Abstract
Patients with poor graft function (PGF) or declining donor chimerism (DC) post allogeneic hematopoietic cell transplantation (HCT) may benefit from a CD34-selected stem cell boost (SCB). We retrospectively studied outcomes of fourteen pediatric patients (PGF: 12 and declining DC: 2), with a median age of 12.8 (range 0.08–20.6) years at HCT, who received a SCB. Primary and secondary endpoints included resolution of PGF or improvement in DC (≥ 15% increase), overall survival (OS) and transplant-related mortality (TRM), respectively. The median CD34 dose infused was 7.47 × 106/kg (range 3.51 × 106–3.39 × 107/kg). Among patients with PGF who survived ≥ 3 months post-SCB (n = 8), we observed a non-significant decrease in the cumulative median number of red cell transfusions, platelet transfusions, and GCSF but not intravenous immunoglobulin doses in the 3 months before and after SCB. Overall response rate (ORR) was 50%, with 29% complete and 21% partial responses. ORR was better in recipients who received lymphodepletion (LD) pre-SCB versus none (75% versus 40%; p = 0.56). The incidence of acute and chronic graft-versus-host-disease was 7% and 14%, respectively. The 1-year OS was 50% (95% CI 23–72%) and TRM was 29% (95% CI 8–58%). SCB was effective in half of our cohort with possible benefit of LD pre-SCB.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Allogeneic hematopoietic stem cell transplantation (HCT), a curative option for many hematological malignancies and disorders, can be associated with poor graft function (PGF) and mixed chimerism (MC). Depending on the underlying primary diagnosis, PGF/MC may necessitate further interventions such as a rapid taper or increase in immunosuppression, stem cell boost (SCB), donor lymphocyte infusion (DLI), or a second HCT [1]. PGF is defined as frequent dependence on blood and/or platelet transfusions and/or growth factors in the absence of other explanations such as disease relapse, drugs or infection [1]. PGF occurs in 5–27% of patients after initial HCT and is associated with a high mortality rate, most often secondary to infection [2]. Mixed chimerism is defined as donor chimerism (DC) between 5 and 95% [3] for both myeloid and lymphoid lineages [1], and occurs with greater frequency following transplant for non-malignant diseases (NMD) and with the use of reduced intensity (RIC) or non-myeloablative conditioning regimens [4].
While PGF can be managed with blood product transfusions or growth factors [Granulocyte colony stimulating factor (G-CSF), thrombopoietin agonists or erythropoietin] [5], this may not be sustainable in the long-term, and is associated with side effects such as iron overload, alloimmunization, thrombosis and bone marrow fibrosis. Similarly, declining DC portends risk of relapse/recurrence of the underlying disease. When compared to DLI, a CD34 SCB is associated with decreased risk of graft versus host disease (GvHD) and, hence, may be the preferred intervention to improve GF or DC [6, 7]. A second HCT, on the other hand, has an increased risk of transplant-related mortality (TRM) and morbidity [8, 9]. While the current literature mostly focuses on outcomes of SCB post-HCT for PGF in adults [2, 3, 10,11,12], there have only been a few pediatric studies that have analyzed outcomes post-SCB in select diseases, such as immunodeficiencies [3] or malignancies [13,14,15]. Therefore, we retrospectively evaluated the efficacy and outcomes of pediatric patients who received a CD34 SCB post-HCT at our center. Two patients in this series have been previously reported [16, 17]. We also reviewed the literature on outcomes of this intervention in pediatric HCT recipients.
2 Methods
2.1 Patients
We obtained approval from our institution’s research board for this retrospective study. All patients who received a CD34 SCB from their original HCT donor for either PGF or MC at our center, from January 2014 to December 2021, were included. Data on demographics, HCT, SCB characteristics, and clinical outcomes were collected and entered into a secure database. PGF was defined as cytopenia(s) affecting any hematopoietic cell line(s) (ANC < 1000/μl, Hb < 8 g/dL, platelets < 30,0000 K/µL) for at least 2 weeks post-HCT requiring the support of transfusions or growth factors in the presence of full DC and absence of relapse, severe GvHD, viral reactivation, and/or drug-related myelosuppression [15]. MC was defined as DC between 5 and 95% in either whole, myeloid, or lymphoid lineages, whereas full DC was defined as having ≥ 95% in all lineages [3]. Stem cells were obtained by apheresis in all but one patient who received a bone marrow (BM) boost. For the former, donors received 10 µg/kg of GCSF for 5 days prior to apheresis for peripheral blood stem cells. The donor apheresis product underwent CD34 selection using the CliniMACS® Milteny device and the fresh product was then infused in patients [18].
