Abstract
1.28 billion adults worldwide have high pressure, and only 21% of people have it under control. If high blood pressure (BP) is not diagnosed and treated properly, then there is a high risk for cardiovascular diseases, the main cause of mortality. Ultrasound has emerged as a potential medical imaging system to monitor cardiovascular health. It is comfortable, noninvasive, safe, and a very well-established and well-known technology. However, there are currently no commercial single ultrasound systems to directly quantify vascular parameters, without the need for complex imaging algorithms, additional software-based solutions, and high energy demands that limit portable and prolonged measurements. In this paper, we present the steps to design an image-free novel ultrasound device to continuously extract vital parameters, with a focus on BP. Moreover, as the BP waveforms are amplified toward the periphery (i.e., from the aorta to the radial artery), we applied mathematical models and algorithms, specific to the site of measurement, to accurately extract BP. We validated these algorithms in silico, in vitro, and ex vivo, where tissue and artery phantoms help emulate human physiology. In young subjects, an in silico pulse pressure (PP) correlation of 0.978 and a mean difference of (– 2.85 ± 2.57) mmHg at the radial artery were achieved. The ex vivo PP correlation was 0.986, with a mean difference of (1.72 ± 3.29) mmHg. Soon thereafter, in vivo measurements of BP and stiffness, and their correlation analysis will be performed to corroborate the accuracy of the developed proof-of-concept device.
Similar content being viewed by others
1 Introduction
Hypertension is a major cause of premature death worldwide and 46% of adults with hypertension are unaware of their condition [1]. By diagnosing and treating hypertension, many cardiovascular diseases can be prevented. Up till now, the “gold standard” of validated techniques for noninvasive reading of blood pressure (BP) requires blood flow to be blocked completely for the measurement. This is done through an arm cuff, placed around the patient’s upper arm that is inflated with air. After blocking the artery, air is released, and values of systolic and diastolic BP are measured with a stethoscope and a manometer [2]. However, these devices often cause discomfort for those who need frequent BP monitoring, such as hypertensive patients or postoperative organ transplant patients. In such cases, BP must be measured every 30 min for 24 h, even when the patient is sleeping [3]. There is a significant need for a noninvasive, unobtrusive, and continuous BP monitoring approach, with a simplified remote healthcare data integration process.
Ultrasound is a real-time imaging modality that measures the wall locations of human vessels with high precision. The acoustic wave emitted by an ultrasound device produces an echo when an acoustic impedance difference between two materials occurs. In an artery, the acoustic wave propagates at different speeds between the muscular tissue (1580 m/s), arterial walls (intima layer 1590 m/s, inner and outer media 1626 m/s and 1699 m/s [4], respectively), and the blood (1575 m/s [5]) that transports the nutrients through the body.
Due to this effect, ultrasound transducers receive acoustic signals delayed in time (in the form of echoes), which recorded in time give us information about the mechanic changes of vessels in time. Ultrasound is also able to see the scattering of the blood cell particles, which is used to monitor blood hemodynamics. Using models and calibration values, those recordings are converted into arterial distensibility, stiffness index, compliance, and BP. Thus, key parameters to predict cardiovascular risks can be noninvasively and continuously measured via ultrasound [6,7,8].
On top of that, advances in new transducer technologies and microsystems make possible the fabrication of image-free ultrasound patches that reduce operator dependency, are wearable, comfortable, and allow for continued cardiovascular monitoring even while doing exercise [7]. Ultrasound therefore presents a promising technology for monitoring individual biomarkers as indicators of aging and cardiovascular disease risk.
However, ultrasound systems still face many challenges, including power-efficiency driving of transducers, low-noise recording of ultrasound echoes, high-attenuation medium (human tissues), and low quality of the images [9]. To better assess cardiovascular health and vascular age, we developed a low-cost and low-energy ultrasound device and implemented patient-specific models to better derive BP from distension waveforms. To guarantee the accurate monitoring of vital parameters, we pay special attention to three main aspects (see Fig. 1): (01) Specification for device design and development with a compromise between resolution, patient safety, and energy saving; (02) Determination of the best artery model/algorithm to extract cardiovascular parameters specifically for each patient and arterial site; (03) Device validation in the laboratory (in vitro, ex vivo) and in a clinical environment (in vivo, in progress) attending to the specific medical device regulations and reference device used for validation.
