Abstract
Background
Antibiotic de-escalation (ADE) is a stewardship initiative that aims to reduce exposure to antimicrobials, thus limiting their unwanted effect, including antimicrobial resistance. Our study aims to describe the impact of ADE compared with the continuation of therapy on the outcome of critically ill coronavirus disease 2019 (COVID-19) patients.
Material and Methods
A single-center retrospective study included critically ill COVID-19 adult patients admitted between January 1, 2019 and August 31, 2021, and started on broad-spectrum antibiotics. The primary outcome was intensive care unit (ICU) mortality. In addition, other clinical outcomes were evaluated, including ICU readmissions, length of stay, and superinfection.
Results
The study included 73 patients with a mean age of 61.0 ± 19.4, and ADE was performed in 10 (13.6%) of these. In the ADE group, 8/10 (80%) cultures were positive. ICU mortality was not statistically different between ADE and continuation of therapy groups (60 vs. 41.3%, respectively, P = 0.317). Superinfection occurred in 4 (5.4%) patients. Hospital mortality, length of stay, and ICU readmission rates did not differ significantly between groups.
Conclusion
De-escalation of broad-spectrum antibiotics in critically ill covid-19 patients was not associated with higher mortality. A larger cohort is needed to confirm these findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
By the end of January 2022, the pandemic caused by severe acute respiratory syndrome coronavirus (SARS-CoV-2) had exceeded 38 million cumulative confirmed cases and more than 5.5 million cumulative deaths worldwide [1]. The Survival Sepsis Campaign (SSC) published guidelines for the treatment and management of coronavirus disease 2019 (COVID-19) [2]. However, this guideline did not include any recommendations for diagnosing and managing COVID-19 bacterial co-infections [2]. On the other hand, the Infectious Diseases Society of America (IDSA) guidelines highlighted the overuse of antibiotics (AB) in early COVID-19 with a low overall rate of reported co-infection [3]. Data on the rate of secondary bacterial infections in patients with COVID-19 are limited [4]. A meta-analysis aimed to determine the prevalence of confirmed bacterial infections among patients with COVID-19 found that only 3.5% of cases had bacterial co-infection, and 14.3% had secondary bacterial infections [5,6,7,8,9]. Another recent meta-analysis analyzing 31 studies found that the estimated bacterial co-infection was 8.6% (95% CI 4.7–15.2%) [9].
Antibiotic de-escalation (ADE) is a stewardship initiative that aims to reduce exposure to antimicrobials, thus limiting their unwanted effect, including antimicrobial resistance [10]. Many guidelines advocate the daily assessment of de-escalation among septic patients [11, 12]. The international guidelines for sepsis and septic shock suggest daily assessment for the de-escalation of antimicrobials as a weak recommendation based on the very low-quality evidence [2]. A meta-analysis of 12 observational studies and one randomized study showed lower mortality in the ADE arm than control (RR 0.72; 95% CI 0.57–0.91) [9]. However, these results should be interpreted with caution as patients enrolled in the ADE arm were less sick and did not have multidrug-resistant pathogens [9]. A recent study in Greece described lower mortality of patients in the ADE arm than controls despite the high rate of multidrug-resistant pathogens in cultures [13].
During the COVID-19 pandemic, several studies identified an increase in the rate of antibiotic utilization [8, 14, 15]. As a result, many initiatives proposed limiting antibiotics in COVID-19 patients [16, 17]. Notably, the National Institute of Health (NIH) guidelines recommend against antibacterial therapy in moderate to severe COVID-19 unless clinical evidence of infection or secondary infection is suspected [12]. However, data on the ADE of antimicrobials in COVID-19 patients in a critical care setting is limited. Therefore, our study aims to compare the outcome of de-escalation versus the continuation of broad-spectrum antimicrobials in critically ill COVID-19 patients in the setting of a high rate of multidrug-resistant pathogens.
2 Materials and Methods
A retrospective study was conducted at King Faisal Specialist Hospital and Research Center-Jeddah (KFSHRC-J), a tertiary care and referral hospital, between January 1, 2019 and August 31, 2021. The hospital institutional review board approved the study (IRB# 2021-65). The study included all COVID-19 patients 18 years or older who required intensive care unit (ICU) admission. Only patients started on the broadest spectrum of antipseudomonal beta-lactams, including carbapenem or ceftazidime-avibactam, were included. Ceftolozane-tazobactam was unavailable at the hospital during the data collection period. The study excluded those who received broad-spectrum antibiotics for less than 48 h, were ICU discharged or died within 48 h of ICU admission. We collected patients' data, including demographics, COVID-19 status, antibiotics used, cultures, baseline labs, and infection sources through the RedCap system. We divided patients according to the broad-spectrum antibiotic course into continuation or ADE therapy groups.
