Abstract
Background
Disease severity among patients infected with SARS-CoV-2 varies remarkably. Preliminary studies reported that the ABO blood group system confers differential viral susceptibility and disease severity caused by SARS-CoV-2. Thus, differences in ABO blood group phenotypes may partly explain the observed heterogeneity in COVID-19 severity patterns, and could help identify individuals at increased risk. Herein, we explored the association between ABO blood group phenotypes and COVID-19 susceptibility and severity in a Saudi Arabian cohort.
Methods
In this retrospective cohort study, we performed ABO typing on a total of 373 Saudi patients infected with SARS-CoV-2 and conducted association analysis between ABO blood group phenotype and COVID-19 infection severity. We then performed gender-stratified analysis by dividing the participating patients into two groups by gender, and classified them according to age.
Results
The frequencies of blood group phenotypes A, B, AB and O were 27.3, 23.6, 5.4 and 43.7%, respectively. We found that blood group phenotype O was associated with a lower risk of testing positive for COVID-19 infection (OR 0.76 95% CI 0.62–0.95, p = 0.0113), while blood group phenotype B was associated with higher odds of testing positive (OR 1.51 95% CI 1.17–1.93, p = 0.0009). However, blood group phenotype B was associated with increased risk in the mild and moderate group but not the severe COVID-19 infection group. Blood group phenotype O was protective in all severity groups.
Conclusion
Our findings provide evidence that blood group phenotype B is a risk for COVID-19 disease while blood group phenotype O is protective from COVID-19 infection. However, further studies are necessary to validate these associations in a larger sample size and among individuals of different ethnic groups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The rapid global spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the resulting coronavirus disease 2019 (COVID-19) has caused drastic morbidity and mortality, igniting an unprecedented effort from scientists and clinicians to rapidly unravel the pathogenesis of disease [1]. COVID-19 is clinically characterized by a multitude of symptoms that vary in severity [2]. The most common symptoms are: fever, cough, fatigue, headache, shortness of breath, conjunctivitis and gastrointestinal problems [3]. There is remarkable variability in viral susceptibility and disease severity caused by SARS-CoV-2 infection, while certain individuals exhibit almost no symptoms, others experience acute respiratory distress syndrome, septic shock, and even death [4, 5].
The ABO blood group system, which is widely used in clinical practice, has been shown in previous studies to confer differential viral susceptibility and disease severity caused by viruses, including SARS-CoV-1 [6]. Indeed, blood groups can play a direct role in infection by serving as receptors or co-receptors for viruses [7]. As with SARS-CoV-1, preliminary evidence suggests a potential correlation between blood group antigens and increased susceptibility to or amplified severity of COVID-19 disease [8,9,10,11]. Notably, a higher risk of severe COVID-19 was observed among individuals with blood group A [12], while blood group O was a protective factor [13].
Given that SARS-CoV-2 infection is heterogeneous in clinical presentation and disease course, it is imperative that immunological biomarkers are further elucidated to better define therapeutic strategies and treatment options for COVID-19. Differences in ABO blood group antigen expression may help explain discrepancies of COVID-19 spread, severity and mortality. Additionally, insights on how ABO influences the response to COVID-19 may help identify populations with increased risk and create targeted public health policies. Hence, we performed ABO typing on 373 Saudi patients infected with SARS-CoV-2 to explore the relationship between ABO blood group phenotypes and COVID-19 susceptibility and severity. We further classified the cohort according to gender and age.
2 Methods
2.1 Ethics Statement and Patient Recruitment
Ethical approval for this study and all experimental protocols was obtained from the Institutional Review Board (IRB) at King Abdullah International Medical Research Center (KAIMRC), Ministry of National Guard—Health Affairs (MNGHA) in Riyadh and site-specific approval was obtained from all participating centers. Written informed consent for clinical genotyping and participation in this study was obtained from all patients or their guardians upon recruitment. This retrospective cohort study recruited a total of 373 patients with confirmed COVID-19, which was defined as a positive SARS-CoV-2 viral RNA polymerase chain reaction (PCR) test from nasopharyngeal swabs or lower respiratory tract samples including endotracheal aspirate, bronchoalveolar lavage fluid or sputum. All patients were recruited from King Abdulaziz Medical City (KAMC) in Riyadh and Ministry of Health Quarantine Facility in Makkah and recruitment was conducted between May 2020 and August 2020.