2.2 Response Criteria
The primary endpoint was improvement in PGF or MC. Responses for PGF were categorized as complete response (CR: resolution of all cytopenias), partial response (PR: resolution of some, but not all cytopenias), or no response (NR) based on recovery of the underlying parameter at least 30 days post-SCB [10]. Improvement in MC was defined as a rise in DC by ≥ 15% and having DC ≥ 20% 3 months post-SCB; stabilization was defined as a rise in DC by < 15% but with DC ≥ 20% 3 months after the boost.1 NR was defined as a decline/no change in DC at 3 and 12 months post-SCB or the need for a second allogenic HCT [3]. Secondary endpoints included cumulative incidence of acute and chronic GvHD, 1-year overall survival (OS), and TRM. OS was defined as the time from SCB to time of death from any cause or censoring. TRM was defined as deaths without signs of relapse of primary disease post-SCB. Acute and chronic GvHD were graded according to Glucksberg’s criteria [19] and NIH consensus guidelines, respectively [20].
2.3 Statistical Analysis
Descriptive statistics were used to summarize all the data. Frequencies and percentages were used to summarize categorical variables, and median and range for quantitative variables. Wilcoxon signed-rank tests were used to compare the number of pRBC and platelet transfusions, GCSF, and IVIG doses before and after SCB. The comparison of CR + PR i.e., overall response rate (ORR) among those who did and did not receive lymphodepletion (LD) was done with a Fisher’s exact test. OS was estimated using the Kaplan–Meier method and presented with a corresponding 95% confidence interval (CI). The TRM rate was summarized as a percentage and 95% CI. P values less than 0.05 were considered statistically significant. We compared the median cumulative number of pRBC, platelet transfusions, GCSF and IVIG doses in the three-month preceding and following SCB in patients with PGF who survived ≥ 3 months post-SCB. Analyses were completed using SAS software, version 9.4 (SAS Institute, Cary, NC).
3 Results
Fourteen (7 male) allogeneic HCT recipients, with a median age of 12.8 (range 0.08–20.6) years at HCT, received a CD34 SCB during the study period (Table 1). This included 5 patients with a malignant disease and 9 with a NMD. Nine received myeloablative (MA) and 5 RIC regimens. Amongst these, one patient (P#11) received a 2nd MA HCT following graft failure (GF) post-1st HCT. Bone marrow (BM; n = 12) or peripheral blood stem cells (PBSC; n = 2) were obtained from matched sibling donors (MSD; n = 3), matched unrelated donors (MUD; n = 7), and haploidentical donors (n = 4). Twelve (86%) had PGF and 2 (14%) had declining DC pre-SCB (Fig. 1). Prior to SCB, all but two patients had a history of infections with five (42%) patients with PGF undergoing active treatment for infections at the time of SCB (Table 2). BM biopsy performed in 10 patients with PGF pre-SCB demonstrated a median cellularity of 15% (range 0–60%). Amongst patients with PGF, 1 had single-line cytopenia (P#1: thrombocytopenia), 1 had bi-lineage cytopenia (P#6: anemia, neutropenia), and 8 had pancytopenia. Thrombopoietin agonists agonists were not considered for the P#1 due to risk BM fibrosis in a heavily treated patient with therapy-related AML/MDS. All patients received blood products (pRBCs, platelets) and growth factors ± intravenous immunoglobulin (IVIG) for ongoing cytopenias. P#11 (Severe congenital neutropenia) and P #12 (OMS, Omenn’s syndrome) developed B-cell aplasia and required monthly IVIG for approximately 4 and 19 years, respectively, pre-SCB. While P#11 developed B cell aplasia following rituximab therapy for EBV reactivation, P#12 had B cell aplasia in the setting of persistently low donor CD19 chimerism (3%) with recurrent episodes of bacterial sinusitis. In the two patients with MC, DC pre-SCB were: whole blood (WB) 41 and 45%; CD3: 56 and 81%; CD33: 30 and 41%, respectively. Despite rapid weaning of immunosuppression (tacrolimus) over 2 weeks, there was no improvement in DC in either of these patients. P#2 was also subsequently treated with a 3-month course of sirolimus with no effect. Six patients developed acute GvHD (Grade I-II in 4, Grade III-IV in 2 patients), and one patient developed severe chronic GVHD following their HCT, all of which resolved prior to a SCB [10].
