Abstract
Background
As Saudi Arabia is expected to face population aging in the future, the burden of diseases arising from inadequate physical activity (PA) and excess sedentary behavior (SB) may subsequently increase without successful interventions. The present study critically reviews the global literature on the effectiveness of PA interventions targeting community-dwelling older adults to draw on lessons and applications for future interventions in Saudi Arabia.
Methods
This umbrella review of systematic reviews included interventions designed to increase PA and/or reduce SB in community-dwelling older adults. We conducted searches in July 2022 in two electronic databases—PubMed and Embase—and identified relevant peer-reviewed systematic reviews in English.
Results
Fifteen systematic reviews focusing on community-dwelling older adults were included. Several reviews reported that PA- or SB-based interventions, including eHealth interventions (such as automated advice, tele-counseling, digital PA coaching, automated PA tracking and feedback, online resources, online social support, and video demonstrations), mHealth interventions, and non-eHealth interventions (such as goal setting, individualized feedback, motivational sessions, phone calls, face-to-face education, counseling, supervised exercise sessions, sending educational materials to participants’ homes, music, and social marketing programs), were effective in the short term (e.g., ≤ 3 months) but with wide heterogeneity in findings and methodologies. There were limited studies on PA- and SB-based interventions that could be effective for one year or more after the intervention. Most reviews were heavily skewed toward studies carried out in Western communities, limiting their generalizability to Saudi Arabia and other parts of the world.
Conclusion
There is evidence that some PA and SB interventions may be effective in the short term, but high-quality evidence regarding long-term effects is lacking. The cultural, climate, and environmental barriers related to PA and SB in Saudi Arabia require an innovative approach and research to evaluate such interventions in older individuals in the long term.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Due to improvements in health services, living conditions, and work environments, population aging has become a global phenomenon. A growing challenge is to maintain health and fitness throughout the lifespan. There is a large body of evidence showing that regular moderate or vigorous physical activity (PA) can prevent chronic disease [1], slow or reverse sarcopenia [2,3,4,5], delay declines in cardiorespiratory fitness [6], reduce the risk of falls [7, 8], and reduce all-cause mortality [9, 10]. Sedentary behavior (SB)—seated or reclining activities that utilize 1.5 or fewer metabolic equivalents [11]—is independently associated with an increased risk of all-cause mortality [12, 13], cardiovascular mortality [12], obesity [14, 15], diabetes mellitus [16, 17], poor cognitive function [18], and poor bone health [19].
Despite the apparent health benefits of engaging in PA and limiting SB, low PA and high SB have been documented in Saudi Arabia [20,21,22]. Since the number of older citizens is projected to increase dramatically in Saudi Arabia over the next several decades [23], the disease burden due to low PA and high SB will increase without successful interventions. Moreover, several studies on the impact of the COVID-19 pandemic on physical behaviors in Saudi Arabia found that PA further declined due to movement restrictions [24,25,26,27].
The World Health Organization recommends that all adults undertake 150–300 min/week of moderate-intensity or 75–150 min/week of vigorous-intensity PA, or some equivalent combination of both and reduce the time spent in SB [28, 29]. Specifically, for older adults, a varied multi-component PA program with strength training and functional balance exercise was strongly recommended [28, 29]. This is similar to recommendations by the Public Health Authority in Saudi Arabia [30] and is aligned with Saudi Vision 2030 objectives for PA and quality of life [31]. Although many initiatives by governmental entities have been implemented to increase PA among all population groups in Saudi Arabia, guidance on what interventions might increase PA and reduce SB among older adults is lacking. The focus of this effort is to review the global literature to draw on lessons and applications for initiatives that could be considered in Saudi Arabia.
2 Methods
The search protocol was developed following the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) statement [32]. We searched the PubMed and Embase databases for systematic reviews of PA, physical inactivity, and SB interventions published since January 1, 2000, with the last day of the search conducted on July 20, 2022. We searched two databases for combinations of the following title words: physical activity, physical inactivity, sedentary, older, elderly, review, and interventions.
For inclusion, we required studies to (1) include a systematic review of interventions aimed at increasing PA, reducing physical inactivity, and/or reducing SB among community-dwelling older adults, (2) include eHealth (defined as the use of information and communications technologies in health and health-related fields), mHealth (defined as the use of mobile phones and other wireless technology in health and health-related fields), or any other type of interventions, (3) be published in a peer-reviewed journal, and (4) be published in English. We excluded protocol papers, meeting abstracts, narrative reviews, scoping reviews, reviews that did not focus primarily on intervention effectiveness, reviews that assessed outcomes other than PA or SB, and reviews that targeted small subpopulations of older adults, such as those with cancer or other diseases.
Two reviewers independently screened all the titles and abstracts of studies identified in the database searches. When there was doubt about the inclusion of a study, the full text was retrieved. Thereafter, the same two reviewers assessed the full texts of potentially eligible studies. When there were disagreements, a third reviewer was consulted to finalize the full list of studies to be included in the review.
The following information was abstracted from each review: the type of intervention, the age of the participants, the type(s) of interventions, the number of studies conducted in Western countries, the main results, and the major methodological limitations of the reviewed studies. We did not perform a meta-analysis but described the findings and interpretations of the included studies.