2.2 Data Collection
Detailed demographic information, clinical data and laboratory findings were collected from all recruited patients and entered into the Saudi Human Genome Program repository and a secure REDCap electronic data capture tool hosted at KAIMRC. Demographics composed of different factors, such as gender, age, nationality and comorbidities. Clinical data comprised vital signs and disease manifestations including fever, cough, dyspnea, diarrhea and chest pain.
2.3 Patient Phenotype
The cohort included 27 patients whose disease severity was categorized as asymptomatic; 88 patients whose disease severity was categorized as mild, which was defined as patients requiring only self-isolation with mild symptoms, such as fever, headache and cough; 88 patients whose disease severity was categorized as moderate, which was defined as patients requiring hospital admission and evidence of lower respiratory disease during clinical assessment or imaging; and 170 patients whose disease severity was categorized as severe, which was defined as patients requiring ICU admission and/or invasive mechanical ventilation. The asymptomatic and mild group were merged and labeled “mild” for simplicity.
2.4 Sample Collection, DNA Analysis and ABO Typing
Blood samples were collected in EDTA tubes from all 373 patients infected with SARS-CoV-2 and human genomic DNA was extracted from peripheral blood using the Gentra Puregene Blood Kit according to the manufacturer’s instructions. The yield of the DNA was then quantified using NanoDropTM spectrophotometer using standard procedures before genotyping. ABO antigens of all 373 patients were typed by next generation sequencing (NGS) using the Illumina NGS Platform at the laboratories of Histogenetics (Ossining, NY). Briefly, amplification primers were designed for exon 2, exon 6 and exon 7, one amplicon each for exon 2 and 6, and 3 amplicons for exon 7. ABO exon 7 is 698 base pairs long, 3 overlapping amplicons were developed to phase the allelic sequences. When phasing was not possible with NGS data, PacBio 1 kb amplicon was used for phasing exon 7. When discrepancies were found between sequence-based genotyping and serological blood ABO phenotyping, the entire exons (total 9 exons) were sequenced. Blood groups were recorded as phenotype.
2.5 Statistical Analysis
The STATA software, version 16.0 (StataCorp, College Station, TX, USA) was used for statistical analysis. Characteristics of the study population were examined and stratified by ABO blood group phenotype and disease severity using descriptive statistics for age and gender. Chi-square test was employed to assess the statistical significance of differences in proportions of blood group phenotypes between the two groups. Age was expressed as mean values ± SD. Associations between different blood group phenotypes and disease severity were analyzed using the Odds Ratio (OR) with 95% confidence interval (CI). p value of less than 0.05 was taken as significant.
3 Results
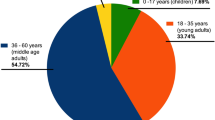
The present study consisted of a total of 373 patients with COVID-19-positive PCR. Of the 373 patients, 218 (58.4%) were males and 155 (41.6%) were females. The age range of the patient cohort was 15–104 years with a mean age of 53.49 (Table 1). The frequencies of blood group phenotypes A, B, AB and O were 27.3, 23.6, 5.4 and 43.7%, respectively. The degree of disease severity increased with age. The analysis showed no statistical significance between gender and severity, however, severe cases were higher in the male gender category while mild cases were higher in females.
Table 2 illustrates the distribution of patients’ gender and disease severity in relation to age. In both gender categories, age increased with disease severity. However, there was no significant difference in the distribution of patients in the gender versus disease severity.
Table 3 illustrates the association between age, blood group phenotype and disease severity. In all blood group phenotypes, age increased with disease severity. However, there was no significant difference in the distribution of patients in the severity versus blood group.
Figure 1 illustrates the blood group distribution in each COVID-19 patient category. In the mild group, the frequencies of blood group phenotypes O, A, B and AB were 42, 30, 23 and 5%, respectively. In the moderate cases, the frequencies of O, A, B and AB were 40, 29, 25 and 6%, respectively. In the severe group, the frequencies of blood group phenotypes O, A, B and AB were 40, 35, 20 and 5%, respectively.
