Abstract
Dental defects and loss are common oral diseases that seriously affect the chewing efficiency of patients and thereby affect their health. With the development of tissue engineering technology, dental tissue regeneration has emerged as a promising technique. Cell type, extracellular matrix (ECM) environment, cytokines and other factors which affect odontogenic differentiation and dental tissue regeneration have aroused significant interest. The functional ECM consists of extracellular components that control the initiation and growth of crystal deposition and regulate the differentiation and regeneration of endogenous or exogenous stem cells in the defect site. At present, the function and regulatory mechanism of the functional ECM in this process remain poorly understood. Therefore, elucidating the effect of the functional ECM on odontogenic differentiation and its mechanism has great scientific significance and potential clinical application. This review explored functional ECM components involved in odontogenic differentiation and dental tissue regeneration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Dental defects and loss are common oral diseases that seriously affect the mastication efficiency of patients and thus affect their digestive system and metabolic capacity. The National Health and Nutrition Examination Survey indicated that 91% of adults aged 20–64 had dental defects (Dye et al. 2015). With the development of tissue engineering technology, dental tissue regeneration by mesenchymal stem cells has emerged as a promising technology (Ravindran and George 2015). However, the translation of this technology for clinical application is a remote possibility, and a few key issues need to be resolved urgently. Little is currently known about the effect of the extracellular matrix (ECM) environment on the final odontogenic differentiation in stem cell replantation. Accordingly, further studies are warranted to assess the impact of the ECM on the regeneration of tooth tissue after the implantation of mesenchymal stem cells to provide a basis for the final safe and practical application of stem cells in the clinic.
In order to improve the success rate of tooth tissue regeneration, the odontogenic differentiation ability of stem cells implanted in jaw bone must be improved. Current studies suggest that the eECM environment of mesenchymal stem cells is the "soil" for the survival of stem cells, which plays a vital role in the behavior and function of stem cells. In such an ECM environment, stem cells are subjected to various stimuli that regulate stem cell activities in a complex synergy. It is widely acknowledged that stem cells cannot perform their original functions without the proper ECM environment. Therefore, it is necessary to study the influence of the ECM environment on stem cells during tissue regeneration. Most tissues that constitute an organism are composed of living cells embedded in the ECM, which is a critical microenvironment for stem cells (Frantz et al. 2010). The ECM comprises structural proteins, mucopolysaccharides, growth factors and cytokines, secretase, and glycoproteins called stromal proteins. The ECM provides structural stability for tissues and organs and regulates the activity of growth factors and cytokines by linking inactive precursor forms directly into the structural components of the ECM. Synthesis of ECM has profound effects on cell behavior, including adhesion, proliferation, migration, and maintenance of the stem cell microenvironment. Each tissue and organ in the human body has a unique ECM, which regulates cell differentiation, migration, wound healing and immune response.
It is well-established that ECM regulates endogenous and exogenous stem cells. Studies have shown that the active components of the ECM can improve the ECM environment of endogenous stem cells and regulate the migration of endogenous stem cells to the defect site for odontogenic differentiation and tissue regeneration. However, under certain pathological conditions such as inflammation, hypoxia, and significant defects, endogenous stem cells and their ECM are severely damaged and cannot function properly. Therefore, exogenous stem cells and ECM should be transplanted to mediate tooth differentiation. Under these pathological conditions, the ECM environment of exogenous stem cells and the extracellular factors secreted by exogenous stem cells themselves could induce odontogenic differentiation and tissue regeneration. These results suggest that ECM is a crucial regulator of dental differentiation of endogenous and exogenous mesenchymal stem cells (Saito et al. 2015).
The ECM of dental tissue is composed of 90% collagen and 10% non-collagen. Collagen provides the scaffold for the deposition of hydroxyapatite plate-like crystals, and functional ECM is believed to control the initiation and growth of the crystalline deposition. Most ECM proteins, such as SIBLING family proteins, are located in the space of collagen fibers in the ECM and aggregate around the dentin tubules, regulating the formation of hydroxyapatite crystals through the ARG-GLy-ASP (RGD) motif. Cytokines such as the TGF-β family and BMP family are secreted by cells into the ECM and bind to and preserve ECM for a long time to regulate the odontoblast differentiation of surrounding cells. Degradation enzymes such as the MMP family can degrade various protein substrates in the ECM, including collagen and elastin, thus providing space for the organic matrix components and further growth of mineralized crystals during dentin formation. Specific matrix components such as extracellular vesicles can interact with ECM macromolecules to degrade collagen and promote dentin mineralization(Table 1). Recent tissue engineering strategies have focused on mimicking the composition of ECM to achieve the required cellular behavior and lineage-specific differentiation to promote tissue regeneration. Therefore, it is vital to elucidate the role and mechanism of the specific functional ECM involved in dental cell differentiation. This review aimed to explore all ECM components involved in developing odontogenic stem cells.
1 ECM proteins
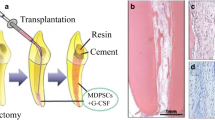
ECM proteins mainly consist of small integrin-binding ligand N-linked glycoproteins (SIBLING) (Frantz et al. 2010), representing a family of non-collagen proteins in bone and dentin ECM. Their encoding genes are located in human chromosome 4q21 and have a similar exon structure. The formation of hydroxyapatite crystals is regulated by their Arg-Gly-Asp (RGD) motif (He et al. 2003), (Fisher et al. 2001), (Minamizaki and Yoshiko 2015). These proteins are mainly expressed in the bone and dentin, secreted into the ECM during osteoid formation, and mineralized. The SIBLING family members include dentin matrix protein 1 (DMP1), dentin sialophosphoprotein (DSPP), bone sialoprotein (BSP), osteopontin (OPN), and extracellular stromal phosphate glycoprotein (MEPE). These five proteins play essential roles in bone tissue formation and tooth development. Additionally, other ECM proteins such as periostin are primarily expressed in the dentin and secretory cells such as odontoblasts (Fig. 1).