a Goals needed to achieve accurate monitoring of vital parameters by employing portable devices. b Accuracy levels, patient comfort, and risks are affected by the methods used during device development (01), and the algorithms or models implemented to derive the cardiovascular parameters (02). Once the proof-of-concept device is available it is validated (03), first in a laboratory environment (in vitro and ex vivo), and later it will be done in animals or humans (in vivo) to assess its performance and validity as a medical device
This review summarizes my Career Development presentation at Artery 2023 (Bonn, Germany). It discusses the methods that we applied to develop a low-consumption, safe, operator-independent, and noninvasive proof-of-concept ultrasound device for accurate and patient-specific vital parameter monitoring. In Section II, the fundamentals of device development to measure arterial diameter are explained. In Section III, vascular models and algorithms to derive BP from the arterial diameter are introduced. In Section IV, the creation of mock circulatory loops (MCL) for in vitro and ex vivo validation is described. The review is finalized with an outlook of our results and the highlight of future research possibilities.
2 Ultrasound Device Development
The impact on the market and exponential growth of wearables, which is expected to reach USD 931.31 billion by 2030 [10], requires further research on the integration of new microtechnologies and sensors into compact armbands and conformable patches for continuous monitoring of cardiovascular health. Specifically, ultrasound has been introduced in the wearable market through the creation of two new generations for the microfabrication of transducers: capacitive and piezoelectric micromachined transducers (CMUTs and PMUTs, respectively [11]). CMUTs are used for high bandwidth and resolution, while PMUTs offer their main advantage in terms of low-power requirements. Both technologies are easily integrated with microchips and show ongoing research and medical potential as stretchable patches and easy-to-wear wristbands [6, 7, 12,13,14]. Most of their applications are found in intravascular ultrasonography and endoscopy [11, 15].
In contrast to CMUTs and PMUTs, conventional piezoelectric-based transducers are the most widely chosen option for medical device production due to their mature technology, reliability, low cost, and broad knowledge of the fabrication process. In the market, a wearable piezoelectric-based ultrasound device for blood flow measurement is available [16]. Moreover, we demonstrated the functionality of a new bulk 5 MHz piezoelectric ultrasound probe [17]. The developed probe is composed of three sensors placed geometrically in a trapezoidal configuration. The sensor in the middle is used in amplitude mode (A-Mode) to detect the luminal diameter of the radial artery, whereas the other two transducers on the side are used for flow measurements based on the frequency shift produced by the movement of erythrocytes (Doppler mode).
In [17], we achieve precise measurement of arterial diameter in A-Mode by determining the difference in time of flight between echo signals from the anterior and posterior vessel walls. Thanks to the inclusion of a peak-detector receiver and high sample rates (125 Mega-Samples Per Second) during digitalization, we increase the vertical and the horizontal resolutions for accurate monitoring of diameter variations during the pulsation of the artery. Finally, we identified biomarkers of arterial hemodynamics by the application of signal processing, arterial models, and corresponding calibration parameters to the acquired raw data.
Important parameters obtained in the literature with image-free ultrasound devices are lumen diameter and arterial wall motion [18, 19], local and regional pulse wave velocity (PWV) [17, 20], intima-media thickness [17, 21] BP and compliance [6,7,8, 22], and blood flow [16]. Concretely, in [7], even continuous measurements of BP during exercise were possible thanks to the design of a conformal stretchable ultrasonic patch. In [6], BP measurements derived from in vivo ultrasonic acquisitions of arterial diameter distension achieved high precision (within 2 mmHg) and high accuracy (grade A). Moreover, they also monitored the PWV using electrodes and the developed ultrasound device.
3 Derivation of Blood Pressure
The heart pumps blood through the arteries in our body in a pulsatile manner. Changes in blood flow velocity U contribute to continuous diameter D changes in our arteries. As seen in Fig. 2a, continuous acquisitions of U and D via ultrasound are converted into BP waveform P(t) by applying specific arterial models. Those models require initial BP calibration values, obtained with measurements at the left brachial artery by the gold standard cuff sphygmomanometer (see Fig. 2b).