Comparing the COVID-19-infected patients to the general population, we found an increased risk for blood group phenotypes B and AB and a significant decreased risk in blood group phenotype O. Table 4 shows that blood group phenotype B carried a risk for COVID-19 disease (OR 1.51, 95% CI 1.17–1.93, p = 0.0009). This association was seen mainly in mild disease (OR 1.57, 95% CI 0.98–2.44, p = 0.038) and moderate disease (OR 1.73, 95% CI 1.02–2.83, p = 0.023). However, this association did not reach significance for the severe disease (OR 1.36, 95% CI 0.91–1.98, p = 0.12). At the same time, blood group phenotype O appears to be protective for COVID-19 disease (OR 0.76, 95% CI 0.62–0.95, p = 0.011). This was the case for all disease severity categories, although the significance was not achieved. In addition, only in the total group, blood group AB carried a risk for COVID-19 disease (OR 1.8, 95% CI 1.11–3.00, p = 0.0072).
4 Discussion
Immense inter-individual susceptibility to SARS-CoV-2 infection and clinical variability in the course of COVID-19 disease has been observed, ranging from silent or benign infection to rapid progression to respiratory failure [2]. Previous work has demonstrated that ABO allele frequencies and distributions of the ABO gene can be appropriate indices for investigating vulnerability to certain infections or disease severity following infections, including SARS-CoV-1 [6]. Correspondingly, recent studies have identified correlations between ABO blood group phenotypes and risk of SARS-CoV-2 infection, as well as susceptibility to severe ICU-requiring COVID-19 disease [14,15,16,17,18,19,20]. Hence, we sought to explore these trends among the population in Saudi Arabia. Herein, we performed ABO typing on 373 Saudi patients with confirmed SARS-CoV-2 infection and conducted association analysis between ABO blood group phenotypes and COVID-19.
Overall, we found no significant associations between blood group phenotype and COVID-19 severity. However, we found evidence for associations between blood group phenotype and risk of infection. Several articles were similar in reporting that risk was increased among type A individuals and decreased among O type individuals. However, some articles reported contradicting observations, suggesting that blood group phenotype B individuals are more susceptible to SARS-CoV-2 infection instead of type A. We found that individuals with blood group phenotypes B and AB were at higher odds of testing positive for COVID-19, while type O individuals were less likely to test positive. In Saudi Arabia, the distribution of blood group phenotypes O, A, B, and AB was 50, 29, 17 and 4%, respectively [21]. This suggests that it is likely that the rate of infection is highest in O type individuals. Meanwhile, we found that individuals with blood group phenotypes B and AB were at higher odds of testing positive for COVID-19, while type O individuals were less likely to test positive. Our findings are mostly consistent with the findings reported by Latz et al. who showed that patients with blood group phenotypes B and AB were more likely to test positive while blood group phenotype O was less likely to test positive for COVID-19 [14]. Intriguingly, another study from Saudi Arabia reported similar observations, suggesting that patients with AB blood group have higher susceptibility while patients with O blood group have lower susceptibility to COVID-19 infection [15]. Two studies that were performed in populations closely related to the Saudi population found similar associations. Almadhi and colleagues found a significantly increased risk with blood group phenotype B instead of A in Bahrain [16]. Moreover, Al-Youha et al. detected a lower prevalence of blood group phenotype O in COVID-19 patients and a higher prevalence of B and AB [17]. However, a recent study from Saudi Arabia reported contradicting results, stating that blood group phenotype O individuals are at increased risk for COVID-19, while AB individuals are at decreased risk [18]. This discrepancy may indicate that hidden confounders may be inherent in the tested populations. Also, the variation in results could be attributed to the modest size and suggests that larger sample sizes are needed to study these associations more precisely in Saudi Arabia.
Interestingly, although the variability in the data was mainly in blood group phenotypes A and B, almost all mentioned studies appear to correlate blood group phenotype O with a lower risk for the disease. This is consistent with an association discovered for SARS-CoV-1, in which blood group phenotype O was less common in infected individuals [6]. We found that blood group phenotype B was significantly higher in COVID-19 patients, but the severity was not associated as we have seen a 57% higher risk in mild patients and a 73% higher risk in moderate infection. However, the severe patients only had a 36% higher risk. Intriguingly, this correlates with an association discovered by Ziets et al. in which blood group phenotype B had increased risk of intubation but decreased risk of death [19].