1.1 DMP1
DMP1 is an acidic phosphorylated non-collagen protein found in the bone and dentin ECM. DMP1 can be hydrolyzed into two active functional segments: C-DMP1 (57 kDa) and N-DMP1 (37 kDa). C-DMP1 is mainly expressed in mineralized dentin, while N-DMP1 is mainly expressed in non mineralized dentin. Many experiments have shown that DMP1 and its hydrolytic functional fragments can bind calcium and initiate hydroxyapatite nucleation, thus playing a pivotal role in dentin formation and mineralization (He et al. 2003; Ravindran and George 2015). Extracellular C-DMP1, produced by proteolysis of DMP1 by MMP-2, regulates the odontogenic differentiation of endogenous mesenchymal stem cells. Mechanism studies have found that C-DMP1 can induce HA crystal formation (Chaussain et al. 2009). Current evidence suggests that the N-DMP1 fragment is primarily located in the nonmineralized predentin, but its regulatory effect and mechanism have not been reported.
In addition to its role in stromal mineralization, DMP1 acts as an intracellular and extracellular signaling molecule at several stages of tooth development, affecting the differentiation of odontoblasts. Since DMP1 has a functional nuclear localization signal (NLS), intracellular transport of proteins can be achieved (Siyam et al. 2012). In the nucleus, DMP1 binds to the DSPP promoter and influences tooth differentiation of preodontoblasts by controlling DSPP expression (Gibson et al. 2013). In addition, extracellular DMP1 triggers calcium-mediated signal transduction through the cell surface receptor GRP78 endocytosis, leading to exogenous stem cell odontoblast differentiation (Merkel et al. 2019; Padovano et al. 2015). Besides, DMP1 can be anchored in the ECM to activate the mitogen-activated protein kinase (MAPK) pathway and ultimately promote the signaling mechanism of ECM-osteocytes by activating cell surface integrin α5β3 (Wu et al. 2011). Interestingly, a study simulated tooth perforation on freshly isolated teeth and injected DPSCs, DMP1, and collagen scaffold materials into the teeth, the results showed that in the presence of DMP1, cell differentiation into odontoblasts and dentin production was better and faster (Alsanea et al. 2011). Subcutaneous replantation experiments also fully demonstrated the ability of DMP1 to induce regeneration of dentin from exogenous stem cells (Saito et al. 2015). Thus, DMP1 plays various roles at different stages of mineralized tissue development, from regulating the lineage-specific differentiation of endogenous and exogenous mesenchymal stem cells to nucleation of crystalline hydroxyapatite.
1.2 DSPP
DSPP is an ECM protein that is closely related to tooth development and forms dentin sialoprotein (DSP) and dentin phosphorus protein (DPP) after proteolytic activation (Yamamoto et al. 2015). DPP is mainly expressed by dentin cells and is the most abundant non-collagen protein in the dentin matrix. The primary function of DPP in the matrix is to initiate the nucleation of hydroxyapatite crystals (Villarreal-Ramirez et al. 2017; Boskey and Villarreal-Ramirez 2016; Ritchie 2018; Kongkiatkamon et al. 2021). Recently, DPP was shown to possess a signal transduction function and could initiate mesenchymal stem cell lineage-specific dental differentiation (Sfeir et al. 2011). In the ECM, DPP mediates cell adhesion and initiates integrin-mediated signal transduction (Eapen et al. 2012a; Eapen et al. 2012b). DPP also initiates calcium- and calmodulin-dependent signal transduction to promote dental differentiation of precursor mesenchymal cells (Eapen et al. 2013). Furthermore, DSP acts as a ligand in an RGD-independent manner and is involved in intracellular signaling via interaction with integrin β6. Moreover, the DSP domain regulates DSPP expression and odontoblast homeostasis via a positive feedback loop (Wan et al. 2016).
An increasing body of evidence suggests that disruption of mineralization homeostasis might be crucial for DSPP mutations resulting in dentin disorders (Jia et al. 2015). In an animal experiment, changes in the teeth of wild-type and DSPP-knockout C57BL/6 mice during 1 to 3 months postbirth were detected,the loss of DSPP caused dental pulp cell differentiation into chondroid cells, indicating that DSPP promoted the repair function of the dental pulp and the differentiation function of dental tissue (Guo et al. 2014). In another knockout experiment, defective dentin, alveolar and calvarial bones, and sutures were observed in mice during development (Chen et al. 2016). Cellular experiments revealed that DSPP overexpression improved the mineralization ability of stem cells and was accompanied by the expression of early odontogenic marker genes (Verdelis et al. 2016). These results indicate that DPP and DSP are multifunctional proteins and play essential roles in matrix mineralization and signal transduction pathways.
1.3 BSP
BSP is the main non-collagen protein involved in the mineralization process of the connective tissues such as dentin, cementum, and calcified cartilage. BSP is well-recognized for regulating the formation of hydroxyapatite crystals in teeth (Fisher et al. 2001). In recent years, studies have explored the expression and regulation of the BSP gene in tooth development and regeneration and tissue engineering in transgenic mice. The RGD sequence near the carboxy-terminal of BSP protein is a cell attachment site recognized by the αvβ3 integrin receptor, which can promote cell signal transduction, cell attachment, and migration (Oldberg et al. 1988a; Oldberg et al. 1988b). Additionally, the polyglutamic acid region at the amino terminus mediates the binding of BSP to hydroxyapatite, which contains a protein structure with a high affinity for calcium, hydroxyapatite, and other minerals (Paz et al. 2005). Thus, it plays a crucial role in mineralization.