2.1 Study Outcomes
The primary outcome was ICU mortality. Secondary outcomes included superinfection, ICU and hospital length of stay, ICU readmission rate, and hospital mortality.
2.2 Definitions
We defined broad-spectrum antibiotics as antimicrobial therapy covering all relevant pathogens that potentially cause the infectious episode [18]. We considered antipseudomonal carbapenem or ceftazidime-avibactam as our targeted prescribed broad-spectrum antibiotic. We based our broad-spectrum antibiotics choice on the hospital antibiogram, which has a high rate of extended-spectrum antibiotics and multidrug resistance. We defined ADE as replacing a broad-spectrum antibiotic with a narrow spectrum or lower ecological Impact [19, 20]. We considered antibiotics re-escalation as the resumption of a broad-spectrum treatment justified by a clinical worsening, not necessarily related to the initial infection [21]. We defined superinfection as the occurrence of infection with pathogen identification with the need to introduce a new antimicrobial treatment. Finally, we described infection recurrence as the reappearance of an infection after the cessation of all antibiotic therapy [21].
2.3 Statistical Analysis
Data were presented as frequencies and percentages for categorical data and mean ± standard deviation (SD) for continuous data. As appropriate, chi-square or Fisher exact tests were used to test significant differences in categorical variables. We used student t tests or Mann–Whitney tests to test significant differences in continuous variables. All P values were two-tailed. P < 0.05 was considered significant. We used SPSS (Version 25.0. Armonk, NY: IBM Corp) for all statistical analyses.
3 Results
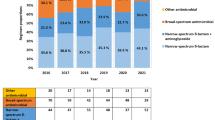
One hundred and nineteen critically ill patients with COVID-19 were screened, and 73 fitted the inclusion criteria. The mean ± SD age was 61.0 ± 19.4 years, with 31 (42.5%) male patients. Most patients, 60 (95.2%), were admitted to the medical ICU. The mean ± SD acute physiology and chronic health evaluation III (APACHE III) score were 19.0 ± 9.9, while the mean ± SD of sequential organ failure assessment (SOFA) score was 10.0 ± 6.7. Mechanical ventilation was used in 51 (69.9%) patients during ICU stay, for a mean ± SD of 20.1 ± 20.5 ventilation days (Table 1). Sixty-three (86.3%) patients completed their therapy without ADE. Among the ten patients in the ADE group (13.6%), four (5.5%) required re-escalation of treatment (Fig. 1). The clinical details of those patients can be found in the supplementary material (Table S1).
Primary and secondary outcomes are summarized in Table 2. There was no statistically significant difference in the primary outcome, ICU mortality, between patients who continued antimicrobial therapy and those in the ADE group. ICU mortality occurred in 32 (43.8%) patients (Table 2). We found similar findings in all secondary outcomes (Table 2). Superinfection was found in 4 (5.4%) patients. Microorganisms found among superinfection patients are listed in Supplementary Table S2. Hospital mortality was observed in 33 (45.2%) patients. The mean ± SD length of ICU stay was 24.8 ± 20.7 days, while the mean ± SD length of hospital stay was 29.7 ± 22.9 days. Six (14.6%) patients had an event of ICU readmission within 30 days of ICU discharge. Recurrence of infection three months after antibiotic therapy was detected in 8 (32.0%) patients.
Patients who continued on antibiotic therapy had a statistically significant longer duration of antibiotic use, with a mean ± SD of 9.4 ± 4.4 days in comparison to patients in the de-escalation group mean ± SD of 5.7 ± 3.1; P = 0.004 (Table 3). Meropenem was the most used antibiotic among 66 (90.4%) patients. Concurrent antibiotic use was found in ten (13.7%) patients, mainly fluoroquinolones 5 (6.8%) and aminoglycosides 4 (5.5%). The culture was positive in 35 (47.9%) of our patients. The most commonly reported microorganism was Pseudomonas aeruginosa in 7 (9.6%) cultures. The most seen resistance patterns were extended-spectrum beta-lactamase- and carbapenem-resistant Pseudomonas among 5 (14.3%) and 2 (5.7%) cultures, respectively (Table 4).