Understanding the role of ABO blood group phenotype in impacting susceptibility and severity of COVID-19 offers the opportunity to gain novel insights into disease pathogenesis, risk stratification and response to therapy. To date, this is the third study that investigates the relationship between ABO and COVID-19 in Saudi Arabia. Our study adds to the growing body of literature around the role of ABO in COVID-19 and findings from our study provide further evidence for several associations that have been reported elsewhere. Nevertheless, these findings should not be taken as conclusive due to certain limitations. First, our study is focused solely on ABO and overlooks the possibilities that other confounding factors may affect the response to COVID-19. Second, our study is confined to the Saudi population. The ABO gene possesses a high degree of polymorphisms and ABO blood group phenotypes have considerably different distributions across populations [22]. Thus, one cannot necessarily assert that the findings presented in this study would apply to other populations or ethnic groups. Finally, the sample size was relatively small and the prevalence of each blood group phenotype is not uniform, with a particularly low sample size in the AB blood group phenotype. Additional studies are necessary to validate these findings in a larger sample size and among individuals of different ethnicities.
In conclusion, our findings provide evidence that blood group B might be a risk factor for COVID disease, while blood group O could be protective from COVID-19 infection in a uniquely Saudi cohort. Nevertheless, the mechanistic link between blood group phenotypes and COVID-19 infection remains elusive. Thus, further interrogation of current findings, both as to their usefulness in risk stratification of patients with COVID-19 and toward a mechanistic understanding of the underlying pathophysiology, is warranted.
Data Availability
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
References
Han Q, Lin Q, Jin S, You L. Coronavirus 2019-nCoV: a brief perspective from the front line. J Infect. 2020;80(4):373–7. https://doi.org/10.1016/j.jinf.2020.02.010.
Eastin C, Eastin T. Clinical characteristics of coronavirus disease 2019 in China: Guan W, Ni Z, Hu Y, et al. N Engl J Med. 2020 Feb 28 [Online ahead of print]. https://doi.org/10.1056/NEJMoa2002032. J Emerg Med. 2020;58(4):711–712. https://doi.org/10.1016/j.jemermed.2020.04.004.
Hu B, Guo H, Zhou P, Shi ZL. Characteristics of SARS-CoV-2 and COVID-19. Nat Rev Microbiol. 2021;19(3):141–54. https://doi.org/10.1038/s41579-020-00459-7.
Wang B, Li R, Lu Z, Huang Y. Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis. Aging (Albany NY). 2020;12(7):6049–57. https://doi.org/10.18632/aging.103000.
Guan WJ, Liang WH, Zhao Y, et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J. 2020;55(5):2000547. https://doi.org/10.1183/13993003.00547-2020.
Cheng Y, Cheng G, Chui CH, et al. ABO blood group and susceptibility to severe acute respiratory syndrome [published correction appears in JAMA. 2005 Aug 17;294(7):794. Cheng, Yufeng [corrected to Cheng, Yunfeng]]. JAMA. 2005;293(12):1450–1451. https://doi.org/10.1001/jama.293.12.1450-c.
Cooling L. Blood groups in infection and host susceptibility. Clin Microbiol Rev. 2015;28(3):801–70. https://doi.org/10.1128/CMR.00109-14.
Li J, Wang X, Chen J, Cai Y, Deng A, Yang M. Association between ABO blood groups and risk of SARS-CoV-2 pneumonia. Br J Haematol. 2020;190(1):24–7. https://doi.org/10.1111/bjh.16797.
O’Sullivan JM, Ward S, Fogarty H, O’Donnell JS. More on Association between ABO blood groups and risk of SARS-CoV-2 pneumonia. Br J Haematol. 2020;190(1):27–8. https://doi.org/10.1111/bjh.16845.
Gérard C, Maggipinto G, Minon JM. COVID-19 and ABO blood group: another viewpoint. Br J Haematol. 2020;190(2):e93–4. https://doi.org/10.1111/bjh.16884.
Liu N, Zhang T, Ma L, et al. The impact of ABO blood group on COVID-19 infection risk and mortality: a systematic review and meta-analysis. Blood Rev. 2021;48: 100785. https://doi.org/10.1016/j.blre.2020.100785.
Bhattacharjee S, Banerjee M, Pal R. ABO blood groups and severe outcomes in COVID-19: a meta-analysis. Postgrad Med J. 2020. https://doi.org/10.1136/postgradmedj-2020-139248.
Muñiz-Diaz E, Llopis J, Parra R, et al. Relationship between the ABO blood group and COVID-19 susceptibility, severity and mortality in two cohorts of patients. Blood Transfus. 2021;19(1):54–63. https://doi.org/10.2450/2020.0256-20.