The histopathological findings of BSP knockout mice consist of acellular osteopenia with a lower degree of mineral deposition, periodontal ligament detachment, and periodontal tissue destruction (Foster et al. 2015; Soenjaya et al. 2015). With age, extensive root and alveolar bone resorption have also been observed (Foster et al. 2013). BSP is the acting molecule in osteogenesis during orthodontic treatment, playing an important role in dentine regeneration in the root (Baloul 2016). Subsequent studies have found that the synergic effect of BSP and inorganic pyrophosphate (PPi) in the ECM can lead to normal dentine development (Ao et al. 2017). These results suggest that BSP plays a vital role in the formation of acellular dentin and may be involved in the initiation of root surface mineralization. In addition, BSP, like other SIBLING proteins, exists in restorative dentin (Bouleftour et al. 2016). Owing to its importance in maintaining bone integrity, BSP is essential for periodontal function. However, its specific mechanism of action remains to be elucidated.
1.4 OPN
OPN, also known as secreted phosphoprotein 1 (SPP1), is a highly phosphorylated 34 kDa protein found in bone and tooth ECM (Sodek et al. 2000). OPN can bind calcium ions to cause and promote matrix mineralization and is a crucial regulator of hydroxyapatite nucleation affecting the shape and size of hydroxyapatite crystals (Singh et al. 2018), (Icer and Gezmen-Karadag 2018), (Qiu et al. 2004), (Giachelli and Steitz 2000).
In addition to its direct role in matrix mineralization, OPN has signal transduction properties. The RGD domain in OPN can bind to α4β1 integrins, thereby promoting the integrin-mediated attachment of osteoblasts (Forsprecher et al. 2011). OPN can also initiate intracellular signal transduction function in other cells, such as lymphocytes, T cells, and osteoclasts, and interact with CD44 cells via intracellular and extracellular signaling (Singh et al. 2018; Zohar et al. 2000; Suzuki et al. 2002; Zhu et al. 2004; Morath et al. 2016). Thus, OPN can affect the attachment of osteoclasts. There is ample evidence suggesting that adding growth factors, TGF-β1 and BMP4, to mouse dental mesenchymal cells (rDMCs) could significantly increase the expression of OPN and thus accelerate the odontogenic differentiation of rDMCs (Zhao et al. 2014). Some transcription factors also contribute to tooth differentiation, overexpression of Bobby Sox Homology transcription factors in DPSCs can cause increased expression of OPN, leading to tooth differentiation of stem cells (Choi et al. 2014). OPN has different functions in different cell types. Interestingly, it has been reported that different posttranslational modifications, such as glycosylation, sulfation, transglutamination, and phosphorylation, influence the functional properties of OPN (Lok and Lyle 2019; Hoac et al. 2017). Phosphorylation and dephosphorylation of OPN appear to control several of its biological functions, such as cell adhesion and migration (Ek-Rylander and Andersson 2010). In mineralized tissues, OPN promotes and inhibits the nucleation of hydroxyapatite at different stages and promotes the activities of osteoclasts or osteoblasts via its signal transduction function.
1.5 MEPE
MEPE was first identified by MacDougall et al. as a protein expressed during dentin formation related to the development of tooth hard tissue (MacDougall et al. 2002). The activity of MEPE depends on its cleavage state and phosphorylation. Recently, acidic serine aspartate-rich MEPE-associated (ASARM) peptides have been identified as functional fragments of MEPE, which are highly conserved sequences (Rowe et al. 2000). MEPE participates in bone homeostasis via two domains, the RGD domain and ASARM motif, that inhibit bone resorption and mineralization, respectively (Schrauwen et al. 2019; Salmon et al. 2013; Salmon et al. 2014). A study investigated the effects of ASARM peptide on tooth differentiation and matrix mineralization using exogenous stem cells from human exfoliated deciduous teeth (SHEDs) that were seeded on a 3D collagen scaffold and induced to undergo dental differentiation. Cells were cultured with the ASARM peptide synthesized from the human MEPE sequence. The phosphorylated ASARM peptide could inhibit the differentiation of SHEDs in vitro, accompanied by high expression of MEPE and no mineralized nodule production. Furthermore, to assess the effects in vivo, phosphorylated ASARM peptide was transplanted into the pulp injury model of grinding teeth in mice. Interestingly, it prevented the damaged dental tissue repair and mineralization and increased MEPE levels were observed by immunofluorescence staining. Finally, it was proved that the active fragment of MEPE, the ASARM peptide, inhibited dental differentiation and matrix mineralization with increased MEPE expression. Moreover, the MEPE knockout mouse model showed an increase in the number of dentine cells and enhanced mineralization capacity, indicating that MEPE is an inhibitor of mineralization differentiation (Liu et al. 2005). Interestingly, Wei et al. found that MEPE and DSPP have similar mineralization regulation abilities for DPCs,that is, MEPE also promoted tooth differentiation (Wei et al. 2007). Another study suggested that MEPE may be instrumental in craniofacial and dental matrix maturation, potentially maintaining a nonmineralized matrix (Gullard et al. 2016).
At present, it is widely believed that MEPE expression in stem cells is a marker of tooth differentiation. Together with DSPP and DSP-1, it is considered a routine marker to detect dental progression (Zhu et al. 2020).
1.6 Periostin
Periostin is a 90 kDa stromal cell protein involved in tissue remodeling by promoting cell adhesion, cell differentiation, cell survival, and fiber formation (Bonnet et al. 2016). In teeth, periostin is expressed by ameloblasts, odontoblasts, and periodontal membrane cells (Ma et al. 2011). Based on its molecular properties and protein interactions, periostin functions are divided into two categories: intracellular fibrogenic function and extracellular regulation of cell movement (Kudo 2011; Tanabe et al. 2010). Periostin promotes proteolytic activation of lysozyme to cause collagen cross-linking, playing an essential role in collagen-fibrillar cross-linking and ECM tissue by binding directly to type I collagen, fibrinogen, and tenascin-C in the matrix (Bonnet et al. 2016). Periostin also acts as a ligand for integrins αvβ3 and αvβ5 to promote cell movement by activating actin/myosin contraction mechanisms (Gillan et al. 2002). Thus, periostin interacts directly with ECM proteins, matrix proteins, membrane receptors, growth factors, and cytokines to participate in tissue genesis and remodeling (Kii et al. 2016), (Rangiani et al. 2016), (Cai et al. 2021).