3 Results
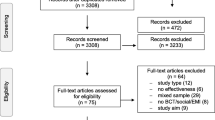
The initial searches yielded 143 reviews, of which 68 were duplicates. Of the 75 remaining records, we excluded 48 in the title- and abstract-review stage because they were not relevant for the review. We obtained and reviewed the full text of the remaining 27 records. Of these, we excluded 12 studies based on our inclusion/exclusion criteria [33,34,35,36,37,38,39,40,41,42,43,44]. We included the remaining 15 reviews [45,46,47,48,49,50,51,52,53,54,55,56,57,58,59]: five reviews of eHealth or mHealth interventions [45,46,47,48,49] and ten reviews of other intervention types [50,51,52,53,54,55,56,57,58,59]. Studies were summarized and presented into two main categories: 1) eHealth or mHealth interventions and 2) other interventions. A flowchart of our literature search is shown in Fig. 1, and a summary of the included reviews is provided in Table 1.
3.1 eHealth/mHealth Interventions
eHealth is a major focus of the PA and SB literature. Five reviews [45,46,47,48,49] assessed the effects of PA-related eHealth interventions—the interventions administered electronically. A wide range of eHealth interventions was assessed, including automated advice, tele-counseling, digital PA coaching, automated PA tracking and feedback, online resources, online social support, and video demonstrations. Many studies used more than one eHealth strategy at the same time. Some eHealth studies did not promote a specific type of PA, while others specifically aimed to increase walking, stretching, balance, and/or resistance training. Two reviews focused on mHealth interventions, such as automated messaging or use of mobile/tablet apps in combination with wearable devices.
Four of the five eHealth reviews reported similar findings [45,46,47,48], with greater PA participation in intervention groups compared to controls. For example, the meta-analysis by Kwan et al. showed that eHealth interventions were associated with a significant increase in PA time compared with the control group results (mean difference = 53.2 min/week, 95% confidence interval [CI] = 30.18–76.21) [46]. This finding is congruent with another meta-analysis that showed increases in moderate-to-vigorous PA equivalent to 52 min/week, which has been shown to have clinical health benefits [48]. A fifth review reported no significant differences between intervention and control groups concerning PA or SB [49].
All four reviews that reported significant intervention effects included a substantial number of studies that relied exclusively on self-reported PA, which correlates poorly with objectively measured PA [60,61,62,63,64]. For example, a meta-analysis of randomized controlled trials by Stockwell et al. [48] showed a positive effect of eHealth interventions on PA but, when trials that relied solely on self-reported PA were excluded, the interventions showed no effect. The one review of eHealth interventions that did not report significant intervention effects excluded studies that relied on self-reported PA or SB [49].
The four eHealth/mHealth reviews that reported significant effects were comprised mainly of studies of ≤ 3 months duration. Short-term increases in PA are unlikely to have long-term health benefits, and evidence suggests that short-term changes in health behaviors are often not sustained. For example, Elavsky et al. noted that the effects of eHealth interventions such as mobile apps, automated messaging, and online resources tended to subside or be reduced in the long term [45]. Among longer-duration studies, high-quality evidence of effectiveness was largely non-existent. Kwan et al. included 38 studies, of which only 3 tracked outcomes for 12 months or more [46]. The review by Stockwell et al. found that many studies were short-term interventions with no follow-up [48]. Muellmann et al. concluded that even though eHealth interventions could effectively promote PA in the short term for adults aged 55 years and above, evidence regarding long-term effects was lacking [47].
In summary, none of the five eHealth reviews cited any high-quality evidence of statistically significant effects of eHealth interventions for one year or beyond. Considering this, Elavsky et al. asked the question of what strategies should be used to encourage long-term use of apps and wearables, given the findings that app use may peak as early as within two weeks of initiation and that one-third of consumers abandon their wearables within 6 months [45].
3.2 Other Interventions
eHealth and mHealth interventions comprise only a portion of interventions focused on PA and SB in community-dwelling older adults. We identified 10 reviews that consisted of other types of interventions, including goal setting, individualized feedback, motivational sessions, phone calls, face-to-face education, counseling, supervised exercise sessions, sending educational materials to participants’ homes, music, and social marketing programs—“the adaptation of commercial marketing technologies to programs designed to influence the voluntary behavior of target audiences to improve their personal welfare and that of society” [54]. Given the heterogeneity of interventions and study populations among these reviews, we present each review separately.
Aunger et al. reviewed various interventions targeting SB in non-working older adults. Interventions included goal setting, individualized feedback, motivational sessions, and phone calls [50]. Although the overall quality of the reviewed studies was deemed poor and half relied solely on self-reported SB, the authors concluded that the interventions could reduce sitting time in non-working older adults by up to 53.9 min per day. Objectively measured reductions in sitting time were between 3.2% and 5.3% of waking time. The duration of studies ranged from 2 to 8 weeks, precluding conclusions about clinical relevance and long-term maintenance of effects.
Chase et al. reviewed a wide range of interventions designed to reduce SB. The interventions included face-to-face education, counseling, and supervised PA [51]. In addition, some interventions entailed sending booklets, DVDs, or other materials to patients’ homes. A meta-analysis showed small but statistically significant reductions in SB among participants in the intervention groups compared to those in the control groups (d = − 0.25, 95% CI = − 0.50, 0.00, p = 0.05). However, most studies did not use experimental designs. The studies that used experimental designs did not meet many of the criteria for internal validity, such as blinding of interventionists and assessors. In addition, these studies did not consistently or clearly report strategies to ensure treatment fidelity. Eight of seventeen studies relied on self-reported measures of SB [65,66,67,68,69,70,71,72], and only two had study durations of at least six months [72, 73]. One of the two longer-term studies relied on self-reported SB [72], while the other reported no effect on overall sedentary time [73].