The median interval between SCB and prior HCT was 0.43 years (range 0.1–19.2). Three patients with PGF (P # 6, 11, and 12) received a CD34 SCB more than 1-year post- HCT. P#6 had autoimmune hemolytic anemia (AIHA) with neutropenia that was refractory to treatment with several agents (steroids, cyclosporine, eculizumab, and daratumumab). Therefore, she received LD followed by a CD34 SCB 13 months post-HCT. P#11 and P#12 were treated for prolonged B cell aplasia as previously described.
Only one patient in our cohort received a marrow boost (P#13). The median CD34 and CD3 doses infused were 7.47 × 106/kg (range 3.51 × 106–3.39 × 107/kg) and 1.74 × 103/kg (range 7.2 × 102–3.10 × 107/kg). Nine patients were briefly maintained on immunosuppression post-SCB (Table 1). Amongst the 12 patients with PGF, after excluding four who died < 3 months post-SCB, in the remaining eight there was a non-significant decrease in the median cumulative number of pRBC [pre: 1 (range 0–6) versus 0 (range 0–6); p = 0.48], platelet transfusion [pre: 4 (range 0–21) versus 0 (range 0–21); p = 0.06], GCSF [pre: 2 (range 0–36) versus post: 0 (range 0–28); p = 0.19], but not IVIG doses [pre: 1 (range 0–2) versus 1 (range 0–6); p = 0.99] (Fig. 2).
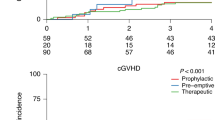
The ORR in our cohort at last follow-up was 50% (n = 7), with CR in 29% (n = 4) and PR in 21% (n = 3). Responses were observed at a median of 1-month post-SCB. The ORR in those with MC was 50% (1 CR, 1 NR) (Fig. 1) and 50% in those with PGF (3 CR, 3 PR, 6 NR). Amongst the latter, P#1 with single-line cytopenia had a CR, P#6 with bi-lineage cytopenia had a PR, and of the 8 with pancytopenia, there were 2 CR, 2 PR, and 4 NR. The two patients with B-cell aplasia had NR and continued to receive monthly IVIG at the last follow-up. Comparing those with malignant diagnosis versus NMD, 50% of those with history of a malignancy had a CR (n = 3), 33% a PR (n = 2), and 17% NR (n = 1); 12.5% of those with NMD had a CR (n = 1), 12.5% had a PR (n = 1), and 75% had NR (n = 6). P#13, who received a BM boost, had NR and subsequently developed GF with return of sickle cell disease. Four patients (P#2, 6, 10, and 13) in our cohort received LD chemotherapy pre-SCB. This included 1 patient with MC (P#2) and 3 with PGF (Table 1). The ORR in patients who received LD (n = 4) and those who did not (n = 10), was 75% (2 CR, 1 PR, 1 NR) versus 40% (2 CR, 2 PR and 6 NR), respectively (p = 0.56).
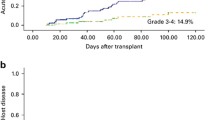
Following SCB, new infections occurred in 4 patients and these included viral reactivations: EBV (P#2 and 13), adenovirus (P#6) and disseminated Candidemia and Enterococcus faescium (P#14) (Table 2). New onset GVHD post-SCB occurred in three patients: Grade II aGVHD in one (7%) and mild cGVHD in 2 patients (14%). At a median follow up of 1.96 years (range 0.0025–9.05 years) post-SCB, 43% (n = 6) of patients were alive. The 1-year OS was 50% (95% CI 23–72%) and TRM was 29% (95% CI 8–58%) (Fig. 3). Causes of mortality included relapse of malignancy (n = 4), disseminated fungal infection (n = 2), right heart failure secondary to anemia (n = 1), and hepatorenal failure (n = 1).