4 Discussion
In our cohort of critically ill COVID-19 patients, only 10 (13.6%) patients underwent de-escalation, which is considered low compared with previously published studies [19, 22]. Microbiological confirmation was documented in 80 and 42.9% of patients in the ADE and continuation groups. Among the sixty-three patients whose antibiotics were continued without ADE, 27 (42.9%) had positive cultures. Sixteen of 27 had a susceptible gram-negative organism to the primary broad-spectrum antibiotic. Seven of these 16 cases (43.7%) had documented resistance requiring therapy continuation. A possible explanation for our cohort's low ADE percentage might be related to our hospital antibiogram. The high rate of multidrug resistance and extended-spectrum antibiotics might render prescribers to the de-escalation decision. Another reason might be the limited data on COVID-19 bacterial co-infection and the infection complication at the beginning of the pandemic [3, 23]. Optimization of diagnostic criteria might provide more objective guidance for ADE. [7] A recent Italian study that tested multiplex PCR assay on critically ill COVID-19 patients to aid in diagnosing pneumonia found that around 39 of 44 (88.6%) patients with positive samples had their antibiotic escalated or de-escalated [24].
In our study, superinfection was found only among patients who continued the therapy and accounted for 6.3% within this group. The overall superinfection rate in our study was relatively lower than in the previous study [22]. Previous studies of non-covid-19 patients detected more Superinfections in the streamlining group (27% in ADE versus 11% in non-ADE, P = 0.03) [10, 22, 25]. Superinfection in our study included two Stenotrophomonas maltophilia and two Aspergillus species. On the other hand, a recent retrospective study found that 43/989 (4.3%) COVID-19 patients had superinfection with Pseudomonas aeruginosa and Escherichia coli as the most isolated organisms [6].
There were no statistically significant differences in either ICU mortality (60 vs. 41.3%, P = 0.317) or hospital mortality (70 vs. 41.3%, P = 0.169) between ADE and continuation of the therapy groups, respectively. Indeed, higher APACHE III scores were found in the de-escalation group, 25.3 ± 10.3, compared to 17.9 ± 9.5 in the continuation group (P = 0.049). In many previously published studies, mortality was not different among non-COVID-19 patients whose antibiotics de-escalated or continued. However, a minority of the cases were severe or required ICU stay [22, 26]. In a systematic review and meta-analysis of 14 stewardship objectives, the relative risk reduction for mortality in the de-escalation group was 66% (RR 0·44, 95% CI 0.30–0.66, P < 0.0001) [27].
A randomized controlled study conducted on 120 septic patients found a trend for longer ICU length of stay with 9 [interquartile range (IQR) 5–22] days in the de-escalation group compared to 8 [IQR 4–15] days in the continuation group (P = 0.71). The mortality rate was similar between groups [22]. A position statement from a task force of the European Society of Intensive Care Medicine (ESICM) gave a moderate recommendation with low-quality evidence to consider both risks of death and difficulty in treating pathogens in the decision to de-escalating antibiotic therapy [28]. The main limitation of this study is the small sample size; we only had ten patients in the ADE group. Another limitation is restricting the definition of ADE to include a narrow spectrum of antibiotics only rather than having the early discontinuation or discontinuation of the combination therapy, including aminoglycosides or fluoroquinolones. Moreover, this cohort had no data on inflammatory marker levels or other radiological diagnostics.
5 Conclusions
During the era of COVID-19, broad-spectrum antibiotics were only de-escalated in a small percentage of high disease severity score patients and microbiological confirmation. Broad-spectrum ADE in critically ill COVID-19 patients was not associated with higher mortality. The continual use of broad-spectrum antibiotics on COVID-19 patients leads to more superinfection cases in our hospital. A larger cohort is needed to confirm these findings.
Availability of Data and Material
Any requested data will be available in a timely manner.
Abbreviations
- ADE:
-
Antibiotic de-escalation
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus
- IDSA:
-
Infectious Diseases Society of America
- SSC:
-
Surviving sepsis campaign
- NIH:
-
National Institute of Health
- KFSHRC-J:
-
King Faisal Specialist Hospital and Research Center-Jeddah
- APACHE III:
-
Acute physiology and chronic health evaluation III
- SOFA:
-
Sequential organ failure assessment
- ICU:
-
Intensive care unit
- COVID-19:
-
Coronavirus disease-19
References
Who coronavirus (COVID-19) dashboard. No Title. Retrieved January 9, 2022. https://covid19.who.int/HealthOrganization. From https://covid19.who.int/.