Chastin et al. reviewed a variety of interventions—mainly counseling, goal setting, and education—designed to reduce SB [52]. The authors identified several biases in the reviewed studies. Among the seven studies, only one study blinded participants to allocation to the control group, leading to possible performance and reporting bias. At least two studies did not blind the assessors. Two studies relied solely on self-reported PA. One study did not report on outcomes declared in the methods section, while the prespecified outcomes were only partially reported in two studies. All the studies were relatively small, with sample sizes ranging from 38 to 98 participants. The authors concluded that it was unclear whether interventions to reduce SB were effective. The number of included studies was low, however, and the certainty of the evidence was very low to low, mainly due to inconsistency in findings and imprecision.
The review by Clark et al. had a much narrower focus: the effect of music interventions on PA [53]. The review was motivated by the evidence that listening to music while exercising can increase PA among younger adults, raising the possibility that such an intervention might also be effective among older adults. The narrative synthesis included 12 low- to moderate-quality studies. Overall, three meta-analyses did not demonstrate within-session differences between music and no-music interventions. ‘Within-session’ outcomes—the focus of 10 of the 12 reviewed studies—referred to the amount of exercise that occurred during a brief exercise session, such as the duration of stationary cycling during a cycling session or the number of steps taken during an indoor walking session. These outcomes might have little relation to overall SB or PA, as measured by the number of minutes of moderate-to-vigorous PA per day. Moreover, all but two of the reviewed studies recruited participants from residential care facilities, chronic obstructive pulmonary disease rehabilitation programs, or inpatient rehabilitation programs. The results of such studies may not be generalizable to the broader population of community-dwelling older adults.
Goethals et al. systematically reviewed social marketing interventions to promote PA and PA-related outcomes among adults aged 60 years and above [54]. Nine interventions were included in the analysis. Three relied solely on self-reported PA or PA-related outcomes [74,75,76], and one of these [76] did not compare people who received the intervention to a control group. Four measured neither PA nor SB [77,78,79,80]. One reported no significant differences across communities over 24 months for moderate-to-vigorous PA, even though the number of people attending walking sessions increased in the intervention communities [81]. Only one study—Varma et al. [82]—provided strong evidence of intervention effectiveness. This three-year study found that a community volunteering program in Baltimore (Maryland, US) increased walking activity among older female—but not male—volunteers by 1,500.3 steps per day (95% CI = 77.6, 2,922.9), which was roughly 0.75 miles in distance. According to the authors, a sample size of 702 people was fairly large, and the risk of bias was low.
Grande et al. reviewed a broad array of PA-based interventions, including general or therapeutic exercise, educational programs, PA coaching or counseling, cognitive behavioral therapies, and feedback using objective PA measures such as electronic devices, such as Fitbit [55]. Unlike most other reviews on this topic, the authors limited their analysis to randomized controlled trials that objectively measured PA, mainly through accelerometers and pedometers. Fourteen published trials were included in their analysis. Pooled estimates showed that PA-based interventions were slightly effective compared with no intervention or minimal intervention in the short term (n = 1605; standard mean difference [SMD] = 0.30; 95% CI = 0.17 to 0.43) and intermediate-term (n = 895; SMD = 0.27; 95% CI = 0.06 to 0.49). However, there were no statistically significant differences between the intervention and control groups at one year and beyond (n = 323; SMD = 0.19; 95% CI = − 0.03 to 0.41).
Merom et al. reviewed workplace PA interventions that targeted older employees [56]. The interventions involved aerobic activity, strength, balance, and/or flexibility. The results of their meta-analyses showed no significant differences between the intervention and control groups with respect to PA. The quality of the evidence in the included studies was low due to high risk of bias, high heterogeneity (inconsistency), and imprecision (all pooled CIs included 0 and were statistically non-significant).
Müller and Khoo reviewed non-face-to-face PA interventions, such as phone counseling, newsletters, and computer-tailored PA advice letters [57]. The interventions were generally effective; of 16 interventions, 14 reported significant improvements in PA. However, no studies obtained objective measures of PA.
Otmanowski and Chase reviewed primary care-based PA interventions, such as counseling, goal setting, and education [58]. The authors explained that such interventions might be expected to be effective because the participants—older adults—valued and respected their health provider’s advice and visited their physician’s office frequently throughout the year, which created opportunities for the primary care providers to deliver PA interventions. Twenty-one studies were included in the review. A pooled analysis reported a standardized mean difference effect size of 0.27 (95% CI 0.15, 0.39, p < 0.01). The authors considered this to be a small to medium effect. Most of the interventions included in this review lasted at least 6 months, and many lasted at least 12 months. Fourteen of the twenty-one studies, however, relied exclusively on self-reported measures of PA. Despite this limitation, the authors concluded that primary care providers could significantly impact the overall health of their older adult patients by providing interventions that increase PA levels.
Sansano-Nadal et al. reviewed exercise-based PA interventions such as resistance training, balance training, and walking [59]. Unlike the other reviews, they limited their analysis to studies with at least six months of post-intervention follow-up. Most of the reviewed studies measured PA using self-reports. The results showed an effect on PA at the six-month follow-up (SMD 0.30; 95% CI 0.15 to 0.44) but not at the one- and two-year follow-ups. The authors found that exercise interventions had small clinical benefits in community-dwelling older adults and that a decline in improvement could be observed after six months of the intervention cessation.
4 Discussion
This umbrella review provided an overview of evidence on PA-promoting interventions for community-dwelling older adults, with a light shed on what might be effective in promoting PA among older adults in Saudi Arabia. We summarized the results of 15 systematic reviews covering a multitude of interventions, including eHealth/mHealth (n = 5) and other interventions (n = 10). Several reviews reported that PA- or SB-based interventions were effective in the short term but with wide heterogeneity in findings and methodologies. There were limited studies on documented PA- or SB-based interventions that could be effective for one year or more after the intervention.