4 Discussion
A CD34-selected SCB, unlike DLI, is associated with decreased risk of GvHD and, hence, may be a preferred treatment strategy for PGF or MC following an allogeneic HCT [6, 7]. Prabahran and colleagues described three mechanisms causing PGF: a decline in the number or efficacy of the stem cells (seed), abnormalities in the BM microenvironment (soil), and immunosuppression of hematopoiesis (environment) [21]. The discussed potential treatment options were CD34-selected SCB, TPO agonists and G-CSF (seed), mesenchymal stromal cells, and antioxidants (soil), T regulatory cell infusion, emapalumab and JAK inhibition (environment). A CD34 SCB is particularly advantageous in patients with NMDs, where graft-versus-leukemia and associated GvHD are of no benefit. However, if there is no response to a SCB by 3 months, an alternative treatment should be pursued. [3]. Through our report, we further demonstrate the effectiveness of a SCB in pediatric HCT recipients. We observed an ORR of 50% in our study cohort including 29% CR and 21% PR. We also noted a decrease in requirements for blood products and GCSF doses in the 3 months post-SCB in patients with PGF. There was, however, no decrease in IVIG requirements in patients with prolonged B cell aplasia. One of the two patients with MC had a CR. A greater proportion of patients who received LD pre-SCB had a response than those who did not.
Three pediatric and three mixed pediatric/adult studies have reported on the use of a SCB for PGF or MC in pediatric patients (Table 3) [12]. While two of these reports [3, 10] focus only on patients with primary immunodeficiencies (PID), the remainder, like ours, included patients with both malignant and NMD [2, 11, 12, 22]. Parallel with our observations, the OS, aGvHD, and cGvHD rates in these studies were 39–100%, 0–12%, and 0–6.2% (Table 3). In contrast, unmanipulated DLI, was associated with 40–60% risk of aGvHD (20–35% with grade III–IV aGvHD) and 33–61% risk of cGvHD, resulting in a decreased OS.[7, 23] In a recent large metanalysis of 209 adults who received a SCB for PGF, the overall pooled ORR, CR and PR were 80%, 72%, and 13%, respectively, but that study did not delineate the type of cytopenia pre-SCB. [6] While the CR rate in our study (29%) is lower than that and those from a few pediatric studies (50–79%) [2, 10, 12], it is similar to that reported by Mianaridi (36%) [11] and Chandra (25%) [3] (Table 3). Per the latter’s report, only 1/3 of patients with MC respond to a SCB. Therefore, the high incidence of pancytopenia (80%) amongst patients with PGF and the inclusion of two patients with MC could be a potential explanation for the lower CR rate in our study.
All patients in our cohort received fresh products from their donors. In two studies involving pediatric patients, cryopreserved products were administered to half of the patients [11, 22]. Ghobadi et al. [24] showed that a CD34 SCB from a cryopreserved product, though associated with a lower CD34 yield, still had equally effective responses in treated patients (63% CR) when compared to those who got fresh products (61% CR). In a study of PID patients who received a SCB for PGF or MC, two patients who received a BM boost, achieved CR but then developed GVHD [10]. The singular patient who received a BM boost in our study had NR and did not develop GVHD. A pediatric study involving 16 patients found that a higher proportion of recipients who received a CD34 cell dose > 6.6 × 106/kg (78%) had a response compared to those who received < 6.6 × 106/kg (57%) [2]. A study with 50 patients, however, found no difference in CD34 dose between responders and non-responders. They observed a threshold effect at 3.25 × 106 /kg, which resulted in an optimal increase in neutrophil count, with higher doses showing no further increases [11]. All patients in our study received a dose greater than 3.25 × 106/kg, and all but two patients (1CR and 1PR) received a dose greater than 6.5 × 106/kg.