Illustration of the concept of the derivation of BP from the distension and blood flow velocity waveform using ultrasound. a The acquired diameter and/or velocity waveform from the sensor is converted into the pressure waveform by applying validated models and initial mean arterial pressure (MAP) and diastolic BP (DBP) values. b Schematic of the wearable ultrasound that acquires the physiological signals of either the ulnar or radial artery. Simultaneously, the MAP and DBP values are measured at the brachial artery using the gold standard cuff sphygmomanometer for calibration
Multiple models to derive BP can be found in the literature [23,24,25,26,27]. All of those models assume that the artery is rotationally symmetrical so that the area waveform in time A(t) is equivalent to:
Due to the pulsatile characteristics of the artery, A(t) changes in each heart cycle and acquires minimum and maximum values, named the diastolic and systolic luminal areas \({(A}_{d}\), \({A}_{s})\), respectively.
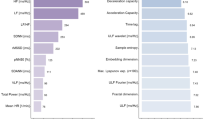
In our research in [28], we compared the state-of-the-art transfer functions to derive BP. Most of those transfer functions are based on the A-Mode ultrasound signals (diameter distension), while others also include pulse wave Doppler signals (blood velocity) as input (see Fig. 2a). We showed that BP can be accurately derived from the diameter distension acquired by ultrasound by applying three best-performing models: linear model (M1), exponential model (M2), and Bramwell–Hill model (M3) [28]. The simplified equations of these three models are included in Fig. 3a. Concretely, in M3, the local PWV in the Bramwell–Hill equation can be extracted by the diameter-blood flow velocity (ln DU-loop) method and the flow-area (QA-loop) method as explained in [29] and [30]. A non-invasive method to measure local PWV is using ultrasound-based pulse wave imaging [31].
Comparison of the three best-performing models (M1, M2, and M3) for BP acquisition with ultrasonic devices from our previous publication [30]. a Transfer BP and calibration functions for the three best-performing models. The exponential model is calibrated through a previous determination of the stiffness coefficient. PWV in M3 is the local pulse wave velocity, and \(\rho\) is the blood density. b Mean pulse pressure (PP) and systolic BP (SBP) difference between the three models at three main peripheral arteries (carotid, brachial, and radial) for a young population with a size of n = 1458
Calibration also plays an important role in accurate BP measurements. In Fig. 3a, the calibration factors for models M1, M2, and M3 are indicated as k, α, and m, respectively. In M1 and M3, the conversion factors are calibrated to the MAP and DBP and use a linear calibration [28]. However, in M2, the factor α (stiffness coefficient) is determined by the cuff measurements of DBP and SBP \({(P}_{s}\) and \({P}_{d})\), at the brachial artery. Because \({P}_{d}\) and MAP are relatively constant throughout most of the arterial tree [29], but \({P}_{s}\) changes significantly, a correction factor of \(\alpha\) (\({\alpha }_{i}\) in Fig. 3), is applied for a certain number of iterations \(i\) until the mean pressure \(\overline{{P }_{i}(t)}\) of the projected waveform converges to the brachial MAP. For more information about this correction, please refer to [23].
In [28], we compared in silico the three best-performing models (M1, M2, and M3) for young (25- and 35-year-old) subjects (n = 1458) at carotid, brachial, and radial arteries. The in silico data was obtained from an open-source database and was validated with in vivo measurements [32]. Results are shown in Fig. 3b [28]. This comparison is based on PP and SBP differences from the novel device to the reference device (ground truth) extracted from Bland–Altman plots. The mean values of the difference are shown in the graphs on the left, while the standard deviations (SD) of the SBP and PP differences are included in the graphs on the right. From the obtained results, we concluded that when measuring the carotid artery in a healthy young subject, the model that better approaches the ground truth is M3, with SBP and PP differences of 2.64 ± 1.79 mmHg and 0.64 ± 1.73 mmHg, respectively. However, when measuring at the brachial or radial artery, the linear model (M1) is more accurate, with SBP and PP differences of: – 0.76 ± 2.21 mmHg and – 2.85 ± 2.57 mmHg (radial); and – 0.57 ± 1.98 mmHg and – 0.57 ± 1.99 mmHg (brachial). As shown in Fig. 3b, those values are within the recommended values from the Association for the Advancement of Medical Instrumentation (AAMI).
