Abstract
Background
Recurrent urinary tract infection (UTI) occurs in sizable percentages of patients after a single episode and is a frequent cause of primary healthcare visits and hospital admissions, accounting for up to one quarter of emergency department visits. We aim to describe the pattern of continuous antibiotic prophylaxis prescription for recurrent urinary tract infections, in what group of adult patients they are prescribed and their efficacy.
Methods
A retrospective chart review of all adult patients diagnosed with single and recurrent symptomatic urinary tract infection in the period of January 2016 to December 2018.
Results
A total of 250 patients with a single UTI episode and 227 patients with recurrent UTI episodes were included. Risk factors for recurrent UTI included diabetes mellitus, chronic renal disease, and use of immunosuppressive drugs, renal transplant, any form of urinary tract catheterization, immobilization and neurogenic bladder. E. coli infections were the most prevalent organism in patients with UTI episodes. Prophylactic antibiotics were given to 55% of patients with UTIs, Nitrofurantoin, Bactrim or amoxicillin clavulanic acid. Post renal transplant is the most frequent reason to prophylaxis antibiotics (44%). Bactrim was more prescribed in younger patients (P < 0.001), in post-renal transplantation (P < 0.001) and after urological procedures (P < 0.001), while Nitrofurantoin was more prescribed in immobilized patients (P = 0.002) and in patients with neurogenic bladder (P < 0.001). Patients who received continuous prophylactic antibiotics experienced significantly less episodes of urinary tract infections (P < 0.001), emergency room visits and hospital admissions due to urinary tract infections (P < 0.001).
Conclusion
Despite being effective in reducing recurrent urinary tract infection rate, emergency room visits and hospital admissions due to UTI, continuous antibiotic prophylaxis was only used in 55% of patients with recurrent infections. Trimethoprim/sulfamethoxazole was the most frequently used prophylactic antibiotic. Urology and gynecological referral were infrequently requested as part of the evaluation process for patients with recurrent UTI. There was a lack of use of other interventions such as topical estrogen in postmenopausal women and documentation of education on non-pharmacological methods to decrease urinary tract infections.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Urinary tract is a leading site of infections in all ages and genders. It is prevalent as a community and healthcare related infections and affects both immunocompetent and immunocompromised hosts [1,2,3,4]. The highest prevalence is among women, with at least one episode of urinary tract infection (UTI) affecting up to 50% of females in their lifetime [5]. Urinary tract infections are frequent causes of primary healthcare visits and hospital admissions, accounting for up to one quarter of emergency department visits especially in certain high-risk groups [6,7,8,9]. The overall prevalence of uncomplicated urinary tract infection in USA is between 8 and 11% [7, 8, 10] while that of women over age of 65 is 20%. In Saudi Arabia, prevalence of urinary tract infection ranges from 9.8 to 24% in some publications [11,12,13] but no national estimation is available.
Recurrent urinary tract infection, defined as the occurrence of three episodes of UTIs in 12 months or two episodes in 6 months incidence may be as high as 44% [6, 9, 10, 14]. After a first episode of an uncomplicated urinary tract infection, at least one second episode will occur in 27% of women in the next 6–12 months [5]. Risk factors for recurrences includes history of childhood UTI [odds ratio (OR = 6.8)] back-to-front douching/wiping after bowel movement (OR = 2.6), younger age at first intercourse (OR = 6.3), increased frequency of sexual intercourse (OR = 4.8), obstructed urinary flow (OR = 1.9), and genital prolapse (OR = 3.4) and lower Vitamin D level [15, 16]
Prevention of recurrent UTIs includes continuous and postcoital antimicrobial prophylaxis and the use of topical estrogen in postmenopausal women [17,18,19,20,21]. Antimicrobial regimens commonly used for continuous antimicrobial prophylaxis include Bactrim, Fosfomycin and Nitrofurantoin. Less frequently used medications include first generation cephalosporin Cephalexin and Amoxicillin/clavulanic acid.