Latz CA, DeCarlo C, Boitano L, et al. Blood type and outcomes in patients with COVID-19. Ann Hematol. 2020;99(9):2113–8. https://doi.org/10.1007/s00277-020-04169-1.
Aljanobi G, Alhajjaj A, Alkhabbaz F, Al-Jishi J. The relationship between ABO blood group type and the COVID-19 susceptibility in Qatif Central Hospital, Eastern Province, Saudi Arabia: a retrospective cohort study. Open J Internal Med. 2020;10:232–8. https://doi.org/10.4236/ojim.2020.102024.
Almadhi MA, Abdulrahman A, Alawadhi A, Rabaan AA, Atkin S, AlQahtani M. The effect of ABO blood group and antibody class on the risk of COVID-19 infection and severity of clinical outcomes. Sci Rep. 2021;11(1):5745. https://doi.org/10.1038/s41598-021-84810-9.
Al-Youha SA, Alduaij W, Al-Serri A, et al. The impact of ABO blood groups on clinical outcomes and susceptibility to COVID-19: a retrospective study in an unselected population. Transfusion. 2021;61(5):1631–41. https://doi.org/10.1111/trf.16365.
Badedi M, Alnami A, Darraj H, et al. Clinical characteristics and ABO blood groups in COVID-19 patients, Saudi Arabia. Medicine (Baltimore). 2021;100(30): e26738. https://doi.org/10.1097/MD.0000000000026738.
Zietz M, Zucker J, Tatonetti NP. Associations between blood type and COVID-19 infection, intubation, and death. Nat Commun. 2020;11(1):5761. https://doi.org/10.1038/s41467-020-19623-x.
Kabrah SM, Kabrah AM, Flemban AF, Abuzerr S. Systematic review and meta-analysis of the susceptibility of ABO blood group to COVID-19 infection. Transfus Apher Sci. 2021;60(4): 103169. https://doi.org/10.1016/j.transci.2021.103169.
Alzahrani M, Jawdat D, Alaskar A, Cereb N, Hajeer AH. ABO and Rh blood group genotypes in a cohort of Saudi stem cell donors. Int J Immunogenet. 2018;45(2):63–4. https://doi.org/10.1111/iji.12354.
Yip SP. Sequence variation at the human ABO locus. Ann Hum Genet. 2002;66(Pt 1):1–27. https://doi.org/10.1017/S0003480001008995.
Acknowledgements
The authors thank and acknowledge the Saudi Human Genome Program (SHGP) as well as the Therapy Development Research Program at King Abdulaziz City for Science and Technology (KACST) for the technical and financial support (https://shgp.kacst.edu.sa). In addition, the authors acknowledge King Abdullah International Medical Research Center (KAIMRC) and the Ministry of National Guard Health Affairs (MNG-HA) for the scientific and ethical approval of the project RC20/221. The authors thank all study participants and their families for contributing to this study. In addition, the authors thank Dr. Hani M. Al-Afghani for providing us with samples from the quarantine facilities in Makkah. The authors thank Professor Yassin Arabi and his team for providing the samples from the ICU, King Abdulaziz Medical City. Finally, the authors thank all staff at the Developmental Medicine Department Laboratory for assisting in DNA extraction.
Funding
This research was funded by King Abdulaziz City for Science and Technology (KACST) and the Saudi Human Genome Project (SHGP).
Author information
Authors and Affiliations
Contributions
Conceptualization, MA and DJ; methodology, MA, DJ and SM; validation, MA, DJ, SM, NA, AH and MSA; formal analysis, MA, DJ, SM, NA, and AH; data curation, MA, and DJ; writing—original draft preparation, MA, and NA; writing—review and editing, MA, DJ, SM, NA, AH and MSA; supervision, MA and SM; project administration, MA; funding acquisition, MA.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflict of interest.
Ethical Approval
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board at King Abdullah International Medical Research Centre, Riyadh; (RC 20/221, approved 28/04/2020).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jawdat, D., Hajeer, A., Massadeh, S. et al. Correlation between ABO Blood Group Phenotype and the Risk of COVID-19 Infection and Severity of Disease in a Saudi Arabian Cohort. J Epidemiol Glob Health 12, 85–91 (2022). https://doi.org/10.1007/s44197-021-00023-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44197-021-00023-3