M, et al. SARS-CoV-2 infection may present as acute hepatitis in children. Pediatr Infect Dis J. 2021;40(5): e214.
Funaki T, Yamada M, Ide K, Ito R, Shoji K, Ogimi C, et al. Etiology of severe acute hepatitis in a pediatric transplant center in Japan. J Pediatr Infect Dis Soc. 2023;12(4):248–51.
Nishiura H, Jung S, Hayashi K. High population burden of Omicron variant (B. 1.1. 529) is associated with the emergence of severe hepatitis of unknown etiology in children. Int J Infect Dis. 2022;122:30–2.
Mieli-Vergani G, Vergani D, Czaja AJ, Manns MP, Krawitt EL, Vierling JM, et al. Autoimmune hepatitis. Nat Rev Dis Prim. 2018;4:18017.
Zhang L, Huang L, Yue Y, Fawaz R, Lim JK, Fan J. Acute hepatitis of unknown origin in children: early observations from the 2022 outbreak. J Clin Transl Hepatol. 2022;10(3):522.
Hong JK, Chopra S, Kahn JA, Kim B, Khemichian S. Autoimmune hepatitis triggered by COVID-19. Intern Med J. 2021;51(7):1182–3.
Camacho-Domínguez L, Rodríguez Y, Polo F, Restrepo-Gutierrez JC, Zapata E, Rojas M, et al. COVID-19 vaccine and autoimmunity. A new case of autoimmune hepatitis and review of the literature. J Transl Autoimmun. 2022;5:100140.
Tan CK, Wong YJ, Wang LM, Ang TL, Kumar R. Autoimmune hepatitis following COVID-19 vaccination: true causality or mere association? J Hepatol. 2021;75(5):1250–2.
Garrido I, Lopes S, Simões MS, Liberal R, Lopes J, Carneiro F, et al. Autoimmune hepatitis after COVID-19 vaccine—more than a coincidence. J Autoimmun. 2021;125:102741.
Costa RC, Esteves CS, Flores P, Varandas L. Acute hepatitis of unknown origin in children: two cases in a Portuguese hospital. Acta Med Port. 2023. https://doi.org/10.20344/amp.18690.
Zhou Y, Gu H, Tang Q, Li F, Zhu J, Ai T, et al. Case report: A case of severe acute hepatitis of unknown origin. Front Pediatr. 2022;10: 975628.
Morita A, Imagawa K, Asayama K, Terakado T, Takahashi S, Yaita K, et al. Immunological characteristics of severe acute hepatitis of unknown origin in a child post SARS-CoV-2 infection. Clin Immunol. 2022;245: 109138.
Boster JM, Dominguez SR, Messacar K, Adams M, Weinberg A, Black JO, et al. Acute liver failure in a child with adenovirus detected by PCR in the explanted liver. Pediatrics. 2023;151(2): 059237.
Gutierrez Sanchez LH, Shiau H, Baker JM, Saaybi S, Buchfellner M, Britt W, et al. A case series of children with acute hepatitis and human adenovirus infection. N Engl J Med. 2022;387(7):620–30.
Lexmond WS, de Meijer VE, Scheenstra R, Bontemps ST, Duiker EW, Schölvinck EH, et al. Indeterminate pediatric acute liver failure: clinical characteristics of a temporal cluster of five children in the Netherlands in the spring of 2022. United Eur Gastroenterol J. 2022;10(8):795–804.
Leiskau C, Tsaka S, Meyer-Ruhnke L, Mutschler FE, Pfister E, Lainka E, et al. Acute severe non-AE-hepatitis of unknown origin in children—a 30-year retrospective observational study from north-west Germany. J Hepatol. 2023;78(5):971–8.
Gao Y, Wang L, Wang L, Lu F. Severe acute hepatitis in children with unknown aetiology, etiology analysis and the next action. Virologica Sinica. 2022;37(5):778.
Zheng L, Wang L, Lu F. Looking back on the outbreak of acute severe hepatitis with unknown etiology in children in 2022: what do we know now and where do we go from here? J Med Virol. 2023;95(6): e28890.