Overall, the reviews suggest that some interventions, including mobile apps, automated messaging, and online resources, may modestly increase PA in the short term (e.g., ≤ 3 months) [45,46,47,48, 50, 51, 54, 55, 57, 59]. There is also some evidence that interventions carried out in primary care settings, including counselling, goal setting, and education, may increase PA in the long term [58]. The overwhelming majority of studies found in the literature were conducted in Western countries (Table 1). It should not be assumed that the results of the reviewed studies are generalizable to other countries such as Saudi Arabia, which have different geographical, climate, and cultural circumstances. There is evidence of context-specific barriers to higher levels of PA among the Gulf Cooperation Council (GCC) countries—Bahrain, Kuwait, Oman, Qatar, Saudi Arabia, and the United Arab Emirates [83]. These barriers include high temperatures that limit the safety of outdoor exercise during much of the day, high levels of urbanization that promote dependence on motor vehicles rather than active transport, and some cultural barriers [83].
Our study has several potential applications for promoting PA in Saudi Arabia. The healthcare system in Saudi Arabia is undergoing a major transition, aiming to prioritize disease prevention and public health in the new model of care [84]. Given the challenges resulting from increasing rates of chronic diseases that Saudi Arabia and other GCC countries face [85], it will be necessary to make decisions on how to scale up the prevention of noncommunicable diseases even with incomplete or inconclusive evidence.
We recommend a three-pronged approach. First, given the lack of definitive evidence in the literature and the paucity of studies conducted in GCC countries, we suggest promoting low-cost interventions that theory suggests are probably effective and that have at least some evidence base in the global literature. PA- and SB-based interventions delivered to older adults in the primary care setting may be one such intervention. As discussed in the review by Otmanowski and Chase [58], there is some evidence that such interventions may have small to modest effects on increasing PA among community-dwelling older adults. The PA-promoting interventions could be relatively easily implemented in Saudi Arabia, where all citizens have free access to government-funded health services [86]. The Ministry of Health operates a network of primary health clinics that provide public health care services [87]. The Ministry’s policies can be designed to encourage the delivery of PA-based behavioral counseling in primary care, thus potentially increasing PA [88].
Second, we recommend conducting high-quality studies to build an evidence base to facilitate future decision-making. After pilot testing to identify preliminary evidence of effectiveness in short-term studies, the selected multi-component interventions should be tested for effectiveness in older Saudi populations. Such research could use a lengthy follow-up to identify whether any intervention effects are likely to be sustained. Evidence from these high-quality studies is expected to increase investments and efforts to increase PA, reduce SB, and guide evidence-driven health policy. The Saudi Vision 2030 emphasizes the key priorities for scientific research and quality of life programs [31]. The recent national research priorities included health and wellness research as one of the four top national priorities for the next decade. In addition, the use of technologies for health purposes has been extensively expanded in Saudi Arabia during the last five years [89].
Third, we suggest focusing on older adults and other age groups in parallel. PA promotion and SB reduction interventions for older adults cannot be viewed in isolation from those targeting younger age groups. The recent movement practice guidelines for Saudi Arabia recognized the need for the life-time approach to movement behavior promotion and for providing opportunities for all the age groups—from infants to older adults—to engage in the appropriate intensity movement activities [30]. The current interventions that focus on young and working age adults need to support creation of the movement culture that would facilitate implementation of the interventions promoting PA and reducing SB in community-dwelling older adults, as Saudi population ages.
One strength of this umbrella review is the large number of systematic reviews included to synthesize the evidence around interventions that aim to increase PA and reduce SB. To our knowledge, this is the first umbrella review to draw on lessons and implications from the global literature on what might be effective in promoting PA among older adults in Saudi Arabia. However, our study has some limitations that should be acknowledged. Many of the primary studies included in the reviewed sources have methodological shortcomings, such as the absence of a control group, reliance on self-reported PA and SB, failure to blind participants, failure to blind interventionists, failure to blind assessors, and/or failure to fully report on prespecified outcomes. These limitations might impact the evidence generated from these studies. Also, as noted above, the generalizability of these studies is questionable. In addition, we did not consider searching for grey literature and non-English articles. We assumed that the most reliable literature was published in English and indexed in the databases we searched. Future research might consider the grey literature and non-English studies to capture any evidence that might have been excluded from this umbrella review. Finally, we did not assess the quality of the included systematic reviews. Further studies are encouraged to address these limitations to provide solid conclusions.
5 Conclusion
In this umbrella review, we assessed the evidence of the effectiveness of interventions aiming to increase PA and/or reduce SB among community-dwelling older adults. There is some evidence that such interventions may be effective in the short term (≤ 3 months), but high-quality evidence on long-term effects is largely lacking. Most reviews were skewed heavily toward studies conducted in Western communities. In the short term, promoting promising and low-cost interventions is reasonable from a public health perspective, even if rigorous evidence of effectiveness is lacking. High-quality studies are needed to assess the validity of our findings among the Saudi population to identify cost-effective strategies to increase PA and reduce SB.
Data Availability
All data generated or analyzed during this study are included in this published article.
Abbreviations
- CI:
-
Confidence interval;
- COPD:
-
Chronic obstructive pulmonary disease;
- GCC:
-
Gulf Cooperation Council;
- PA:
-
Physical activity;
- SB:
-
Sedentary behavior
References
Warburton DER, Nicol CW, Bredin SSD. Health benefits of physical activity: the evidence. CMAJ Can Med Assoc J J Assoc Medicale Can. 2006;174:801–9. https://doi.org/10.1503/cmaj.051351.
Montero-Fernández N, Serra-Rexach JA. Role of exercise on sarcopenia in the elderly. Eur J Phys Rehabil Med. 2013;49:131–43.