In animal models, periostin expression has been detected during the development of tooth papilla and pulp cells, while it is only expressed in the periodontal ligament and gingiva after birth (Padial-Molina et al. 2015; Rios et al. 2005). In addition, experimental data indicate that periostin may play a role in dental pulp restoration (Ma et al. 2011; Cobo et al. 2019; Zhou et al. 2015). Periostin knockout mice showed heterotopic mineralization and hypermineralized dentin, indicating periostin as a negative stromal mineralization regulator. In addition, periostin exerted a negative regulatory effect on mechanical load and TGF-β stimulation in vitro, substantiating its role as a negative regulator of matrix mineralization (Wiesen et al. 2015). However, it is believed that periostin might play a pivotal role in the regeneration of the periodontal ligament and alveolar bone following periodontal surgery by promoting collagen fibrillogenesis and migration of fibroblasts and osteoblasts (Du and Li 2017). These pieces of evidence indicate that periostin plays a vital role as a regulator of mineralization, but whether it is a positive or negative regulator needs further study.
2 The transforming growth factor (TGF) superfamily
The TGF superfamily is an important growth factor involved in regulating cell differentiation, proliferation and programmed death, with similar high-level protein structures, including TGF-β, bone morphogenetic protein (BMP) and growth differentiation factor (GDF), activator protein (ACT) and inhibitory protein. It has been established that they mediate and transduce signals through their corresponding receptors. TGF and BMP play an important role when odontoblasts secrete ECM and mineralize. BMP regulates the expression of various transcription factors and mediates the interaction between the epithelial and mesenchymal layers during tooth development. Moreover, TGF-βs participate in the regulation of matrix formation and mineralization and regulates the arrangement of odontoblasts.
2.1 BMP family
BMP belongs to the transforming growth factor β superfamily and comprises more than 20 family members. The expression of BMP2, BMP4, and BMP7 can be detected in the tooth epithelium at early stages of tooth initiation. They play important roles in the interaction between the epithelium that induces tooth formation and the mesenchyme (Dong et al. 2014; Balic and Thesleff 2015; Graf et al. 2016). Moreover, they can induce the expression of ameloblast protein, thus promoting the generation of tooth enamel (Greenblatt et al. 2015; Liu et al. 2016a). Furthermore, BMP2, BMP3, BMP4, and BMP7 are expressed in the root (Yamashiro et al. 2003). BMP2 knockout reportedly affects the formation of root and periodontal membrane (Wu et al. 2015) and blocks the development of dentin and tooth enamel in mice (Wu et al. 2015; Yang et al. 2012). BMP4 knockout decreased the expression of Msx1 and Pax9, thus inhibiting the germination of mandibular molars (Jia et al. 2013). Additionally, in vitro studies showed that recombinant human BMP2 could stimulate the differentiation of human dental pulp cells into odontoblasts in monolayers and 3D mass culture systems (Casagrande et al. 2010; Iohara et al. 2004). Similarly, recombinant BMP4 protein could promote the differentiation of exogenous stem cells into ameloblasts or odontoblasts, while recombinant human BMP7 promoted the dental differentiation ability of seed cells in a culture system with scaffold material (Liu et al. 2016b; Jani et al. 2018; Seki et al. 2015; Cho et al. 2016). In addition, BMP9 and BMP11 were found to induce dentin repair or regeneration (Nakashima et al. 2003; Liu et al. 2020; Zhang et al. 2015). Furthermore, Feng et al. confirmed the functional significance of BMP signaling in regulating the fate of endogenous mesenchymal stem cells (MSCs) during root development (Feng et al. 2017). Thus, BMPs play an essential role in tooth germination, dentin formation, and dentin regeneration.
2.2 Transforming growth factor βs (TGF-βs)
TGF-β is a secreted protein established to be a multifunctional growth factor and an essential regulator of craniofacial development and tooth formation (Sassá Benedete et al. 2008; Ripamonti et al. 2016). TGF-β is a dimer composed of two subunits with the same or similar structure and a relative molecular mass of 1.25 × 104 connected by disulfide bonds. It is a polypeptide growth factor with a highly conserved structure and function. The TGF-β subfamily mainly includes three congeners of TGF-β1 to 3, which have similar biological activities and a high degree of homology in amino acid sequences. TGF-β mRNA and its protein are expressed at different stages of tooth germination, from the early bud stage to the formation of root dentin. Using in situ hybridization in a mouse dental development model, TGF-β1 was found to be initially expressed in the dental epithelium and mesenchyme at the cap stage,subsequently, it was also expressed in ameloblasts and odontoblasts and was then found to be continuously expressed in odontoblasts (Okubo et al. 2019; Song et al. 2018). To identify the function of TGF-βs, knockout and overexpression animal models were used. The mandibular molars and incisors of TGF-β1 knockout mice showed severe wear and low density. The enamel column was elongated, and an undegraded enamel matrix protein was observed under electron microscopy (Liu et al. 2019). In transgenic mice overexpressing TGF-β2, an increased rate of hard tissue deposition of dentin was observed, suggesting that TGF-β2 may stimulate the synthesis and deposition of mineralized substrates (Um et al. 2018). Another research group found that exogenous TGF-β2 could induce the overexpression of genes associated with tooth development, such as DSPP in tooth embryos. Interestingly, few studies have reported contradictory findings of significantly reduced dentine elastic modulus accompanied by enamel hypoplasia in TGF-β2 overexpressing mice (Saeki et al. 2007).