The AAMI recommends for BP cuff devices a maximum mean difference of ± 5 mmHg and SD of ± 8 mmHg between the reference and the proof-of-concept device [33]. As seen in Fig. 3b, BP measurements of young subjects at the carotid or radial artery derived from the M2 model (exponential relationship) provide higher errors in SBP and PP than the maximum allowed by the AAMI. Surprisingly, the exponential model is still the most extended in the literature and is mostly used for BP determination when using ultrasonic devices. This may be due to its better accuracy for aged (middle and late adulthood) subjects and to the tube law employed in the 1D model, which has a profound effect on the pressure estimation. The application of other 1D models may lead to other conclusions. Thus, the validity of the proposed models M1-M3 still requires in vivo data for a better and more accurate physiological validation.
4 Proof-of-Concept Validation
The emergence of new cutting-edge technologies to continuously measure vital parameters and prevent cardiovascular risks requires the validation of proof-of-concept devices at different stages of development [34]. In vivo experiments provide the most valuable information about the performance of the device. However, they are very expensive for iterative optimizations or modifications required in the development of a new medical device [35]. Thus, before performing in vivo measurements in animals or humans, the performance of the new device needs to be demonstrated in a laboratory environment (technology readiness level 4, TRL4 [36]). Hemodynamic evaluations of flow and distension at peripheral arteries and central arteries (i.e., aorta) can be modeled in vitro by implementing mechanical MCL [37]. MCL evaluates the human cardiovascular system and offers the advantage that complications in the circulation and potential risk of cardiovascular diseases, such as atherosclerosis, stenosis, and changes in the arterial structure, can be mechanically modeled and controlled with high repeatability.
A simple MCL to measure heart rate, BP, compliance and resistance of the arteries can be composed of the following mechanical elements: pressure motor or peristaltic pump to mimic the heart function, bubble trap to remove the bubbles produced by the pump, variable valves to reduce or increase the peripheral resistance, tubes to emulate arteries, compliance chamber to simulate arterial compliance by changing the air pressure column on top, and various reservoirs. The main challenge of MCLs is the design of patient-specific mimicked arteries and tissues that possess the same characteristics as humans or animals. For this purpose, phantoms are widely used. The phantom design for validation of a new device needs to resemble the human tissue as it is seen by the wave that is going to be propagated through it. This means that if the device to be evaluated is an ultrasonic device, the phantom needs to have the same acoustic impedance, speed, and attenuation as the human tissue.
For the validation of our ultrasonic device, we tested multiple phantoms [38]. Agar, gelatin, gel–wax, and polyvinyl (PVA)-based phantoms are the most commonly used [39]. Gel–wax, agar, and gelatin phantoms are low-cost, easy, and fast to develop. However, they are not long-lasting, and their properties change very fast in time, so they can be used only for some days. As we demonstrated in [38], PVA–cryogel is the most preferred alternative for ultrasound applications due to its stability and very optimal acoustic attenuation. In addition, its mechanical and speed properties can be easily tunable by freeze-drying processes, changing concentration, or adding other chemicals. PVA can be made transparent by adding dimethyl sulfoxide, which is of high advantage when visualization of the flow in the phantom is needed. The limitation is that the viscoelastic properties of the arterial walls cannot be modeled with those phantoms. Still, the elastic modulus can be tuned with the freeze-drying process [40].
Multimodal phantoms that can be used for more than only one signal modality provide the advantage that they can be applied in MCL for the validation of various devices, or for one single device that integrates two or more sensor technologies [41].
We also used extracted arteries from animals provided by slaughterhouses instead of phantoms for a better evaluation of the ultrasonic device. In this case, we are talking about ex vivo cardiovascular setups. The advantage is that they provide a more realistic mimicking of the non-linear mechanics of the tissue.
In [17, 28], we validated in silico, in vitro, and ex vivo our newly developed US device. In young subjects, an in silico pulse pressure (PP) correlation of 0.978 and a mean difference of (– 2.85 ± 2.57) mmHg at the radial artery were achieved. At the same artery, the ex vivo PP correlation was 0.986, with a mean difference of (1.72 ± 3.29) mmHg. The next steps are being done now for the in vivo US validation.