Multiple studies have demonstrated that response rates are higher for single-lineage compared to bi-lineage or tri-lineage cytopenias. For instance, Berger et al. reported response rates of 80% for single-lineage and 44% for bi-lineage cytopenia in their patients [2, 22]. Other factors predictive of a response to SCB include absence of infection, recipient-donor gender matching, shared donor/recipient (D/R) CMV seronegative status, absence of CMV reactivation [12] and donor age < 40 years [11]. Donor type (sibling versus non sibling) did not seem to impact outcomes in most studies [1, 11]. We could not determine the impacts of these factors in our limited cohort, as all but 2 (1 CR and 1 PR) patients with PGF had pancytopenia. Additionally, only 2 D/R pairs shared CMV seronegative status with NR in both recipients (Table 1). We also found a similar rate of response in gender mismatched cohorts (2 CR 1 PR and 3 NR) versus gender matched (2 CR, 2 PR, 4NR) cohorts (data not shown).
Similar to the Fraint et al.’s report, nearly half of our patients with PGF had active infections around the time of the SCB [22]. Infections not only cause PGF but can also be a major cause of failure of response and deaths following SCB [2]. In our limited cohort, amongst the 7 with NR, 3 had active infections at the time of SCB resulting in death in 2 of these patients (Table 2). Patients with a CR following a SCB have been shown to have a better OS compared to those with a PR or NR [11, 12, 25]. The 5-year OS in a mixed adult-pediatric study of 62 patients was 74%, 17% and 22% in patients with a CR, PR and NR, respectively [12]. In contrast, we did not detect such a difference, which may be attributed to our small sample size. In our study, 50% of patients with CR, 0% with PR, and 58% with NR were alive at the last follow-up. Notably four patients with NR had NMD with two of them receiving a SCB > 1 year post HCT. Therefore, these factors likely contributed to their favorable OS at last follow-up. Berger et al. found that the majority of deaths occurred within the first 6 months of a SCB [2], consistent with our observation wherein six of the eight deaths occurred within the same timeframe.
Like our study, Mainardi et al. also noted a significant decrease in red cell and platelet transfusions (1 and 7 versus 0) at 8-weeks post-SCB from non-sibling donors [11]. Slatter et al. reported improved B cell function and IVIG independence in 7 of 12 responders, and a CR in a patient with AIHA. However, Fraint et al. reported death in a patient with AIHA, despite an initial CR [22]. In our cohort, the two patients with B cell aplasia had NR, and the single patient with AIHA had a PR that was not sustained. Berger et al. excluded patients who received chemotherapy/LD, prior to SCB. However, we elected to include these patients as LD is often used to eliminate residual host immunity thought to mediate PGF/MC, thereby facilitating engraftment [16]. We utilized this strategy in patients with NMD or MDS who are usually chemotherapy-naïve with a robust host immune response, which can mediate graft rejection. Slatter et al. used LD [anti-thymocyte globulin (ATG) or alemtuzumab] pre-SCB in two patients with PID following which one had a CR, the other NR and proceeded to a 2nd HCT. Fraint et al. also included 4 patients with MC (DC < 90%) and pancytopenia due to PGF who received LD (3 with ATG and 1 with Fludarabine and ATG). The outcomes of these patients were not reported separately. [22] Our study was limited by a small sample size and its retrospective nature; despite this, our observations mirror other published reports and add to the literature on the utility of SCB for treatment of PGF or MC after HCT for both malignant and NMD.
5 Conclusion
SCB was associated with lower rates of GvHD in our cohort and a non-significant but decreased need for blood product support and GCSF in patients with PGF. Patients with NMD/MDS may benefit from lymphodepletion prior to SCB. Overall, our data support the use and consideration of SCB as a strategy for treatment of PGF or MC after initial HCT in pediatric patients.
Availability of Data and Material
These will be made available upon reasonable request to authors.