Marzetti E, Calvani R, Tosato M, et al. Physical activity and exercise as countermeasures to physical frailty and sarcopenia. Aging Clin Exp Res. 2017;29:35–42. https://doi.org/10.1007/s40520-016-0705-4.
Beaudart C, Dawson A, Shaw SC, et al. Nutrition and physical activity in the prevention and treatment of sarcopenia: systematic review. Osteoporos Int J Establ Result Coop Eur Found Osteoporos Natl Osteoporos Found USA. 2017;28:1817–33. https://doi.org/10.1007/s00198-017-3980-9.
Nascimento CM, Ingles M, Salvador-Pascual A, et al. Sarcopenia, frailty and their prevention by exercise. Free Radic Biol Med. 2019;132:42–9. https://doi.org/10.1016/j.freeradbiomed.2018.08.035.
Chodzko-Zajko WJ, Proctor DN, et al. American college of sports medicine position stand. exercise and physical activity for older adults. Med Sci Sports Exerc. 2009;41:1510–30. https://doi.org/10.1249/MSS.0b013e3181a0c95c.
Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012. https://doi.org/10.1002/14651858.CD007146.pub3.
Thomas E, Battaglia G, Patti A, et al. Physical activity programs for balance and fall prevention in elderly: a systematic review. Med (Baltimore). 2019;98:16218. https://doi.org/10.1097/MD.0000000000016218.
de Rezende LFM, Rey-López JP, Matsudo VKR, et al. Sedentary behavior and health outcomes among older adults: a systematic review. BMC Public Health. 2014;14:333. https://doi.org/10.1186/1471-2458-14-333.
Mok A, Khaw K-T, Luben R, et al. Physical activity trajectories and mortality: population based cohort study. BMJ. 2019;365:l2323. https://doi.org/10.1136/bmj.l2323.
Tremblay MS, Aubert S, Barnes JD, et al. Sedentary behavior research network (SBRN) - terminology consensus project process and outcome. Int J Behav Nutr Phys Act. 2017;14:75. https://doi.org/10.1186/s12966-017-0525-8.
Matthews CE, George SM, Moore SC, et al. Amount of time spent in sedentary behaviors and cause-specific mortality in US adults. Am J Clin Nutr. 2012;95:437–45. https://doi.org/10.3945/ajcn.111.019620.
Lavie CJ, Ozemek C, Carbone S, et al. Sedentary behavior, exercise, and cardiovascular health. Circ Res. 2019;124:799–815. https://doi.org/10.1161/CIRCRESAHA.118.312669.
Thorp AA, Owen N, Neuhaus M, et al. Sedentary behaviors and subsequent health outcomes in adults a systematic review of longitudinal studies, 1996–2011. Am J Prev Med. 2011;41:207–15. https://doi.org/10.1016/j.amepre.2011.05.004.
Gennuso KP, Gangnon RE, Matthews CE, et al. Sedentary behavior, physical activity, and markers of health in older adults. Med Sci Sports Exerc. 2013;45:1493–500. https://doi.org/10.1249/MSS.0b013e318288a1e5.
Healy GN, Matthews CE, Dunstan DW, et al. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003–06. Eur Heart J. 2011;32:590–7. https://doi.org/10.1093/eurheartj/ehq451.
Proper KI, Singh AS, van Mechelen W, et al. Sedentary behaviors and health outcomes among adults: a systematic review of prospective studies. Am J Prev Med. 2011;40:174–82. https://doi.org/10.1016/j.amepre.2010.10.015.
Hamer M, Stamatakis E. Prospective study of sedentary behavior, risk of depression, and cognitive impairment. Med Sci Sports Exerc. 2014;46:718–23. https://doi.org/10.1249/MSS.0000000000000156.
Tremblay MS, Colley RC, Saunders TJ, et al. Physiological and health implications of a sedentary lifestyle. Appl Physiol Nutr Metab Physiol Appl Nutr Metab. 2010;35:725–40. https://doi.org/10.1139/H10-079.
Al-Hazzaa HM. Prevalence of physical inactivity in Saudi Arabia: a brief review. East Mediterr Health J Rev Sante Mediterr Orient Al-Majallah Al-Sihhiyah Li-Sharq Al-Mutawassit. 2004;10:663–70.
Al-Hazzaa HM. Physical inactivity in Saudi Arabia revisited: A systematic review of inactivity prevalence and perceived barriers to active living. Int J Health Sci. 2018;12:50–64.
Evenson KR, Alhusseini N, Moore CC, et al. Scoping review of population-based physical activity and sedentary behavior in Saudi Arabia. J Phys Act Heal. 2023;1:16.
Karlin NJ, Weil J, Felmban W. Aging in Saudi Arabia: an exploratory study of contemporary older persons’ views about daily life, health, and the experience of aging. Gerontol Geriatr Med. 2016;2:2333721415623911. https://doi.org/10.1177/2333721415623911.
Bakhsh MA, Khawandanah J, Naaman RK, et al. The impact of COVID-19 quarantine on dietary habits and physical activity in Saudi Arabia: a cross-sectional study. BMC Public Health. 2021;21:1487. https://doi.org/10.1186/s12889-021-11540-y.
Alfawaz H, Amer OE, Aljumah AA, et al. Effects of home quarantine during COVID-19 lockdown on physical activity and dietary habits of adults in Saudi Arabia. Sci Rep. 2021;11:5904. https://doi.org/10.1038/s41598-021-85330-2.
Abdulsalam NM, Khateeb NA, Aljerbi SS, et al. Assessment of dietary habits and physical activity changes during the full COVID-19 curfew period and its effect on weight among adults in Jeddah, Saudi Arabia. Int J Environ Res Public Health. 2021;18:8580. https://doi.org/10.3390/ijerph18168580.