The prescription patterns of continuous antimicrobial prophylaxis in children and adults are not well described in Saudi patients. Barry et al. reported on status of long-term antibiotic prophylaxis for urinary tract infections in children including 34 RCTs, 9 systematic reviews, and 3 guidelines with no reference to any literature from Saudi Arabia [20]. We seek to describe the pattern of antibiotic prescription, type, duration, prescribers and in what group of patients, in adults’ Saudi patients with recurrent urinary tract infection and to assess how effective the treatment were compared to those who were not given continuous prophylaxis.
2 Method
The study was conducted at King Abdulaziz Medical City, National Guard-Health affairs (NGHA), Riyadh. This is one the major tertiary care medical cities in Saudi Arabia where it is estimated that more than a 100,000 patient visits occur annually in Outpatient department (OPD).
Electronic heath record (BESTCare system) review was retrospectively performed searching all patients age 18 years or older with at least one episode of symptomatic urinary tract infection from January 2016 to December 2018. Only outpatient visits were included. We excluded patients who are pregnant at the time of UTI diagnosis. All patients should have a minimum 12 months of follow-up after the first diagnosis of UT.
Patients were then grouped into those with single urinary tract infection during the follow-up of one year from initial episode and those with recurrent infections. Recurrent urinary tract infection is defined as either ≥ 3 symptomatic episodes with positive urinary cultures per year or ≥ 2 symptomatic episodes with positive urinary cultures in the last 6 months. Patients who were started on continuous prophylactic antibiotics were identified from the group with urinary tract infection. In those patients, a minimum follow-up of 12 months post completion of the antibiotic regimens was required.
The following data were collected; patients demographics (age, gender, BMI, and social status), date of a first symptomatic positive culture of UTI episode, presence of symptoms (dysuria, fever, flank pain, etc.), UTI risk factors (renal transplant, neurogenic bladder, and vesicoureteral reflux, etc.), antibiotic prophylaxis used (Nitrofurantoin, Augmentin, First-generation cephalosporin, Ampicillin, Amoxicillin, Fosfomycin, Trimethoprim, and Bactrim), antibiotic prophylaxis start and completion dates, a number of visits while on antibiotic prophylaxis, number of UTI while on antibiotic prophylaxis and in the follow-up period, and antibiotic prophylaxis compliance documentation.
3 Data Analysis
The data was analyzed by Statistical Package for Social Sciences (SPSS software version 25). Categorical data (e.g., gender, and comorbidities) was presented by frequencies and percentages. Continuous variables such as age was presented by means and standard deviation. Descriptive and inferential statistics have been performed for the socio-demographic and clinical variables. The categorical variables were compared using a chi-square test or Fisher’s exact test, as appropriate. All tests were two-tailed, and significance was accepted at a p-value < 0.05.
4 Results
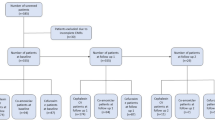
A total of 477 patients with at least one symptomatic with a positive urine culture were seen in outpatient department (OPD) in the period between January 2016 and December 2018 (Fig. 1). There were 250 patients with a documented single UTI episode and 227 patients with recurrent UTI episodes during the study period (Table 1). The mean age of all patients with urinary tract infections was 57 ± 20.5 and with a mean body mass index (BMI) of 29.6 ± 10.3. Those with recurrent UTIs were significantly older with a mean age of 60.6 ± 21.54 vs 53.6 ± 19.1 (p < 0.001) (Table 1).
More than two third of UTI patients were female, 317 (66.5%), of whom 62 (19.6%) are single. Recurrent UTI occurred in (n = 148, 46.7%) females while 169 (53.3%) had a single episode. Out of the 224 married females with urinary tract infections, (n = 125, 55.8%) had single episodes and (n = 99, 44.2%) had recurrent UTI (P = 0.75). First urinary tract infection occurred at pre-menopausal in 136 patients (42.9%) and in the post-menopause in 131 patients (41.3%). In patients with recurrent urinary tract infections, first episode of infections more frequently occurred at post-menopause (P < 0.001) (Table 1).