TGF-β3 has been reported to be primarily expressed in the stellate network and bell phase and plays a regulatory role in the development of teeth. TGF-β3 can also induce mineralization by up-regulating the expression of OCN and collagen type I (COL1) in odontogenic stem cells and inducing the differentiation of odontogenic stem cells into odontoblasts (Huojia et al. 2005). Moreover, exogenous TGF-β3 promotes the mineralization of endogenous odontogenic stem cells, which may be achieved by activating the MAPK signaling pathway (Li et al. 2019). In vivo experiments showed that a combination of TGF-β3 and DPSCs could effectively promote osseointegration and mineralization of implants (Rizk and Rabie 2013). Thus, TGF-βs, expressed during tooth formation, can induce odontoblast differentiation and functional odontoblast-like cell formation in vitro. In addition, exogenous TGF-β may increase restorative dentin formation by acting on odontoblasts.
The TGF superfamily mediates signals through their corresponding receptors. The signal pathway is composed of the TGF-β1 receptor (TGF-βR1) and type 2 receptor (TGF-βR2) to transduce signals. TGF β II receptor interaction protein 1 (TRIP-1) is a WD-40 protein (WD is tryptophan–aspartic acid dipeptide). Ample evidence suggests that TRIP-1 is synthesized and secreted into the extracellular space by osteoblasts and odontoblasts and is localized in the mineralized ECM during odontogenesis and osteogenesis (Chen and George 2018). Importantly, recombinant TRIP-1 can coordinate the formation of hydroxyapatite crystals. In addition, TRIP-1, at different concentrations, participates in the nucleation of calcium phosphate polymorphism. A nucleation experiment on demineralized and deproteinized dentine chips under physiological conditions showed that TRIP-1 promoted the deposition of calcium phosphate mineral aggregates in the interstitial overlap area of type I collagen (Ramachandran et al. 2018).
Assessment of mesenchymal stem cell function during in vitro experiments showed that the expression of TRIP-1 under the induction of a mineralized culture medium promoted TRIP-1 mineralization and increased the formation of the mineralized matrix. Implantation of TRIP-1 showed high calcium and phosphate deposits, neat rows of collagen fibers, and high expression of mineralization-related molecules Runx2 and ALP in the implanted area (Ramachandran et al. 2016). In addition, the presence of TRIP-1 was detected in proteins secreted by mesenchymal stem cells, suggesting that TRIP-1 may participate in a similar calcium phosphate crystal mineralization process in vivo (Unterbrink et al. 2002). This phenomenon provides a theoretical basis for the tissue regeneration function of TRIP-1.
3 Matrix metalloproteinases (MMPs)
MMPs represent a class of endopeptidases capable of degrading almost all ECM proteins, including natural and deformable forms of different collagen proteins. Overwhelming evidence substantiates the presence of many MMP family members in dentin and predentin, where they play critical roles in dentin formation and mineralization (Mazzoni et al. 2015; Linde and Goldberg 1993). The ECM of dentin, consisting mainly of the organic component type I collagen, may be impaired by proteolytic degradation by collagenases (MMP1, MMP8, MMP13) and gelatinases (MMP2, MMP9) (Toledano et al. 2012; Maciejczyk et al. 2016). In fact, odontogenesis imperfecta is characterized by large amounts of type III collagen in dentin (Kawashima and Okiji 2016; Tjäderhane et al. 2001). Current evidence suggests that MMP1 and MMP8 degrade type III collagen and ensure the preservation of normal dentin (Tjäderhane et al. 2001; Doren 2015). During caries formation, demineralization or degradation of the demineralized organic matrix was found to occur in dentin after the release of MMP20 from dentin, indicating that MMP20 may be involved in the organic matrix tissue during dentin formation (Prajapati et al. 2018; Koli et al. 2015). MMP3 can degrade ECM components, including proteoglycan, fibrinogen, laminin, and type IV collagenase, and activate collagenases. Chen et al. documented a signaling pathway related to MMP3 tooth differentiation in stem cells (Chen et al. 2021). In vivo tests showed that MMP-3 might represent a valuable therapy for treating mild irreversible pulpitis (Eba et al. 2012).
4 Extracellular vesicles (EVs)
EVs are components of the ECM that are small particles of the plasma membrane released from cells into the extracellular space, with a diameter ranging from 30 to 2,000 nm (Rilla et al. 2019). Usually, they contain nucleic acids, proteins, lipids, and signaling molecules. EVs can regulate the synthesis or degradation of matrix molecules by target cells and directly or indirectly alter the composition of the ECM.
As a form of EVs, exosomes play an essential regulatory role in tooth differentiation and tooth regeneration (Jiang et al. 2017; Zhu et al. 2018). The exosomes derived from hDPSCs have been reported to promote odontogenic differentiation of hDPSCs and hBMSCs by activating the P38 MAPK pathway (Huang et al. 2016). Moreover, exosomes from BMSCs promoted periodontal tissue regeneration, while exosomes of odontoblasts promoted the differentiation and mineralization of osteoblasts (Kawai et al. 2015; Kim et al. 2009). Intriguingly, EVs secreted by Schwann cells in the dental pulp could maintain the mutability of hDPSCs (Couve et al. 2018), (Li et al. 2017), suggesting that the nervous system also plays a vital role in tooth regeneration. In addition, EVs derived from mesenchymal stem cells from other tissues may be a crucial source of tooth regeneration.