5 Outlook
The development of new noninvasive, portable, and compact cutting-edge devices offers the possibility to continuously monitor BP comfortably and safely. Ultrasound is a technology that is widely used in clinics, is very well known, and can potentially be used to noninvasively measure vital parameters for in-home monitoring. However, limitations in power consumption, reduced accuracy affected by the arterial-site measurement, placement of the device, and the challenge of creating patient-specific algorithms to derive multiple vital parameters still require further research. New technologies can be further expanded to obtain a better penetration depth and amount of signal transmitted to the tissue. Furthermore, specific algorithms applied according to the arterial age and sex of the patient significantly improve the accuracy of BP derivation. On top of that, MCL setups using mechanical in vitro and ex vivo approaches are simplified solutions for iterative modifications and improvement of medical devices, and help emulate arterial hemodynamics and cardiovascular risk conditions before proceeding with in vivo trials.
Availability of Data and Materials
The datasets generated and/or analyzed during this review (Fig. 3) are available in Table II of this published article: A. C. Gonçalves Seabra, A. F. d. Silva, T. Stieglitz and A. B. Amado-Rey, "In Silico Blood Pressure Models Comparison," in IEEE Sensors Journal, vol. 22, no. 23, pp. 23,486–23,493, 1 Dec.1, 2022, https://doi.org/10.1109/JSEN.2022.3215597.
References
Hypertension. [Online]. Available: https://www.who.int/news-room/fact-sheets/detail/hypertension. Accessed 3 Aug 2024.
Mukherjee R, Ghosh S, Gupta B, Chakravarty T. A literature review on current and proposed technologies of noninvasive blood pressure measurement. Telemed J e-health Off J Am Telemed Assoc. 2018;24(3):185–93. https://doi.org/10.1089/tmj.2017.0068.
Pena-Hernandez C, Nugent K, Tuncel M. Twenty-four-hour ambulatory blood pressure monitoring. J Prim Care Community Health. 2020;11:2150132720940519. https://doi.org/10.1177/2150132720940519.
Miura K. Tunica intima compensation for reduced stiffness of the tunica media in aging renal arteries as measured with scanning acoustic microscopy. PLoS ONE. 2020;15(11): e0234759. https://doi.org/10.1371/journal.pone.0234759.
Azhari H. Basic of biomedical ultrasound for engineers. Appendix a: typical acoustic properties of tissues, pp. 313–314.
Wang C, et al. Monitoring of the central blood pressure waveform via a conformal ultrasonic device. Nat Biomed Eng. 2018;2(9):687–95. https://doi.org/10.1038/s41551-018-0287-x.
Sempionatto JR, et al. An epidermal patch for the simultaneous monitoring of haemodynamic and metabolic biomarkers. Nat Biomed Eng. 2021;5(7):737–48. https://doi.org/10.1038/s41551-021-00685-1.
Peng C, Chen M, Sim HK, Zhu Y, Jiang X. Noninvasive and nonocclusive blood pressure monitoring via a flexible piezo-composite ultrasonic sensor. IEEE Sens J. 2021;21(3):2642–50. https://doi.org/10.1109/JSEN.2020.3021923.
Zhang Y, Demosthenous A. Integrated circuits for medical ultrasound applications: imaging and beyond. IEEE Trans Biomed Circuits Syst. 2021;15(5):838–58. https://doi.org/10.1109/TBCAS.2021.3120886.
Wearable Technology Market Size, Share & COVID-19 Impact Analysis, By Type (Smart Glasses, VR Headsets, Smart Jackets and Smart Rings, Smart Watches, Fit Bands), By Technology (IoT Based, AR and VR, Others), By End Use (Health and Fitness, BFSI, Gaming and Entertainment, Fashion, Travel, Education, Logistics & Warehouse), and Regional Forecast, 2023–2030 | Fortune Business Insights. Accessed 28 Nov 2023.
Wang J, Zheng Z, Chan J, Yeow JTW. Capacitive micromachined ultrasound transducers for intravascular ultrasound imaging. Microsyst Nanoeng. 2020;6(1):73. https://doi.org/10.1038/s41378-020-0181-z.
Jiang X, Perrot V, Varray F, Bart S, Hartwell PG. Piezoelectric micromachined ultrasonic transducer for arterial wall dynamics monitoring. IEEE Trans Ultrason Ferroelectr Freq Control. 2022;69(1):291–8. https://doi.org/10.1109/TUFFC.2021.3120283.