Alhazzani W, Evans L, Alshamsi F, Møller MH, Ostermann M, Prescott HC, et al. Surviving sepsis campaign guidelines on the management of adults with Coronavirus disease 2019 (COVID-19) in the ICU: first update. Crit Care Med. 2021;2019:E219–34.
Cheng VC chung, Edwards KM, Gandhi R, Gallagher J. Last updated January 8, 2021 and posted online at http://www.idsociety.org/COVID19guidelines. Please check website for a most updated version of these guidelines. 2021;0–137.
Baiou A, Elbuzidi AA, Bakdach D, Zaqout A, Alarbi KM, Bintaher AA, et al. Clinical characteristics and risk factors for the isolation of multi-drug-resistant Gram-negative bacteria from critically ill patients with COVID-19. J Hosp Infect. 2021;1(110):165–71.
Langford BJ, So M, Raybardhan S, Leung V, Westwood D, MacFadden DR, et al. Bacterial co-infection and secondary infection in patients with COVID-19: a living rapid review and meta-analysis. Clin Microbiol Infect. 2020;26:1622–9. https://doi.org/10.1016/j.cmi.2020.07.016.
Garcia-Vidal C, Sanjuan G, Moreno-García E, Puerta-Alcalde P, et al. Incidence of co-infections and superinfections in hospitalized patients with COVID-19—a retrospective cohort study. Clin Microbiol Infect. 2021;27(1):83–8.
Maataoui N, Chemali L, Patrier J, et al. Impact of rapid multiplex PCR on management of antibiotic therapy in COVID-19-positive patients hospitalized in intensive care unit. Eur J Clin Microbiol Infect Dis. 2021;40(10):2227–34.
Langford BJ, So M, Raybardhan S, Leung V, Westwood D, MacFadden DR, et al. Bacterial co-infection and secondary infection in patients with COVID-19: a living rapid review and meta-analysis. Vol. 26, clinical microbiology and infection. Amsterdam: Elsevier BV; 2020. p. 1622–9.
Langford BJ, So M, Raybardhan S, et al. antibiotic prescribing in patients with COVID-19—rapid review and meta-analysis. Clin Microbiol Infect. 2021;27(4):520–31.
Lakbar I, De Waele JJ, Tabah A, Einav S, Martin-Loeches I, Leone M. Antimicrobial de-escalation in the ICU: from recommendations to level of evidence. Adv Ther. 2020;37(7):3083–96.
Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021;47(11):1181–247.
National Institutes of Health. Treatment guidelines panel. Coronavirus disease 2019 (COVID-19). Nih. 2021;2019:1–243.
Routsi C, Gkoufa A, Arvaniti K, Kokkoris S, Tourtoglou A, Theodorou V, et al. De-escalation of antimicrobial therapy in ICU settings with high prevalence of multidrug-resistant bacteria: a multicentre prospective observational cohort study in patients with sepsis or septic shock. J Antimicrob Chemother. 2020;75(12):3665–74.
Pettit NN, Nguyen CT, Lew AK, Bhagat PH, Nelson A, Olson G, et al. Reducing the use of empiric antibiotic therapy in COVID-19 on hospital admission. BMC Infect Dis. 2021;21:516. https://doi.org/10.1186/s12879-021-06219-z.
Abelenda-Alonso G, Padullés A, Rombauts A, Gudiol C, Pujol M, Alvarez-Pouso C, et al. Antibiotic prescription during the COVID-19 pandemic: A biphasic pattern. Infect Control Hosp Epidemiol. 2020;41(11):1371–2.
Pettit NN, Nguyen CT, Lew AK, Bhagat PH, Nelson A, Olson G, et al. Reducing the use of empiric antibiotic therapy in COVID-19 on hospital admission. BMC Infect Dis. 2021;21(1):1–7.
Furukawa D, Graber CJ. Antimicrobial stewardship in a pandemic: picking up the pieces. Clin Infect Dis. 2021;72:e542–4.