The most frequently documented comorbidities in patients with urinary tract infections were hypertension, in 272 patients (57%), diabetes mellitus in 217 patients (45.5%) and chronic renal disease in 122 (25.6%) patients (Table 1). Comorbidities significantly associated with risk of recurrent urinary tract infections included, Diabetes, Hypertensions, Chronic renal disease, Use of immunosuppressive medications including steroids and biological drugs, heart failure and mental health illness (Table 1). Only Chronic renal disease and mental illness were associated with recurrent UTI in multivariate analysis (Table 2).
Risk factors of urinary tract infections that poses increase risk of recurrent infections included history of urinary incontinence, renal transplantation, recent indwelling or intermittent urinary catheterization, urological procedures, immobilization and neurogenic bladder were all associated with risk of recurrent urinary tract infection (Table 2).
The most common uropathogens isolated in urinary culture were E. coli, 233 patients (49%), Klebsiella pneumoniae, 102 patients (21%), and Enterococcus faecalis, 44 patients (9.2%) (Table 1). E. coli infections was the most prevalent organism in both patients who have single episode and recurrent UTI episodes. Streptococcus agalactiae was more significantly associated with single UTI episode (p = 0.006).
At least one course of continuous prophylactic antibiotics was prescribed in 125 patients, 55 (44%) of those were post-renal transplant patients. In the post-renal transplant group, 17 patients (31%) were given prophylactic antibiotic after a single episode of UTI and 39 patients (71%) were given continuous prophylaxis after multiple UTI episodes. There were 10 other patients who received continuous antibiotic prophylaxis course after a single episode of UTI, mainly in patients with chronic urinary tract catheterization, neurogenic bladder and vesicoureteral reflux disease.
Antibiotic prophylaxis was not given in 102 (45%) patients with recurrent UTI (Table 3). The mean age of those not receiving prophylactic was significantly older, 67.2 ± 20.1 vs 55 ± 21 (p < 0.001). Patients above age of 65 were less likely to receive prophylaxis (p < 0.001). Renal transplantation, history of urological procedures, intermittent urinary catheterization and neurogenic bladder were all significantly associated with decision to use continuous prophylaxis antibiotics while immobilization was significantly associated with avoiding the use of prophylaxis therapy (Table 3). The mean number of UTI episodes in patients who did not receive antibiotics prophylaxis was (4.7 ± 3.5) episodes vs (3.3 ± 3.1) episodes in those who received antibiotics (P < 0.001).
The most frequently used antibiotic prophylaxis for those prescribed a prophylaxis antibiotic was oral trimethoprim/sulfamethoxazole (TMP-SMX), prescribed for 65 patients (52%) followed by oral Nitrofurantoin, prescribed for 52 patients (41.6%). Amoxicillin/clavulanic acid was prescribed in eight patients only (6.4%). The mean duration of antibiotics prophylaxis was (128 ± 58) days for Bactrim, (93 ± 46) days for Nitrofurantoin and (58 ± 42) days for Amoxicillin/clavulanic acid. The most frequent first prescribers for prophylaxis antibiotics were nephrologist followed by urologist and infectious disease specialist. Prophylactic antibiotics were prescribed more in renal transplant patients (P < 0.001), neurogenic bladder patients (P < 0.001) and those with urological pathology (P < 0.001).
TMP-SMX was more prescribed in younger patients, (49 ± 18.8 vs 63.4 ± 21.5), P < 0.001), in post- renal transplantation (P < 0.001) and after urological procedures (P < 0.001), while Nitrofurantoin was more prescribed in immobilized patients (P = 0.002) and in patients with neurogenic bladder (P < 0.001) (Table 4). TMP-SMX was prescribed significantly more for recurrent UTI occurring in the pre-menopausal period.
Patients who received continuous prophylactic antibiotics experienced significantly less symptomatic episodes of urinary tract infections (P < 0.001), Emergency room visits and hospital admissions due to urinary tract infections (P < 0.001) for both Nitrofurantoin and TMX-SMX. (Tables 5, 6).