Lin M, et al. A fully integrated wearable ultrasound system to monitor deep tissues in moving subjects. Nat Biotechnol. 2023. https://doi.org/10.1038/s41587-023-01800-0.
Sunwoo S-H, et al. Soft bioelectronics for the management of cardiovascular diseases. Nat Rev Bioeng. 2023. https://doi.org/10.1038/s44222-023-00102-z.
Gurun G, et al. Single-chip CMUT-on-CMOS front-end system for real-time volumetric IVUS and ICE imaging. IEEE Trans Ultrason Ferroelectr Freq Control. 2014;61(2):239–50. https://doi.org/10.1109/TUFFC.2014.6722610.
Kenny J-ÉS, et al. A novel, hands-free ultrasound patch for continuous monitoring of quantitative Doppler in the carotid artery. Sci Rep. 2021;11(1):7780. https://doi.org/10.1038/s41598-021-87116-y.
Amado-Rey AB, Seabra ACG, Becker FJ, Fournelle M, Stieglitz T. Extraction of radial-artery strain and stiffness by using noninvasive ultrasound and a low-power peak detector. IEEE Sens Lett. 2021;5(8):1–4. https://doi.org/10.1109/LSENS.2021.3096640.
Steinberg S, Huang A, Ono Y, Rajan S. Continuous artery monitoring using a flexible and wearable single-element ultrasonic sensor. IEEE Instrum Meas Mag. 2022;25(1):6–11. https://doi.org/10.1109/MIM.2022.9693453.
Frey S, Vostrikov S, Benini L, Cossettini A. WULPUS: a Wearable Ultra Low-Power Ultrasound probe for multi-day monitoring of carotid artery and muscle activity, pp. 1–4.
Nabeel PM et al. An image-free ultrasound device for simultaneous measurement of local and regional arterial stiffness indices, pp. 1–6.
Shomaji S, Basak A, Mandai S, Karam R, Bhunia S. A wearable carotid ultrasound assembly for early detection of cardiovascular diseases, pp. 17–20.
Seo J, Pietrangelo SJ, Lee H-S, Sodini CG. Noninvasive arterial blood pressure waveform monitoring using two- element ultrasound system. IEEE Trans Ultrason Ferroelectr Freq Control. 2015;62(4):776–84. https://doi.org/10.1109/TUFFC.2014.006904.
Meinders JM, Hoeks APG. Simultaneous assessment of diameter and pressure waveforms in the carotid artery. Ultrasound Med Biol. 2004;30(2):147–54. https://doi.org/10.1016/j.ultrasmedbio.2003.10.014.
Soleimani E, Mokhtari-Dizaji M, Fatouraee N, Saberi H. Assessing the blood pressure waveform of the carotid artery using an ultrasound image processing method. Ultrasonography (Seoul, Korea). 2017;36(2):144–52. https://doi.org/10.14366/usg.16019.
Athaya T, Choi S. A review of noninvasive methodologies to estimate the blood pressure waveform. Sensors (Basel, Switzerland). 2022. https://doi.org/10.3390/s22103953.
Vappou J, Luo J, Okajima K, Di Tullio M, Konofagou E. Pulse wave ultrasound manometry (PWUM): measuring central blood pressure non-invasively, pp. 2122–2125.
Vennin S, et al. Noninvasive calculation of the aortic blood pressure waveform from the flow velocity waveform: a proof of concept. Am J Physiol Heart Circ Physiol. 2015;309(5):H969–76. https://doi.org/10.1152/ajpheart.00152.2015.
Goncalves Seabra AC, Silva AF, Stieglitz T, Amado-Rey AB. In silico blood pressure models comparison. IEEE Sens J. 2022;22(23):23486–93. https://doi.org/10.1109/JSEN.2022.3215597.
Giudici A, et al. Transfer-function-free technique for the noninvasive determination of the human arterial pressure waveform. Physiol Rep. 2021;9(18): e15040. https://doi.org/10.14814/phy2.15040.
Beulen BWAMM, Bijnens N, Koutsouridis GG, Brands PJ, Rutten MCM, van de Vosse FN. Toward noninvasive blood pressure assessment in arteries by using ultrasound. Ultrasound Med Biol. 2011;37(5):788–97. https://doi.org/10.1016/j.ultrasmedbio.2011.01.020.