Stromal vesicles (MVs) are special EVs that play a key role in dentin mineralization (Golub 2009). While other EVs release regulatory factors into other target cells or the ECM, MVs release their bioactive substances into the ECM to change their composition and properties (Chaudhary et al. 2016). The role of MVs in the mineralization of developing hard tissues, such as calcified cartilage, bone, and dentin, has been recognized for the last 50 years, indicating the role of MVs in matrix remodeling (Anderson 1967). At present, Phospho1 and Alpl are known to play essential roles in the formation of MV,in Phospho1-/-,Alpl +/− mice, the number of MVs in the dentine layer was significantly reduced, and the biogenesis of dentin and dentin mineralization was significantly affected (McKee et al. 2013; Yadav et al. 2016). In addition, the research group confirmed that the transcription factor Trps1 could regulate Phospho1 and Alpl expression, thus affecting the MVs secretion of cells, ultimately leading to delayed and reduced mineralization of odontoblasts (Kuzynski et al. 2014). These results indicate that Phospho1 and Alpl play key roles in the formation and secretion of MVs, thus affecting the odontoblast differentiation ability. In another study, knocking out rab27a/b of the GTPase Rab family in tooth embryos resulted in a 20%–40% decrease in MVs secretion of epithelial and mesenchymal cells. Over an extended culture period, it was found that rab27a/b knockout resulted in the loss of the basement membrane components derived from epithelial cells and the weakening of the odontoblast differentiation ability of mesenchymal cells (Jiang et al. 2017). Additionally, in the Rab27 knockout mutant mouse model, a decrease in enamel/dentin matrix synthesis and neck ring size was observed. This evidence suggests that the amount of secreted MVs can influence and determine the formation and biomineralization of dentin.
Moreover, MVs secreted into ECM can interact with ECM macromolecules to influence the mineralization process. MV is generally believed to be the initial site of mineral formation. MV is derived mainly from the plasma membrane of osteoblasts or odontoblasts, which form and transport material from the parent cells. MV mineralization mainly occurs in the dentine mask (Goldberg et al. 2011; Abou Neel et al. 2016). MVs contain TNAP (tissue non-specific alkaline phosphatase), NPP1 (nucleotide pyrophosphatase phosphodiesterase), and AnnexinV (membrane conjugate protein V), three proteins that play essential roles in the process of matrix mineralization. In addition, MVs participates in regulating the concentration of PPi in ECM, and the removal of PPi promotes mineral formation (Golub 2009). There is a rich literature available that reveals that MVs mineralization is mainly carried out in two stages. During the first stage, apatite in MVs is preliminarily formed, Ca2+ and phosphate enter the MV through the Annexin channel and type III Na+ dependent phosphate transporter, respectively, to form apatite crystals (Arispe et al. 1996; Bottini et al. 2018; Wu et al. 2003). During the second stage, the apatite crystal expands and grows in the ECM (Butler et al. 2003),acidic phospholipid and other MV components bind to the apatite crystal, then MV specifically combines with fibrin in the ECM inserting the apatite crystal into the fibrin structure (Jin et al. 2019). MV synergizes with matrix macromolecules, thus causing matrix calcification.
In addition, other substances contained in the EVs can regulate odontogenic differentiation. MMPs, for example, are localized in MVs, where they participate in cell-to-matrix interactions, matrix degradation, and ECM protein remodeling (D’Angelo et al. 2001). Similarly, studies have shown that miR135a, derived from exosomes secreted by epithelial stem cells, can activate Wnt/catenin signaling after endocytosis of target cells, thus activating the differentiation of mesenchymal stem cells (Jiang et al. 2017).
5 Applications
ECM proteins can be divided into bioactive proteins and non-bioactive proteins. Bioactive matrix proteins can promote the odontogenic differentiation of stem cells. At present, most matrix proteins exist in the form of bioactive polypeptides and small molecular preparations, which are injected into the defect to regulate the odontogenic differentiation of endogenous stem cells. In addition, exogenous stem cells can be modified by gene-editing techniques to express bioactive matrix proteins, which can then be implanted into the defective part to promote the odontogenic differentiation of exogenous stem cells. Non-bioactive matrix proteins mainly act as chemotaxis and adhesion to endogenous or exogenous stem cells. Therefore, they are primarily used as components of scaffold materials for transforming growth factor superfamily and degrading enzymes. Most of them are applied in the form of recombinant proteins. They are injected into the defect site, with or without a sustained-release system, to induce the homing of endogenous or exogenous stem cells and to differentiate into odontoblasts to promote tooth tissue regeneration. Given that the components of EVs are complex with heterogeneous sizes, it is too early to achieve standardized production and clinical application.
6 Conclusion
Odontogenic differentiation is a complex process. Regarding tooth tissue regeneration and cell implantation, the ECM environment is known to influence the final differentiation into tooth tissue. Growing evidence suggests that functional ECM components in body tissues, such as ECM proteins, cell factors, degrading enzymes, and extracellular vesicles, can affect the composition and function of the ECM cells to regulate tooth differentiation. Given that the precise regulatory mechanisms remain unclear, their application in clinical practice is limited. Therefore, elucidating the effect of functional ECM on the odontogenic differentiation function of replantation cells is of great significance for the clinical research and application of tooth tissue regeneration. Future studies are expected to focus on the regulatory effect and mechanism of functional ECM on odontogenic differentiation function. Furthermore, identifying different strategies to accurately regulate the odontogenic differentiation ability of the ECM and its cells would provide a theoretical basis and evidence for the clinical application of tooth tissue regeneration.
Availability of data and material
Not applicable.
References
Abou Neel EA, Aljabo A, Strange A, et al. Demineralization-remineralization dynamics in teeth and bone. Int J Nanomedicine. 2016. https://doi.org/10.2147/IJN.S107624.
Alsanea R, Ravindran S, Fayad MI, et al. Biomimetic approach to perforation repair using dental pulp stem cells and dentin matrix protein 1. J Endod. 2011. https://doi.org/10.1016/j.joen.2011.05.019.
Anderson HC. Electron microscopic studies of induced cartilage development and calcification. J Cell Biol. 1967. https://doi.org/10.1083/jcb.35.1.81.
Ao M, Chavez MB, Chu EY, et al. Overlapping functions of bone sialoprotein and pyrophosphate regulators in directing cementogenesis. Bone. 2017. https://doi.org/10.1016/j.bone.2017.08.027.
Arispe N, Rojas E, Genge BR, Wu LN, Wuthier RE. Similarity in calcium channel activity of annexin V and matrix vesicles in planar lipid bilayers. Biophys J. 1996. https://doi.org/10.1016/S0006-3495(96)79377-3.