There was no documentation on any education given to patients with UTI or recurrent UTI in regard to how to avoid recurrent infections. Referral for Gynecological evaluation was requested for 44 female patients (20%) with recurrent UTI, of whom 11 (25%) and 27 (61%) were pre-menopausal and postmenopausal, respectively.
Urology referral was requested in 80 female patients with recurrent UTI (35.2%); 19 patients (23.7%) and 20 patients (25%) were pre-menopausal and postmenopausal, respectively.
Urological evaluation was requested for 36 male patients (45.6%) with recurrent UTI (45.6%). Male gender with recurrent urinary tract infections were more frequently referred to Urology clinic compared to female gender (P = 0.042).
5 Discussion
This study explores a very complex and common problem in medical practice in Saudi Arabia, which is recurrent urinary tract infection. One relevant previous study in adults explored host-related risk factors for recurrent urinary tract infection in Saudi women of childbearing age but did not elaborate on management strategies used [15]. We described the risk factors and the use of antibiotic prophylaxis in patients with recurrent UTI in Saudi Arabia. We showed that old age, female gender and comorbidities (diabetes, indwelling urinary catheterization, immobilization, neurogenic bladder and renal transplantation) were associated with recurrent urinary tract infection. The use of antibiotic prophylaxis was associated with a reduction in the number of episodes of urinary tract infection and a decrease in the emergency room visits and hospitalization for UTI. The identified risk factors for recurrent UTI in our study were similar to previous studies nationally and internationally [15, 22,23,24,25].
Being conducted in a tertiary care center, almost half of patients who received antibiotic prophylaxis for recurrent UTI were renal transplants, in addition to patients with neurogenic bladder, bladder flow obstruction and intermittent catheterization. This population sitting may explain the higher percentage of male patients with recurrent urinary tract infections in our study compared to other studies conducted in the primary care setting [22, 25,26,27]. Our results are useful to improve the care of patients with recurrent UTI in tertiary care centers being common and affecting patients with different comorbidities but may not be applicable for pre-menopausal healthy female patients in the primary care setting to. The efficacy of antibiotic prophylaxis in patients with recurrent UTI is conflicting in various studies while some studies showed more harm than benefit is noted in view of development of resistant pathogens and Clostridium Difficile associated diarrhea, other studies showed efficacy in preventing recurrent urinary tract infections in patients with intermittent catheterization [28,29,30].
Only half of patients with recurrent UTI were prescribed prophylaxis antibiotics. These patients were transplant recipients, with neurogenic bladder and intermittent catheterization. Although we showed a reduction of recurrent UTI in patients who received antibiotic prophylaxis, our sample size was not powered to assess the group of patients that would benefit significantly from antibiotic prophylaxis. Both TMP-SMX and Nitrofurantoin were used effectively to prevent recurrent UTI in our study. It is not clear whether the practice of choosing one antibiotic over the other was based on patient characteristics, pathogen resistance pattern or physician versus patient preference. Fosfomycin was not used in our study in view of unavailability. Future studies are needed to evaluate the practice of various antibiotic options used as prophylaxis for recurrent UTI with emphasis on emerging bacterial resistance.
We noted that only one third of patients with recurrent UTI were referred for urological and gynecological evaluation in our study. In addition, the use of vaginal estrogen cream in postmenopausal female patients with recurrent UTI is limited. The concept of using antibiotic prophylaxis in preventing recurrent UTI without urological and gynecological review in our study is an indicator for the urgent need to develop a multi-disciplinary care for patients with recurrent UTI especially in the era of increasing bacterial resistance in tertiary care centers.
Patients with recurrent urinary tract infection in our cohort were significantly older more than those with single episode which is consistent with other report from Saudi showing recurrence UTI more frequent in those above age of 65 years [15] and international literature showing increasing prevalence of 20% with in women who are 65 years and older [15, 21, 31].