Abbreviations
- HCT:
-
Hematopoietic cell transplant
- PGF:
-
Poor graft function
- MC:
-
Mixed chimerism
- DC:
-
Donor chimerism
- GvHD:
-
Graft versus host disease
- SCB:
-
Stem cell boost
- OS:
-
Overall survival
- ORR:
-
Overall response rate
- CR:
-
Complete response
- PR:
-
Partial response
- NR:
-
No response
- DLI:
-
Donor lymphocyte infusion
- NMD:
-
Non-malignant diseases
- LD:
-
Lymphodepletion
- aGVHD:
-
Acute graft versus host disease
- RIC:
-
Reduced intensity chemotherapy
- MAC:
-
Myeloablative chemotherapy
- NRM:
-
Non-relapse mortality
- TRM:
-
Transplant related mortality
- BM:
-
Bone marrow
- PBSC:
-
Peripheral blood stem cells
- MSD:
-
Matched sibling donor
- MURD:
-
Matched unrelated donor
- SCN:
-
Severe congenital neutropenia
- OMS:
-
Omenn syndrome
- IVIG:
-
Intravenous immunoglobulin
- WB:
-
Whole blood
- MDS:
-
Myelodysplastic syndrome
- GCSF:
-
Granulocyte colony stimulating factor
- cGVHD:
-
Chronic graft versus host disease
References
Kharfan-Dabaja MA, Kumar A, Ayala E, Aljurf M, Nishihori T, Marsh R, et al. Standardizing definitions of hematopoietic recovery, graft rejection, graft failure, poor graft function, and donor chimerism in allogeneic hematopoietic cell transplantation: a report on behalf of the American Society for Transplantation and Cellular Therapy. Transplant Cell Ther. 2021;27(8):642–9. https://doi.org/10.1016/j.jtct.2021.04.007. (Epub 2021/07/27. PubMed PMID: 34304802).
Berger M, Faraci M, Saglio F, Giardino S, Ernestina Vassallo E, Prete A, et al. CD34+ selected peripheral blood Stem Cell Boost (SCB) for Poor Graft Function (PGF) or mixed chimerism in pediatric patients, after hematopoietic stem cell transplantation: results of a retrospective multicenter study. Pediatr Transplant. 2021;25(5):e13909. https://doi.org/10.1111/petr.13909. (PubMed PMID: 33141997. Epub 2020/11/04).
Chandra S, Bleesing JJ, Jordan MB, Grimley MS, Khandelwal P, Davies SM, et al. Post-transplant CD34(+) selected stem cell “boost” for mixed chimerism after reduced-intensity conditioning hematopoietic stem cell transplantation in children and young adults with primary immune deficiencies. Biol Blood Marrow Transplant. 2018;24(7):1527–9. https://doi.org/10.1016/j.bbmt.2018.03.013. (PubMed PMID: 29555312. Epub 2018/03/21).
Zimmerman C, Shenoy S. Chimerism in the realm of hematopoietic stem cell transplantation for non-malignant disorders-a perspective. Front Immunol. 2020;11:1791. https://doi.org/10.3389/fimmu.2020.01791. (PubMed PMID: 32903736; PubMed Central PMCID: PMCPMC7438804. Epub 2020/09/10).
Marotta S, Marano L, Ricci P, Cacace F, Frieri C, Simeone L, et al. Eltrombopag for post-transplant cytopenias due to poor graft function. Bone Marrow Transplant. 2019;54(8):1346–53. https://doi.org/10.1038/s41409-019-0442-3. (Epub 20190124. PubMed PMID: 30679824).
Shahzad M, Siddiqui RS, Anwar I, Chaudhary SG, Ali T, Naseem M, et al. Outcomes with CD34-selected stem cell boost for poor graft function after allogeneic hematopoietic stem cell transplantation: a systematic review and meta-analysis. Transplant Cell Ther. 2021;27(10):877.e1-e8. https://doi.org/10.1016/j.jtct.2021.07.012. (Epub 2021/07/21. PubMed PMID: 34284148).
Haines HL, Bleesing JJ, Davies SM, Hornung L, Jordan MB, Marsh RA, et al. Outcomes of donor lymphocyte infusion for treatment of mixed donor chimerism after a reduced-intensity preparative regimen for pediatric patients with nonmalignant diseases. Biol Blood Marrow Transplant. 2015;21(2):288–92. https://doi.org/10.1016/j.bbmt.2014.10.010. (Epub 2014/12/03. PubMed PMID: 25464116).