Balic A, Thesleff I. Tissue interactions regulating tooth development and renewal. Curr Top Dev Biol. 2015. https://doi.org/10.1016/bs.ctdb.2015.07.006.
Baloul SS. Osteoclastogenesis and osteogenesis during tooth movement. Front Oral Biol. 2016. https://doi.org/10.1159/000351901.
Bonnet N, Garnero P, Ferrari S. Periostin action in bone. Mol Cell Endocrinol. 2016. https://doi.org/10.1016/j.mce.2015.12.014.
Boskey AL, Villarreal-Ramirez E. Intrinsically disordered proteins and biomineralization. Matrix Biol. 2016. https://doi.org/10.1016/j.matbio.2016.01.007.
Bottini M, Mebarek S, Anderson KL, et al. Matrix vesicles from chondrocytes and osteoblasts: Their biogenesis, properties, functions and biomimetic models. Biochim Biophys Acta Gen Subj. 2018. https://doi.org/10.1016/j.bbagen.2017.11.005.
Bouleftour W, Juignet L, Bouet G, et al. The role of the SIBLING, Bone Sialoprotein in skeletal biology - Contribution of mouse experimental genetics. Matrix Biol. 2016. https://doi.org/10.1016/j.matbio.2015.12.011.
Butler WT, Brunn JC, Qin C. Dentin extracellular matrix (ECM) proteins: comparison to bone ECM and contribution to dynamics of dentinogenesis. Connect Tissue Res. 2003;44(Suppl 1):171–8.
Cai J, Qin H, Yu G. Effect of periostin silencing on Runx2, RANKL and OPG expression in osteoblasts. Wirkung von Periostin-Silencing auf die Expression von Runx2, RANKL und OPG in Osteoblasten. J Orofac Orthop. 2021. https://doi.org/10.1007/s00056-020-00253-3
Casagrande L, Demarco FF, Zhang Z, Araujo FB, Shi S, Nör JE. Dentin-derived BMP-2 and odontoblast differentiation. J Dent Res. 2010. https://doi.org/10.1177/0022034510364487.
Chaudhary SC, Kuzynski M, Bottini M, et al. Phosphate induces formation of matrix vesicles during odontoblast-initiated mineralization in vitro. Matrix Biol. 2016. https://doi.org/10.1016/j.matbio.2016.02.003.
Chaussain C, Eapen AS, Huet E, et al. MMP2-cleavage of DMP1 generates a bioactive peptide promoting differentiation of dental pulp stem/progenitor cell. Eur Cell Mater. 2009; https://doi.org/10.22203/ecm.v018a08
Chen Y, George A. TRIP-1 promotes the assembly of an ECM that contains extracellular vesicles and factors that modulate angiogenesis. Front Physiol. 2018. https://doi.org/10.3389/fphys.2018.01092.
Chen Y, Zhang Y, Ramachandran A, George A. DSPP is essential for normal development of the dental-craniofacial complex. J Dent Res. 2016. https://doi.org/10.1177/0022034515610768.
Chen Y, Pethö A, Ganapathy A, George A. DPP promotes odontogenic differentiation of DPSCs through NF-κB signaling. Sci Rep. 2021. https://doi.org/10.1038/s41598-021-01359-3.
Cho H, Tarafder S, Fogge M, Kao K, Lee CH. Periodontal ligament stem/progenitor cells with protein-releasing scaffolds for cementum formation and integration on dentin surface. Connect Tissue Res. 2016. https://doi.org/10.1080/03008207.2016.1191478.
Choi YA, Seol MY, Shin HI, Park EK. Bobby Sox homology regulates odontoblast differentiation of human dental pulp stem cells/progenitors. Cell Commun Signal. 2014. https://doi.org/10.1186/1478-811X-12-35.
Cobo T, Cobo JL, Pérez-Varela JC, Vega JA, Cobo J. Periostin and human teeth. Adv Exp Med Biol. 2019. https://doi.org/10.1007/978-981-13-6657-4_8.
Couve E, Lovera M, Suzuki K, Schmachtenberg O. Schwann cell phenotype changes in aging human dental pulp. J Dent Res. 2018. https://doi.org/10.1177/0022034517733967.
D’Angelo M, Billings PC, Pacifici M, Leboy PS, Kirsch T. Authentic matrix vesicles contain active metalloproteases (MMP). a role for matrix vesicle-associated MMP-13 in activation of transforming growth factor-beta. J Biol Chem. 2001; https://doi.org/10.1074/jbc.M009725200
Dong X, Shen B, Ruan N, et al. Expression patterns of genes critical for BMP signaling pathway in developing human primary tooth germs. Histochem Cell Biol. 2014. https://doi.org/10.1007/s00418-014-1241-y.
Du J, Li M. Functions of Periostin in dental tissues and its role in periodontal tissues’ regeneration. Cell Mol Life Sci. 2017. https://doi.org/10.1007/s00018-017-2645-3.
Dye B, Thornton-Evans G, Li X, Iafolla T. Dental caries and tooth loss in adults in the United States, 2011–2012. NCHS Data Brief. 2015 ; PMID: 25973996
Eapen A, Ramachandran A, George A. Dentin phosphoprotein (DPP) activates integrin-mediated anchorage-dependent signals in undifferentiated mesenchymal cells. J Biol Chem. 2012a. https://doi.org/10.1074/jbc.M111.290080.
Eapen A, Ramachandran A, George A. DPP in the matrix mediates cell adhesion but is not restricted to stickiness: a tale of signaling. Cell Adh Migr. 2012b. https://doi.org/10.4161/cam.20627.
Eapen A, Kulkarni R, Ravindran S, et al. Dentin phosphophoryn activates Smad protein signaling through Ca2+-calmodulin-dependent protein kinase II in undifferentiated mesenchymal cells. J Biol Chem. 2013. https://doi.org/10.1074/jbc.M112.413997.