Although recurrent UTI is more frequent among females occurring in 65.2% of our sample population, more than one third (34%) of recurrent urinary tract infections episodes in this patient’s population occurred in males. This is higher than what is found by Ahmad eta al who reported retrospectively in 19,696 adults in that 20% of adults with recurrent urinary tract infections were male [31]. Our patient’s population are from a tertiary care hospital outpatient clinic compared to a community set up in the previous reference and a much smaller number in our study, all of which may explain the prevalence difference in male patients. Recurrent urinary tract infections are not infrequent in male patients however; but still occur far less than female patients. Around 14% of men will experience at least one UTI in their lifetime, compared with approximately 50% of women. Prevalence of urinary tract infection increase in male above age of 85 and 15% of those with UTI will have recurrent infection. Recurrent urinary tract infections in male are more likely related to prostatic hypertrophy and diabetes both of which lead to high post-void residuals [32, 33] The mean age of our male patients with recurrent UTI was (64.6 ± 22.5) years.
Risk factors for recurrent urinary tract infection included diabetes, indwelling urinary catheterization, immobilization, neurogenic bladder and renal transplantation and are all consistent with what is previously reported [22, 23, 25, 34]. Because of increased risk of recurrent UTI in post-transplant especially in the first few months’ post-transplant [25], many physicians elected to start prophylaxis therapy even before the first episode or after a single episode of urinary tract infection in this population. Among all the risk factors, we found that renal transplant patients had a high rate of antibiotic prophylaxis prescription despite having a single UTI episode in our cohort.
Over all Trimethoprim-Sulfamethoxazole was the most frequently used prophylaxis antibiotic in both men and women although Nitrofurantoin is still used more frequently in our patients compared to other studies specially in male (18% vs 31%) [31]. TMP-SMX is also the most prescribed antibiotic prophylaxis in post-renal transplant adult patients compared to Nitrofurantoin (P = 0.019). At the time of this study, Fosfomycin was not present in our formulary list which can explains the low use of this drug.
Both Nitrofurantoin and TMP-SMX were effective in reducing number of symptomatic urinary tract infections, admissions to hospital and ER visits due to UTI in our patients. Similar results were found by Philipp Jent et al. who conducted a systematic review and meta-analysis of published randomized controlled trials and concluded that continuous prophylactic antibiotics are effective in reducing recurrent infections irrespective of the antibiotics used [35]. Continuous antibiotic prophylaxis was also is effective in reducing recurrent UTI in patients who use clean intermittent self-catheterization [36]. Antibiotics regimens used included Nitrofurantoin, trimethoprim and Bactrim resulted in close to 50% reduction in the rate of UTI episodes.
The benefit continuous prophylaxis antibiotics in elderly patients was studied previously with conflicting results. Some studies showed increased risk of harm due to resistant organisms and Clostridioides difficile infection [37] while antibiotic prophylaxis was associated with an average of 50% reduction in UTI in men and women above age of 65 in others [31]. In this study, there were 42 patients above age of 65 years who received continuous prophylaxis. Nitrofurantoin was more frequently used in this patient population (64.3% vs 35.7%).
Our results show a low prescription of topical estrogen as a preventative measure for recurrent UTI in postmenopausal women. Out of 227 patients with recurrent UTI only 7 patients (3.1%) were prescribed topical estrogen. The lack of referrals to the gynecological department in our data correlates with the low prescription of topical estrogen. This contraindicates with recent studies proving that topical estrogen is an effective conservative treatment of recurrent UTI in postmenopausal women [38, 39].
Chang et al. prioritized topical estrogen as a first line treatment for postmenopausal women with recurrent UTI [39].
Measures other than antibiotic prophylaxis have been proposed to be just as effective as prophylactic antibiotics. Harding et al. proposed that Methenamine Hippurate is not inferior to antibiotic prophylaxis in terms of UTI prevention as it showed comparable efficacy, as well as it negates the risk of antimicrobial resistance [40]. Those measures were rarely used or documented as part of alternatives for our patients.
The main limitation of our study is being single center and retrospective in nature with selection bias. In addition, the lack of antibiotic susceptibility patterns of bacterial isolates of UTI is a major limitation of our study. Our main strength is the detailed evaluation of risk factors of recurrent UTI in relation to the use of antibiotic prophylaxis.