De Waele JJ, Schouten J, Beovic B, Tabah A, Leone M. Antimicrobial de-escalation as part of antimicrobial stewardship in intensive care: no simple answers to simple questions—a viewpoint of experts. Intensive Care Med. 2020;46(2):236–44.
De Bus L, Denys W, Catteeuw J, Gadeyne B, Vermeulen K, Boelens J, et al. Impact of de-escalation of beta-lactam antibiotics on the emergence of antibiotic resistance in ICU patients: a retrospective observational study. Intensive Care Med. 2016;42(6):1029–39.
Tabah A, Bassetti M, Kollef MH, Zahar JR, Paiva JA, Timsit JF, et al. Antimicrobial de-escalation in critically ill patients: a position statement from a task force of the European Society of Intensive Care Medicine (ESICM) and European Society of Clinical Microbiology and Infectious Diseases (ESCMID) critically ill patient. Intensive Care Med. 2020;46(2):245–65.
Morel J, Casoetto J, Jospé R, Aubert G, Terrana R, Dumont A, et al. De-escalation as part of a global strategy of empiric antibiotherapy management. A retrospective study in a medico-surgical intensive care unit. Crit Care. 2010;14(6):R225.
Leone M, Bechis C, Baumstarck K, Lefrant JY, Albanèse J, Jaber S, et al. De-escalation versus continuation of empirical antimicrobial treatment in severe sepsis: a multicenter non-blinded randomized noninferiority trial. Intensive Care Med. 2014;40(10):1399–408.
Deshpande A, Richter SS, Haessler S, Lindenauer PK, Yu PC, Zilberberg MD, et al. De-escalation of empiric antibiotics following negative cultures in hospitalized patients with pneumonia: rates and outcomes. Clin Infect Dis Off Publ Infect Dis Soc Am. 2021;72(8):1314–22.
Posteraro B, Cortazzo V, Liotti FM, Menchinelli G, Ippoliti C, De Angelis G, et al. Diagnosis and treatment of bacterial pneumonia in critically ill patients with COVID-19 using a multiplex PCR assay: a large Italian hospital’s five-month experience. Microbiol Spectr. 2021;9(3):e0069521.
Tabah A, Cotta MO, Garnacho-Montero J, Schouten J, Roberts JA, Lipman J, et al. A systematic review of the definitions, determinants, and clinical outcomes of antimicrobial de-escalation in the Intensive Care Unit. Clin Infect Dis. 2016;62(8):1009–17.
Sadyrbaeva-Dolgova S, Aznarte-Padial P, Pasquau-Liaño J, Expósito-Ruiz M, Calleja Hernández MÁ, Hidalgo-Tenorio C. Clinical outcomes of carbapenem de-escalation regardless of microbiological results: a propensity score analysis. Int J Infect Dis. 2019;1(85):80–7.
Schuts EC, Hulscher MEJL, Mouton JW, Verduin CM, Stuart JWTC, Overdiek HWPM, et al. Current evidence on hospital antimicrobial stewardship objectives: a systematic review and meta-analysis. Lancet Infect Dis. 2016;16(7):847–56.
Tabah A, Bassetti M, Kollef MH, Zahar JR, Paiva JA, Timsit JF, et al. Antimicrobial de-escalation in critically ill patients: a position statement from a task force of the European Society of Intensive Care Medicine (ESICM) and European Society of Clinical Microbiology and Infectious Diseases (ESCMID) Critically Ill Patients Study Group (ESGCIP). Intensive Care Med. 2020;46(2):245–65.
Funding
This research received no specific Grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to the methodology, data analysis, and manuscript writing.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict or competing interests to declare.
Ethics approval and consent to participate
The institutional review board of King Faisal Specialist Hospital and Research center approved the study (IRB# 2021-65). All methods followed relevant guidelines and regulations (Declaration of Helsinki). However, informed consent was not collected, given the study's retrospective nature. Therefore, the institutional review board of King Faisal Specialist Hospital and Research center waived the informed consent requirements for this study.
Consent to publication
All participating authors have read, approved, and consented to the publication of this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Aldardeer, N.F., Shukairi, A.N.A.L., Nasser, M.E. et al. Continuation Versus De-escalation of Broad-Spectrum Antibiotic Therapy in Critically Ill COVID-19 Patients. Dr. Sulaiman Al Habib Med J 5, 33–41 (2023). https://doi.org/10.1007/s44229-023-00027-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44229-023-00027-0