Forlanini F, Zinter MS, Dvorak CC, Bailey-Olson M, Winestone LE, Shimano KA, et al. Hematopoietic cell transplantation-comorbidity index score is correlated with treatment-related mortality and overall survival following second allogeneic hematopoietic cell transplantation in children. Transplant Cell Ther. 2022;28(3):155.e1-e8. https://doi.org/10.1016/j.jtct.2021.11.015. (Epub 2021/12/02, PubMed PMID: 34848362).
Yalniz FF, Saliba RM, Greenbaum U, Ramdial J, Popat U, Oran B, et al. Outcomes of second allogeneic hematopoietic cell transplantation for patients with acute myeloid leukemia. Transplant Cell Ther. 2021;27(8):689–95. https://doi.org/10.1016/j.jtct.2021.05.007. (Epub 2021/05/24, PubMed PMID: 34023569. PubMed Central PMCID: PMCPMC8316329).
Slatter MA, Bhattacharya A, Abinun M, Flood TJ, Cant AJ, Gennery AR. Outcome of boost haemopoietic stem cell transplant for decreased donor chimerism or graft dysfunction in primary immunodeficiency. Bone Marrow Transplant. 2005;35(7):683–9. https://doi.org/10.1038/sj.bmt.1704872. (PubMed PMID: 15723084 Epub 2005/02/22).
Mainardi C, Ebinger M, Enkel S, Feuchtinger T, Teltschik HM, Eyrich M, et al. CD34(+) selected stem cell boosts can improve poor graft function after paediatric allogeneic stem cell transplantation. Br J Haematol. 2018;180(1):90–9. https://doi.org/10.1111/bjh.15012. (Epub 2017/12/06, PubMed PMID: 29205259).
Cuadrado MM, Szydlo RM, Watts M, Patel N, Renshaw H, Dorman J, et al. Predictors of recovery following allogeneic CD34+-selected cell infusion without conditioning to correct poor graft function. Haematologica. 2020;105(11):2639–46. https://doi.org/10.3324/haematol.2019.226340. (Epub 2020/11/03, PubMed PMID: 33131253, PubMed Central PMCID: PMCPMC7604618).
Haen SP, Schumm M, Faul C, Kanz L, Bethge WA, Vogel W. Poor graft function can be durably and safely improved by CD34+-selected stem cell boosts after allogeneic unrelated matched or mismatched hematopoietic cell transplantation. J Cancer Res Clin Oncol. 2015;141(12):2241–51. https://doi.org/10.1007/s00432-015-2027-x. (Epub 2015/08/15 PubMed PMID: 26272482).
Oyekunle A, Koehl U, Schieder H, Ayuk F, Renges H, Fehse N, et al. CD34(+)-selected stem cell boost for delayed or insufficient engraftment after allogeneic stem cell transplantation. Cytotherapy. 2006;8(4):375–80. https://doi.org/10.1080/14653240600735784. (Epub 2006/08/23 PubMed PMID: 16923613).
Klyuchnikov E, El-Cheikh J, Sputtek A, Lioznov M, Calmels B, Furst S, et al. CD34(+)-selected stem cell boost without further conditioning for poor graft function after allogeneic stem cell transplantation in patients with hematological malignancies. Biol Blood Marrow Transplant. 2014;20(3):382–6. https://doi.org/10.1016/j.bbmt.2013.11.034. (Epub 2013/12/11 PubMed PMID: 24321747).
Rangarajan HG, Crowell SA, Towerman AS, Shenoy SS. CD34-selected stem cell boost as therapy for late graft rejection following allogeneic transplantation for sickle cell disease. Bone Marrow Transplant. 2022;57(10):1592–4. https://doi.org/10.1038/s41409-022-01749-9. (Epub 2022/07/08 PubMed PMID: 35798858).