6 Conclusion
Urinary tract infection and recurrent UTI are common problems in outpatient’s visits especially in postmenopausal women. About one third of patients with recurrent UTI are male. Continuous antibiotic prophylaxis was only used in about half of recurrent UTI patients with TMP-SMX being the most frequently used. It was effective in reducing recurrence rate, ER visits and hospital admissions due to recurrent UTI. Urology and gynecological referral were infrequently requested as part of the evaluation process for patients with recurrent UTI. There was a lack of use of other interventions such as topical estrogen in postmenopausal women. The overall process of caring of patients with recurrent UTI lacks adequate documentations and focus on individuals’ preference rather than an organized systematic approach.
Data Availability
Not available.
Abbreviations
- UTI:
-
Urinary tract infection
- OP:
-
Odds ratio
- RCTs:
-
Randomized clinical trials
- NGHA:
-
National Guard-Health affairs
- OPD:
-
Outpatient clinic
- BMI:
-
Body mass index
- SPSS:
-
Statistical Package for Social Sciences
- TMP-SMX:
-
Trimethoprim/sulfamethoxazole
- ER:
-
Emergency room ER
References
Turner D, et al. Cost effectiveness of management strategies for urinary tract infections: results from randomised controlled trial. Bmj. 2010;340:c346. https://doi.org/10.1136/bmj.c346
Spencer JD, Schwaderer A, McHugh K, Hains DS. Pediatric urinary tract infections: an analysis of hospitalizations, charges, and costs in the USA. Pediatr Nephrol. 2010;25(12):2469–75. https://doi.org/10.1007/s00467-010-1625-8.
François M et al. The economic burden of urinary tract infections in women visiting general practices in France: a cross-sectional survey. BMC Health Ser Res. 2016;16(a):365. https://doi.org/10.1186/s12913-016-1620-2
Caterino JM, Weed SG, Espinola JA, Camargo Jr CA. National trends in emergency department antibiotic prescribing for elders with urinary tract infection 1996–2005. Acad Emerg Med. 2009;16(6):500–7. https://doi.org/10.1111/j.1553-2712.2009.00353.x.
Jung C, Brubaker L. The etiology and management of recurrent urinary tract infections in postmenopausal women. Climacteric. 2019;22(3):242–9.
Alós JI. Epidemiology and etiology of urinary tract infections in the community. Antimicrobial susceptibility of the main pathogens and clinical significance of resistance. Enferm Infecc Microbiol Clin. 2005; 23(Suppl 4):3–8. https://doi.org/10.1157/13091442.
Schappert SM, Rechtsteiner EA. Ambulatory medical care utilization estimates for 2007. Vital Health Stat. 2011;13(169):1–38.
Foxman B. Urinary tract infection syndromes: occurrence, recurrence, bacteriology, risk factors, and disease burden. Infect Dis Clin North Am. 2014;28(1):1–13. https://doi.org/10.1016/j.idc.2013.09.003.
Nawar EW, Niska RW, Xu J. National Hospital Ambulatory Medical Care Survey: 2005 emergency department summary. Adv Data. 2007;386:1–32.
Martínez MA, Inglada L, Ochoa C. Villagrasa, “Assessment of antibiotic prescription in acute urinary tract infections in adults. J Infect. 2007;54(3):235–44. https://doi.org/10.1016/j.jinf.2006.05.015.
Alanazi MQ, Al-Jeraisy MI, Salam M. Prevalence and predictors of antibiotic prescription errors in an emergency department, Central Saudi Arabia. Drug Healthc Patient Saf. 2015;7:103–11. https://doi.org/10.2147/dhps.s83770.
Al-Rubeaan KA, Moharram O, Al-Naqeb D, Hassan A, Rafiullah MR. Prevalence of urinary tract infection and risk factors among Saudi patients with diabetes. World J Urol. 2013;31(3):573–8. https://doi.org/10.1007/s00345-012-0934-x.