Mahallawi WH, Ibrahim NA, Aljohani AS, Shaikh EA, Nafe RH, Khan AM, et al. Assessment of SARS-CoV-2 anti-spike IgG antibody in women and children in Madinah, Saudi Arabia: a single-center study. Int J Environ Res Public Health. 2021;18(19):9971.
Centers for Disease Control and Prevention. Coronavirus Disease 2019 in Children—United States. 2020. https://www.cdc.gov/mmwr/volumes/69/wr/mm6914e4.htm. Cited 11 Feb 2023.
National Center for Immunization and Respiratory Diseases, (NCIRD). Laboratory Testing Guidance For Pediatric Patients with Acute Hepatitis. 2022: https://www.cdc.gov/ncird/investigation/hepatitis-unknown-cause/laboratories-testing-typing.html#:~:text=Nucleic%20acid%20amplification%20testing%20(NAAT,by%20PCR%20and%20is%20preferred. Cited 10 Jan 2023.
Khalifa A, Andreias L, Velpari S. Adenovirus hepatitis in immunocompetent adults. J Investig Med High Impact Case Rep. 2022;10:23247096221079190.
Canan O, Ozçay F, Bilezikçi B. Adenovirus infection as possible cause of acute liver failure in a healthy child: a case report. Turk J Gastroenterol. 2008;19(4):281–3.
Lynch JP, Fishbein M, Echavarria M. Adenovirus. Semin Respir Crit Care Med. 2011;32(4):494–511.
Alcamo AM, Wolf MS, Alessi LJ, Chong HJ, Green M, Williams JV, et al. Successful use of cidofovir in an immunocompetent child with severe adenoviral sepsis. Pediatrics. 2020;145(1): e20191632.
Verma A, Vimalesvaran S, Lampejo T, Deep A, Dhawan A. Use of cidofovir in recent outbreak of adenovirus-associated acute liver failure in children. Lancet Gastroenterol Hepatol. 2022;7(8):700–2.
Centers for Disease Control and Prevention. Information for pediatric healthcare providers. 2020: https://www.cdc.gov/coronavirus/2019-ncov/hcp/pediatric-hcp.html.
World Health Organization. COVID-19 disease in children and adolescents: scientific brief, 29 Sep 2021.
National Institutes of Health. General management of nonhospitalized patients with acute COVID-19 . 2021: https://www.covid19treatmentguidelines.nih.gov/management/clinical-management/nonhospitalized-patients--general-management/. Cited 18 Aug 2022.
Beigel JH, Tomashek KM, Dodd LE, Mehta AK, Zingman BS, Kalil AC, et al. Remdesivir for the treatment of COVID-19—preliminary report. N Engl J Med. 2020;383(19):1813–36.
U.S. Food and Drug Administration. Coronavirus (COVID-19) | Drugs . 2022; [cited December 5, 2022]. Available from: https://www.fda.gov/drugs/emergency-preparedness-drugs/coronavirus-covid-19-drugs. Cited 5 Dec 2022.
Son MBF, Friedman K. COVID-19: multisystem inflammatory syndrome in children (MIS-C) management and outcome 2022.
Alvarez F. Autoimmune hepatitis in children. Jornal de Pediatria. 2019;95(4):382–4.
Zhaori G. Severe acute hepatitis of unknown causes in children–current findings, questions, opinions, and recommendations, a mini-review. Pediatr Investig. 2022;6(3):211–8.
Funding
There was no funding for this review.
Author information
Authors and Affiliations
Contributions
MA, BAA, and ZAB conceived the review and developed the study design; MA, BAA, HS, and TA performed the screening and/or data extraction; MA, BAA, HS, AE, and TA analysed and interpreted the data; ZAB supervised the review process; MA, BAA, HS, AE, TA, and CM drafted the manuscript. All authors read and critically revised the manuscript, and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
No potential conflicts of interest are reported by the authors.
Ethical Approval and Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
AlShurman, M., AlShurman, B.A., Sehar, H. et al. Uncovering the Underlying Causes of Severe Acute Hepatitis of Unknown Aetiology in Children: A Comprehensive Review. Dr. Sulaiman Al Habib Med J 5, 101–117 (2023). https://doi.org/10.1007/s44229-023-00043-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44229-023-00043-0