Vappou J, Luo J, Konofagou EE. Pulse wave imaging for noninvasive and quantitative measurement of arterial stiffness in vivo. Am J Hypertens. 2010;23(4):393–8. https://doi.org/10.1038/ajh.2009.272.
Charlton PH, Mariscal Harana J, Vennin S, Li Y, Chowienczyk P, Alastruey J. Modeling arterial pulse waves in healthy aging: a database for in silico evaluation of hemodynamics and pulse wave indexes. Am J Physiol Heart Circ Physiol. 2019;317(5):H1062–85. https://doi.org/10.1152/ajpheart.00218.2019.
ANSI/AAMI/ISO 81060-2:2019 - Non-invasive sphygmomanometers - Part 2: Clinical investigation of intermittent automated measurement type. [Online]. Available: https://webstore.ansi.org/standards/aami/ansiaamiiso810602019. Accessed 28 Nov 2023.
Gonçalves Seabra AC, Ferreira da Silva A, Stieglitz T, Belen Amado-Rey A. Preliminary validation system for cuffless blood pressure measurement. Curr Dir Biomed Eng. 2022;8(2):189–92. https://doi.org/10.1515/cdbme-2022-1049.
Xu K-W, Gao Q, Wan M, Zhang K. Mock circulatory loop applications for testing cardiovascular assist devices and in vitro studies. Front Physiol. 2023;14:1175919. https://doi.org/10.3389/fphys.2023.1175919.
Raffaini P, Manfredi L. Project management. In: Endorobotics. Elsevier; 2022. p. 337–58.
Chen D, et al. A mock circulation loop for in vitro hemodynamic evaluation of aorta: application in aortic dissection. J Endovasc Ther Off J Int Soc Endovasc Spec. 2022;29(1):132–42. https://doi.org/10.1177/15266028211034863.
Amado-Rey B, Mittnacht A, Stieglitz T. Experimental characterization of optoacoustic phantoms in gel wax and polyvinyl alcohol for blood pressure measurements. In: Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. Annual International Conference, vol. 2019, pp. 5820–5823, 2019. https://doi.org/10.1109/EMBC.2019.8857175.
Groves LA, et al. A review of low-cost ultrasound compatible phantoms. IEEE Trans Biomed Eng. 2023;70(12):3436–48. https://doi.org/10.1109/TBME.2023.3288071.
Dineley J, Meagher S, Poepping TL, McDicken WN, Hoskins PR. Design and characterisation of a wall motion phantom. Ultrasound Med Biol. 2006;32(9):1349–57. https://doi.org/10.1016/j.ultrasmedbio.2006.05.033.
Nabeel PM, Joseph J, Karthik S, Sivaprakasam M, Chenniappan M. Bi-modal arterial compliance probe for calibration-free cuffless blood pressure estimation. IEEE Trans Bio-med Eng. 2018;65(11):2392–404. https://doi.org/10.1109/TBME.2018.2866332.
Acknowledgements
This review article and the associated career development lecture at the ARTERY 23 conference in Bonn, Germany (05-07 October 2023) summarize my research on continuous BP measurement using ultrasound that has been performed at the Technical University of Freiburg, Germany. This work has been completed, thanks to the cooperation with Fraunhofer IBMT (Dr. Marc Fournelle), who provided the ultrasonic sensor. Additionally, thanks to Msc. A. C. Gonçalves Seabra for her extraordinary work performed in this project, and Annette Mittnacht for her help with the phantom characterization. This work would not have taken place without the support and encouragement of all of my colleagues at the laboratory for biomedical microtechnology and the constant guidance, knowledge, and motivation from Prof. Dr. Thomas Stieglitz, who guides our department throughout science.
Funding
Open Access funding enabled and organized by Projekt DEAL. This work was funded by the Margarethe von Wrangell-Programme (Ministry of Science, Research and Arts of Baden-Wuerttemberg, Germany). Link: http://www.margarete-von-wrangell.de/.
Author information
Authors and Affiliations
Contributions
Ana Belen Amado Rey is the full contributor of this review paper.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Ethics Approval and Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Amado Rey, A.B. Estimation of Blood Pressure by Image-Free, Wearable Ultrasound. Artery Res 30, 3 (2024). https://doi.org/10.1007/s44200-024-00048-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44200-024-00048-6