Alanazi MQ. An evaluation of community-acquired urinary tract infection and appropriateness of treatment in an emergency department in Saudi Arabia. Ther Clin Risk Manag. 2018;14:2363–73. https://doi.org/10.2147/tcrm.s178855.
Medina M, Castillo-Pino E. An introduction to the epidemiology and burden of urinary tract infections. Ther Adv Urol. 2019;11:1756287219832172. https://doi.org/10.1177/1756287219832172.
Ahmed AF, Solyman AA, Kamal SM. Potential host-related risk factors for recurrent urinary tract infection in Saudi women of childbearing age. Int Urogynecol J. 2016;27(8):1245–53. https://doi.org/10.1007/s00192-016-2965-0.
Ali SB, Perdawood D, Abdulrahman R, Al Farraj DA, Alkubaisi NA. Vitamin D deficiency as a risk factor for urinary tract infection in women at reproductive age. Saudi J Biol Sci. 2020;27(11):2942–47.
Albert X, Huertas I, Pereiró, II, Sanfélix J, Gosalbes V, Perrota C. Antibiotics for preventing recurrent urinary tract infection in non-pregnant women. Cochrane Database Syst Rev. 2004;2004(3):Cd001209. https://doi.org/10.1002/14651858.CD001209.pub2.
Raz R, Stamm WE. A controlled trial of intravaginal estriol in postmenopausal women with recurrent urinary tract infections. N Engl J Med. 1993;329(11):753–6. https://doi.org/10.1056/nejm199309093291102.
Perrotta C, Aznar M, Mejia R, Albert , Ng CW. Oestrogens for preventing recurrent urinary tract infection in postmenopausal women. Cochrane Database Syst Rev. 2008;2:Cd005131. https://doi.org/10.1002/14651858.CD005131.pub2.
Alsubaie SS, Barry MA. Current status of long-term antibiotic prophylaxis for urinary tract infections in children: An antibiotic stewardship challenge. Kidney Research and Clinical Practice. 2019;38(4):441.
Chu CM, Lowder JL. Diagnosis and treatment of urinary tract infections across age groups. Am J Obstet Gynecol. 2018;219(1):40–51. https://doi.org/10.1016/j.ajog.2017.12.231.
Welk B, Lenherr S, Santiago-Lastra Y, Norman HS, Keiser MG, Elliott CS. Differences in the incidence of urinary tract infections between neurogenic and non-neurogenic bladder dysfunction individuals performing intermittent catheterization. Neurourol Urodyn. 2022;41(4):1002–11.
Salib A, Rudnick B, Murphy A. Vesicoureteral reflux in adults with urinary tract infections: is there a role for treatment? Curr Urol Rep. 2020;21(10):1–5.
Guglietta A. Recurrent urinary tract infections in women: risk factors, etiology, pathogenesis and prophylaxis. Future Microbiol. 2017;12(3):239–46.
Arabi Z, et al. Urinary Tract Infections in the First 6 Months after Renal Transplantation. Int J Nephrol. 2021;2021:3033276. https://doi.org/10.1155/2021/3033276.
Vasudeva P, Madersbacher H. Factors implicated in pathogenesis of urinary tract infections in neurogenic bladders: some revered, few forgotten, others ignored. Neurourol Urodyn. 2014;33(1):95–100.
Kennelly M et al. Adult neurogenic lower urinary tract dysfunction and intermittent catheterisation in a community setting: risk factors model for urinary tract infections. Adv Urol. 2019;2019.
Langford BJ, et al. The Benefits and Harms of Antibiotic Prophylaxis for Urinary Tract Infection in Older Adults. Clin Infect Dis. 2021;73(3):e782–91. https://doi.org/10.1093/cid/ciab116.
Ten Doesschate,T et al. Nitrofurantoin 100 mg versus 50 mg prophylaxis for urinary tract infections, a cohort study. Clin Microbiol Infect. 2022; 28(2):248–54.
Ge IY, et al. Reducing risk of Clostridium difficile infection and overall use of antibiotic in the outpatient treatment of urinary tract infection. Ther Adv Urology. 2018;10(10):283–93.