Evenson KR, Alothman SA, Moore CC, et al. A scoping review on the impact of the COVID-19 pandemic on physical activity and sedentary behavior in Saudi Arabia. BMC Public Health. 2023;23:572.
World Health Organization. Physical activity. https://www.who.int/news-room/fact-sheets/detail/physical-activity. Accessed Aug 2022.
Bull FC, Al-Ansari SS, Biddle S, et al. World health organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451–62. https://doi.org/10.1136/bjsports-2020-102955.
Saudi Arabia Public Health Authority. Twenty-Four-Hour Movement Practice Guidelines for Saudi Arabia. https://faculty.ksu.edu.sa/sites/default/files/24hr_s_movement_practice_guidelines_for_saudi_arabia_1619026105.pdf (2021). Accessed Aug 2022.
Kingdom of Saudi Arabia. Homepage: The Progress & Achievements of Saudi Arabia - Vision 2030. https://www.vision2030.gov.sa/. Accessed Aug 2022.
Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. https://doi.org/10.1186/2046-4053-4-1.
McCorry MJ, Murphy MH, Bleakley C, et al. Effectiveness of physical activity and sedentary behaviour interventions in altering sedentary behaviour among older adults: a systematic review. The Lancet. 2018;392:S61. https://doi.org/10.1016/S0140-6736(18)32045-2.
Chase J-AD. Physical activity interventions among older adults: a literature review. Res Theory Nurs Pract. 2013;27:53–80. https://doi.org/10.1891/1541-6577.27.1.53.
Jonkman NH, van Schooten KS, Maier AB, et al. eHealth interventions to promote objectively measured physical activity in community-dwelling older people. Maturitas. 2018;113:32–9. https://doi.org/10.1016/j.maturitas.2018.04.010.
Lim SER, Cox NJ, Tan QY, et al. Volunteer-led physical activity interventions to improve health outcomes for community-dwelling older people: a systematic review. Aging Clin Exp Res. 2021;33:843–53. https://doi.org/10.1007/s40520-020-01556-6.
van der Bij AK, Laurant MGH, Wensing M. Effectiveness of physical activity interventions for older adults: a review. Am J Prev Med. 2002;22:120–33. https://doi.org/10.1016/s0749-3797(01)00413-5.
Taylor AH, Cable NT, Faulkner G, et al. Physical activity and older adults: a review of health benefits and the effectiveness of interventions. J Sports Sci. 2004;22:703–25. https://doi.org/10.1080/02640410410001712421.
Chase J-AD. Interventions to increase physical activity among alder adults: a meta-analysis. Gerontologist. 2015;55:706–18. https://doi.org/10.1093/geront/gnu090.
Devereux-Fitzgerald A, Powell R, Dewhurst A, et al. The acceptability of physical activity interventions to older adults: A systematic review and meta-synthesis. Soc Sci Med. 2016;158:14–23. https://doi.org/10.1016/j.socscimed.2016.04.006.
Copeland JL, Ashe MC, Biddle SJ, et al. Sedentary time in older adults: a critical review of measurement, associations with health, and interventions. Br J Sports Med. 2017;51:1539–1539. https://doi.org/10.1136/bjsports-2016-097210.
Geohagen O, Hamer L, Lowton A, et al. The effectiveness of rehabilitation interventions including outdoor mobility on older adults’ physical activity, endurance, outdoor mobility and falls-related self-efficacy: systematic review and meta-analysis. Age Ageing. 2022;51:120. https://doi.org/10.1093/ageing/afac120.
Geraedts H, Zijlstra A, Bulstra SK, et al. Effects of remote feedback in home-based physical activity interventions for older adults: a systematic review. Patient Educ Couns. 2013;91:14–24. https://doi.org/10.1016/j.pec.2012.10.018.
Shrestha N, Grgic J, Wiesner G, et al. Effectiveness of interventions for reducing non-occupational sedentary behaviour in adults and older adults: a systematic review and meta-analysis. Br J Sports Med. 2019;53:1206–13. https://doi.org/10.1136/bjsports-2017-098270.
Elavsky S, Knapova L, Klocek A, et al. Mobile health interventions for physical activity, sedentary behavior, and sleep in adults aged 50 years and older: a systematic literature review. J Aging Phys Act. 2019;27:565–93. https://doi.org/10.1123/japa.2017-0410.
Kwan RYC, Salihu D, Lee PH, et al. The effect of e-health interventions promoting physical activity in older people: a systematic review and meta-analysis. Eur Rev Aging Phys Act. 2020;17:7. https://doi.org/10.1186/s11556-020-00239-5.
Muellmann S, Forberger S, Möllers T, et al. Effectiveness of eHealth interventions for the promotion of physical activity in older adults: a systematic review. Prev Med. 2018;108:93–110. https://doi.org/10.1016/j.ypmed.2017.12.026.
Stockwell S, Schofield P, Fisher A, et al. Digital behavior change interventions to promote physical activity and/or reduce sedentary behavior in older adults: a systematic review and meta-analysis. Exp Gerontol. 2019;120:68–87. https://doi.org/10.1016/j.exger.2019.02.020.
Yerrakalva D, Yerrakalva D, Hajna S, et al. Effects of mobile health app interventions on sedentary time, physical activity, and fitness in older adults: systematic review and meta-analysis. J Med Internet Res. 2019;21:14343. https://doi.org/10.2196/14343.
Aunger JA, Doody P, Greig CA. Interventions targeting sedentary behavior in non-working older adults: a systematic review. Maturitas. 2018;116:89–99. https://doi.org/10.1016/j.maturitas.2018.08.002.