Yonkof JR, Basu A, Redmond MT, Dobbs AK, Perelygina L, Notarangelo LD, et al. Refractory, fatal autoimmune hemolytic anemia due to ineffective thymic-derived T-cell reconstitution following allogeneic hematopoietic cell transplantation for hypomorphic RAG1 deficiency. Pediatr Blood Cancer. 2022. https://doi.org/10.1002/pbc.30183. (Epub 2022/12/31, PubMed PMID: 36583469).
Ings SJ, Balsa C, Leverett D, Mackinnon S, Linch DC, Watts MJ. Peripheral blood stem cell yield in 400 normal donors mobilised with granulocyte colony-stimulating factor (G-CSF): impact of age, sex, donor weight and type of G-CSF used. Br J Haematol. 2006;134(5):517–25. https://doi.org/10.1111/j.1365-2141.2006.06223.x.
Glucksberg H, Storb R, Fefer A, Buckner CD, Neiman PE, Clift RA, et al. Clinical manifestations of graft-versus-host disease in human recipients of marrow from HL-A-matched sibling donors. Transplantation. 1974;18(4):295–304. https://doi.org/10.1097/00007890-197410000-00001. (PubMed PMID: 4153799).
Jagasia MH, Greinix HT, Arora M, Williams KM, Wolff D, Cowen EW, et al. National Institutes of Health Consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. The 2014 diagnosis and staging working group report. Biol Blood Marrow Transplant. 2015;21(3):389-401.e1. https://doi.org/10.1016/j.bbmt.2014.12.001. (Epub 20141218, PubMed PMID: 25529383, PubMed Central PMCID: PMCPMC4329079).
Prabahran A, Koldej R, Chee L, Ritchie D. Clinical features, pathophysiology, and therapy of poor graft function post-allogeneic stem cell transplantation. Blood Adv. 2022;6(6):1947–59. https://doi.org/10.1182/bloodadvances.2021004537. (Epub 2021/09/08 PubMed PMID: 34492685. PubMed Central PMCID: PMCPMC8941468).
Fraint E, Farooki SS, Klein E, Mauguen A, Prockop SE, Scaradavou A, et al. Durable engraftment and excellent overall survival after CD34-selected peripheral blood stem cell boost in pediatric patients with poor graft function following allogeneic stem cell transplantation. Transplant Cell Ther. 2022. https://doi.org/10.1016/j.jtct.2022.09.027. (Epub 2022/10/10, PubMed PMID: 36210027).
Frey NV, Porter DL. Graft-versus-host disease after donor leukocyte infusions: presentation and management. Best Pract Res Clin Haematol. 2008;21(2):205–22. https://doi.org/10.1016/j.beha.2008.02.007. (Epub 2008/05/28, PubMed PMID: 18503987, PubMed Central PMCID: PMCPMC2504712).
Ghobadi A, Fiala MA, Ramsingh G, Gao F, Abboud CN, Stockerl-Goldstein K, et al. Fresh or cryopreserved CD34. Biol Blood Marrow Transplant. 2017;23(7):1072–7. https://doi.org/10.1016/j.bbmt.2017.03.019. (Epub 2017/03/18 PubMed PMID: 28323004. PubMed Central PMCID: PMCPMC5515540).
Berger M, Faraci M, Saglio F, Giardino S, Ernestina-Vassallo E, Prete A, et al. CD34+ selected peripheral blood Stem Cell Boost (SCB) for Poor Graft Function (PGF) or mixed chimerism in pediatric patients, after hematopoietic stem cell transplantation: Results of a retrospective multicenter study. Pediatr Transplant. 2020. https://doi.org/10.1111/petr.13909. (Epub 2020/11/04 PubMed PMID: 33141997).
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
SB collected and analyzed data, wrote and edited the manuscript. JS performed statistical analysis and edited the manuscript. VP, RB and RA edited the manuscript. HGR designed the study, collected data, contributed to analysis, wrote and edited the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical Approval
This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Human Investigation Committee (IRB) of Nationwide Children’s Hospital approved this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bowman, S., Stanek, J., Bajwa, R. et al. CD34 Stem Cell Boost in Pediatric Allogeneic Stem Cell Transplant Recipients: A Case Series and Review of Literature. Clin Hematol Int 5, 155–164 (2023). https://doi.org/10.1007/s44228-023-00042-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44228-023-00042-w