Ahmed H, Farewell D, Jones HM, Francis NA, Paranjothy S, Butler CC. Antibiotic prophylaxis and clinical outcomes among older adults with recurrent urinary tract infection: cohort study. Age Ageing. 2019;48(2):228–34. https://doi.org/10.1093/ageing/afy146.
Drekonja DM, Rector TS, Cutting A, Johnson JR. Urinary tract infection in male veterans: treatment patterns and outcomes. JAMA Intern Med. 2013;173(1):62–8.
Mody L, Juthani-Mehta M. Older men may benefit from antimicrobial prophylaxis for recurrent urinary tract infections. Age Ageing. 2019;48(2):167–8. https://doi.org/10.1093/ageing/afy195.
Nitzan O, Elias M, Chazan B, Saliba W. Urinary tract infections in patients with type 2 diabetes mellitus: review of prevalence, diagnosis, and management. Diab Metab Syndr Obes Targets Ther. 2015;8:129.
Jent P, Berger J, Kuhn A, Trautner BW, Atkinson A, Marschall J. Antibiotics for preventing recurrent urinary tract infection: systematic review and meta-analysis. Open Forum Infect Dis. 2022;9(7):ofac327. https://doi.org/10.1093/ofid/ofac327.
Fisher H, et al. Continuous low-dose antibiotic prophylaxis for adults with repeated urinary tract infections (AnTIC): a randomised, open-label trial. Lancet Infect Dis. 2018;18(9):957–68. https://doi.org/10.1016/s1473-3099(18)30279-2.
Langford BJ, et al. The benefits and harms of antibiotic prophylaxis for urinary tract infection in older adults. Clin Infect Dis. 2021;73(3):e782–91.
Buck ES, Lukas VA, Rubin RS. Effective Prevention of Recurrent UTIs With Vaginal Estrogen: Pearls for a Urological Approach to Genitourinary Syndrome of Menopause. Urology. 2021;151:31–6. https://doi.org/10.1016/j.urology.2020.05.058.
Chang E, et al. Vaginal Estrogen as First-Line Therapy for Recurrent Urinary Tract Infections in Postmenopausal Women and Risk Factors for Needing Additional Therapy. Female Pelvic Med Reconstr Surg. 2021;27(3):e487–92. https://doi.org/10.1097/spv.0000000000000989.
Harding C, et al. Methenamine hippurate compared with antibiotic prophylaxis to prevent recurrent urinary tract infections in women: the ALTAR non-inferiority RCT. Health Technol Assess. 2022.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
HG collected data and performed Critical revision of the manuscript for important intellectual content. AA collected data and revised the final manuscript. RJ Wrote the research proposal for ethical approval and revised the final manuscript. RM collected data and revised the final manuscript. AS collected data and revised the final manuscript. EA collected data and revised the final manuscript. WB Revised the final manuscript for consistency. AS performed Critical revision of discussion part of the manuscript for important intellectual content. EM performed the analysis, and interpretation of data. LL revised and edited the final manuscript, review and updated the reference.SB Developed the idea and designed the methods, presented the discussion, wrote the manuscript, revised the content and finalization. All authors have critically reviewed and approved the final version and are responsible for the content and similarity index of the manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
The Institutional Review Board at King Abdullah International Medical Research Center, Ministry of National Guard-Health Affairs, Riyadh, Kingdom of Saudi Arabia (IRB no. 0984/21), approved the study. Patient confidentiality was ensured, and the collected patients' data used by the research team only. Serial numbers were used instead of medical record numbers to ensure anonymity. Written informed consent from the participants’ legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Consent for Publication
All authors agree for publication.
Conflict of Interest
None.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alghoraibi, H., Asidan, A., Aljawaied, R. et al. Recurrent Urinary Tract Infection in Adult Patients, Risk Factors, and Efficacy of Low Dose Prophylactic Antibiotics Therapy. J Epidemiol Glob Health 13, 200–211 (2023). https://doi.org/10.1007/s44197-023-00105-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44197-023-00105-4