Chase J-AD, Otmanowski J, Rowland S, et al. A systematic review and meta-analysis of interventions to reduce sedentary behavior among older adults. Transl Behav Med. 2020;10:1078–85. https://doi.org/10.1093/tbm/ibz189.
Chastin S, Gardiner PA, Harvey JA, et al. Interventions for reducing sedentary behaviour in community-dwelling older adults. Cochrane Database Syst Rev. 2021;6:12784. https://doi.org/10.1002/14651858.CD012784.pub2.
Clark I, Taylor N, Baker F. Music interventions and physical activity in older adults: a systematic literature review and meta-analysis. J Rehabil Med. 2012;44:710–9. https://doi.org/10.2340/16501977-1025.
Goethals L, Barth N, Hupin D, et al. Social marketing interventions to promote physical activity among 60 years and older: a systematic review of the literature. BMC Public Health. 2020;20:1312. https://doi.org/10.1186/s12889-020-09386-x.
Grande GD, Oliveira CB, Morelhão PK, et al. Interventions promoting physical activity among older adults: a systematic review and meta-analysis. Gerontologist. 2020;60:e583–99. https://doi.org/10.1093/geront/gnz167.
Merom D, Stanaway F, Gebel K, et al. Supporting active ageing before retirement: a systematic review and meta-analysis of workplace physical activity interventions targeting older employees. BMJ Open. 2021;11:e045818. https://doi.org/10.1136/bmjopen-2020-045818.
Müller AM, Khoo S. Non-face-to-face physical activity interventions in older adults: a systematic review. Int J Behav Nutr Phys Act. 2014;11:35. https://doi.org/10.1186/1479-5868-11-35.
Otmanowski JA, Chase J-AD. Systematic review and meta-analysis of primary care-based physical activity interventions among older adults. J Aging Phys Act. 2022;1:1–15. https://doi.org/10.1123/japa.2021-0111.
Sansano-Nadal G-G, et al. Exercise-based interventions to enhance long-term sustainability of physical activity in older adults: a systematic review and meta-analysis of randomized clinical trials. Int J Environ Res Public Health. 2019;16:2527. https://doi.org/10.3390/ijerph16142527.
Colley RC, Butler G, Garriguet D, et al. Comparison of self-reported and accelerometer-measured physical activity in Canadian adults. Health Rep. 2018;29:3–15.
Colley RC, Butler G, Garriguet D, et al. Comparison of self-reported and accelerometer-measured physical activity among Canadian youth. Health Rep. 2019;30:3–12.
Ekelund U, Tomkinson G, Armstrong N. What proportion of youth are physically active? Measurement issues, levels and recent time trends. Br J Sports Med. 2011;45:859–65. https://doi.org/10.1136/bjsports-2011-090190.
Jacobs DR, Ainsworth BE, Hartman TJ, et al. A simultaneous evaluation of 10 commonly used physical activity questionnaires. Med Sci Sports Exerc. 1993;25:81–91. https://doi.org/10.1249/00005768-199301000-00012.
Taber DR, Stevens J, Murray DM, et al. The effect of a physical activity intervention on bias in self-reported activity. Ann Epidemiol. 2009;19:316–22. https://doi.org/10.1016/j.annepidem.2009.01.001.
Chang AK, Fritschi C, Kim MJ. Sedentary behavior, physical activity, and psychological health of Korean older adults with hypertension: effect of an empowerment intervention. Res Gerontol Nurs. 2013;6:81–8. https://doi.org/10.3928/19404921-20121219-01.
Maher JP, Sliwinski MJ, Conroy DE. Feasibility and preliminary efficacy of an intervention to reduce older adults’ sedentary behavior. Transl Behav Med. 2017;7:52–61. https://doi.org/10.1007/s13142-016-0394-8.
White I, Smith L, Aggio D, et al. On Your Feet to Earn Your Seat: pilot RCT of a theory-based sedentary behaviour reduction intervention for older adults. Pilot Feasibility Stud. 2017;3:23. https://doi.org/10.1186/s40814-017-0139-6.
Ory MG, Lee S, Han G, et al. Effectiveness of a lifestyle intervention on social support, self-efficacy, and physical activity among older adults: evaluation of Texercise Select. Int J Environ Res Public Health. 2018;15:E234. https://doi.org/10.3390/ijerph15020234.
Britten L, Addington C, Astill S. Dancing in time: feasibility and acceptability of a contemporary dance programme to modify risk factors for falling in community dwelling older adults. BMC Geriatr. 2017;17:83. https://doi.org/10.1186/s12877-017-0476-6.
Matei R, Thuné-Boyle I, Hamer M, et al. Acceptability of a theory-based sedentary behaviour reduction intervention for older adults ('On Your Feet to Earn Your Seat’). BMC Public Health. 2015;15:606. https://doi.org/10.1186/s12889-015-1921-0.
Toto PE, Raina KD, Holm MB, et al. Outcomes of a multicomponent physical activity program for sedentary, community-dwelling older adults. J Aging Phys Act. 2012;20:363–78. https://doi.org/10.1123/japa.20.3.363.
Burke L, Lee AH, Jancey J, et al. Physical activity and nutrition behavioural outcomes of a home-based intervention program for seniors: a randomized controlled trial. Int J Behav Nutr Phys Act. 2013;10:14. https://doi.org/10.1186/1479-5868-10-14.
Fanning J, Porter G, Awick EA, et al. Effects of a DVD-delivered exercise program on patterns of sedentary behavior in older adults: a randomized controlled trial. Prev Med Rep. 2016;3:238–43. https://doi.org/10.1016/j.pmedr.2016.03.005.
Kamada M, Kitayuguchi J, Abe T, et al. Community-wide intervention and population-level physical activity: a 5-year cluster randomized trial. Int J Epidemiol. 2018;47:642–53. https://doi.org/10.1093/ije/dyx248.
Reger-Nash B, Bauman A, Cooper L, et al. Evaluating communitywide walking interventions. Eval Program Plann. 2006;29:251–9. https://doi.org/10.1016/j.evalprogplan.2005.12.005.
Russell C, Oakland MJ. Nutrition education for older adults: The Chef Charles Club. J Nutr Educ Behav. 2007;39:233–4. https://doi.org/10.1016/j.jneb.2007.01.014.
DiGuiseppi CG, Thoreson SR, Clark L, et al. Church-based social marketing to motivate older adults to take balance classes for fall prevention: cluster randomized controlled trial. Prev Med. 2014;67:75–81. https://doi.org/10.1016/j.ypmed.2014.07.004.
Withall J, Jago R, Fox KR. The effect a of community-based social marketing campaign on recruitment and retention of low-income groups into physical activity programmes - a controlled before-and-after study. BMC Public Health. 2012;12:836. https://doi.org/10.1186/1471-2458-12-836.
Matsudo V, Matsudo S, Andrade D, et al. Promotion of physical activity in a developing country: the Agita São Paulo experience. Public Health Nutr. 2002;5:253–61. https://doi.org/10.1079/phn2001301.
Richert ML, Webb AJ, Morse NA, et al. Move More Diabetes: using Lay Health Educators to support physical activity in a community-based chronic disease self-management program. Diabetes Educ. 2007;33(Suppl 6):179S-184S. https://doi.org/10.1177/0145721707304172.
Wilson DK, Van Horn ML, Siceloff ER, et al. The results of the ‘Positive Action for Today’s Health’ (PATH) trial for increasing walking and physical activity in underserved African-American communities. Ann Behav Med Publ Soc Behav Med. 2015;49:398–410. https://doi.org/10.1007/s12160-014-9664-1.
Varma VR, Tan EJ, Gross AL, et al. Effect of community volunteering on physical activity: a randomized controlled trial. Am J Prev Med. 2016;50:106–10. https://doi.org/10.1016/j.amepre.2015.06.015.
Nash EA, Critchley JA, Pearson F, et al. A systematic review of interventions to promote physical activity in six Gulf countries. PLoS ONE. 2021;16:e0259058. https://doi.org/10.1371/journal.pone.0259058.
Chowdhury S, Mok D, Leenen L. Transformation of health care and the new model of care in Saudi Arabia: Kingdom’s Vision 2030. J Med Life. 2021;14:347–54.
Salem V, AlHusseini N, Abdul Razack HI, et al. Prevalence, risk factors, and interventions for obesity in Saudi Arabia: A systematic review. Obes Rev Off J Int Assoc Study Obes. 2022;23:13448. https://doi.org/10.1111/obr.13448.
Al Asmri M, Almalki MJ, Fitzgerald G, et al. The public health care system and primary care services in Saudi Arabia: a system in transition. East Mediterr Health J Rev Sante Mediterr Orient Al-Majallah Al-Sihhiyah Li-Sharq Al-Mutawassit. 2020;26:468–76.
Al Saffer Q, Al-Ghaith T, Alshehri A, et al. The capacity of primary health care facilities in Saudi Arabia: infrastructure, services, drug availability, and human resources. BMC Health Serv Res. 2021;21:365. https://doi.org/10.1186/s12913-021-06355-x.
Alahmed Z, Lobelo F. Physical activity promotion in Saudi Arabia: A critical role for clinicians and the health care system. J Epidemiol Glob Health. 2018;7(Suppl 1):S7-15. https://doi.org/10.1016/j.jegh.2017.10.005.
Alessy SA, Alattas M, Mahmoud MA, et al. Population health data in KSA: Status, challenges, and opportunities. J Taibah Univ Med Sci. 2022. https://doi.org/10.1016/j.jtumed.2022.06.011.
Acknowledgements
The paper was produced by the King Faisal Specialist Hospital and Research Center in collaboration with technical support from the World Bank. The authors are grateful for the overall support provided by Rekha Menon, World Bank Practice Manager, Health Nutrition and Population, Middle East and North Africa region, and Issam Abousleiman, World Bank Country Director for GCC countries. The authors are also grateful for the support in literature search and screening provided by Ratna Singh. The findings, interpretations, and conclusions expressed in this work are those of the authors and do not necessarily reflect the views of the King Faisal Specialist Hospital and Research Center, or the World Bank, their Boards of Directors, or the governments they represent.
Funding
Funding was provided by Saudi Ministry of Finance under the World Bank reimbursable advisory service (project number P179873).
Author information
Authors and Affiliations
Contributions
CHH, SAA, and HMA-H had the idea for the article. All authors contributed to the study conception and design. JDM, EAF, SAA, and KRE performed the literature search. JDM, EAF, SAA, and KRE extracted and analyzed data. JDM, EAF, SAA, and SR drafted the manuscript. HMA-H, VC, RAA, and BAB critically revised the work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no competing interests to declare that are relevant to the content of this article.
Ethical Approval and Consent to PArticipate
Not applicable.
Consent for Publication
Not applicable.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alessy, S.A., Malkin, J.D., Finkelstein, E.A. et al. Effectiveness of Interventions Promoting Physical Activity and Reducing Sedentary Behavior in Community-Dwelling Older Adults: An Umbrella Review With Application to Saudi Arabia. J Epidemiol Glob Health 13, 361–373 (2023). https://doi.org/10.1007/s44197-023-00111-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44197-023-00111-6