Eba H, Murasawa Y, Iohara K, et al. The anti-inflammatory effects of matrix metalloproteinase-3 on irreversible pulpitis of mature erupted teeth. PLoS One. 2012. https://doi.org/10.1371/journal.pone.0052523.
Ek-Rylander B, Andersson G. Osteoclast migration on phosphorylated osteopontin is regulated by endogenous tartrate-resistant acid phosphatase. Exp Cell Res. 2010. https://doi.org/10.1016/j.yexcr.2009.10.019.
Feng J, Jing J, Li J, et al. BMP signaling orchestrates a transcriptional network to control the fate of mesenchymal stem cells in mice. Development. 2017. https://doi.org/10.1242/dev.150136.
Fisher LW, Torchia DA, Fohr B, Young MF, Fedarko NS. Flexible structures of SIBLING proteins, bone sialoprotein, and osteopontin. Biochem Biophys Res Commun. 2001. https://doi.org/10.1006/bbrc.2000.4146.
Forsprecher J, Wang Z, Goldberg HA, Kaartinen MT. Transglutaminase-mediated oligomerization promotes osteoblast adhesive properties of osteopontin and bone sialoprotein. Cell Adh Migr. 2011. https://doi.org/10.4161/cam.5.1.13369.
Foster BL, Soenjaya Y, Nociti FH, et al. Deficiency in acellular cementum and periodontal attachment in bsp null mice. J Dent Res. 2013. https://doi.org/10.1177/0022034512469026.
Foster BL, Ao M, Willoughby C, et al. Mineralization defects in cementum and craniofacial bone from loss of bone sialoprotein. Bone. 2015. https://doi.org/10.1016/j.bone.2015.05.007.
Frantz C, Stewart KM, Weaver VM. The extracellular matrix at a glance. J Cell Sci. 2010. https://doi.org/10.1242/jcs.023820.
Giachelli CM, Steitz S. Osteopontin: a versatile regulator of inflammation and biomineralization. Matrix Biol. 2000. https://doi.org/10.1016/s0945-053x(00)00108-6.
Gibson MP, Zhu Q, Wang S, et al. The rescue of dentin matrix protein 1 (DMP1)-deficient tooth defects by the transgenic expression of dentin sialophosphoprotein (DSPP) indicates that DSPP is a downstream effector molecule of DMP1 in dentinogenesis. J Biol Chem. 2013. https://doi.org/10.1074/jbc.M112.445775.
Gillan L, Matei D, Fishman DA, Gerbin CS, Karlan BY, Chang DD. Periostin secreted by epithelial ovarian carcinoma is a ligand for alpha(V)beta(3) and alpha(V)beta(5) integrins and promotes cell motility. Cancer Res. 2002;62(18):5358–64.
Goldberg M, Kulkarni AB, Young M, Boskey A. Dentin: structure, composition and mineralization. Front Biosci (elite Ed). 2011. https://doi.org/10.2741/e281.
Golub EE. Role of matrix vesicles in biomineralization. Biochim Biophys Acta. 2009. https://doi.org/10.1016/j.bbagen.2009.09.006.
Graf D, Malik Z, Hayano S, Mishina Y. Common mechanisms in development and disease: BMP signaling in craniofacial development. Cytokine Growth Factor Rev. 2016. https://doi.org/10.1016/j.cytogfr.2015.11.004.
Greenblatt MB, Kim JM, Oh H, et al. p38α MAPK is required for tooth morphogenesis and enamel secretion. J Biol Chem. 2015. https://doi.org/10.1074/jbc.M114.599274.
Gullard A, Gluhak-Heinrich J, Papagerakis S, et al. MEPE localization in the craniofacial complex and function in tooth dentin formation. J Histochem Cytochem. 2016. https://doi.org/10.1369/0022155416635569.
Guo S, Lim D, Dong Z, et al. Dentin sialophosphoprotein: a regulatory protein for dental pulp stem cell identity and fate. Stem Cells Dev. 2014. https://doi.org/10.1089/scd.2014.0066.
He G, Dahl T, Veis A, George A. Nucleation of apatite crystals in vitro by self-assembled dentin matrix protein 1. Nat Mater. 2003. https://doi.org/10.1038/nmat945.
Hoac B, Nelea V, Jiang W, et al. Mineralization-inhibiting effects of transglutaminase-crosslinked polymeric osteopontin. Bone. 2017. https://doi.org/10.1016/j.bone.2017.04.007.
Huang CC, Narayanan R, Alapati S, Ravindran S. Exosomes as biomimetic tools for stem cell differentiation: Applications in dental pulp tissue regeneration. Biomaterials. 2016. https://doi.org/10.1016/j.biomaterials.2016.09.029.
Huojia M, Muraoka N, Yoshizaki K, et al. TGF-beta3 induces ectopic mineralization in fetal mouse dental pulp during tooth germ development. Dev Growth Differ. 2005. https://doi.org/10.1111/j.1440-169x.2005.00790.x.
Icer MA, Gezmen-Karadag M. The multiple functions and mechanisms of osteopontin. Clin Biochem. 2018. https://doi.org/10.1016/j.clinbiochem.2018.07.003.
Iohara K, Nakashima M, Ito M, Ishikawa M, Nakasima A, Akamine A. Dentin regeneration by dental pulp stem cell therapy with recombinant human bone morphogenetic protein 2. J Dent Res. 2004. https://doi.org/10.1177/154405910408300802.
Jani P, Liu C, Zhang H, Younes K, Benson MD, Qin C. The role of bone morphogenetic proteins 2 and 4 in mouse dentinogenesis. Arch Oral Biol. 2018. https://doi.org/10.1016/j.archoralbio.2018.02.004.
Jia S, Zhou J, Gao Y, et al. Roles of Bmp4 during tooth morphogenesis and sequential tooth formation. Development. 2013. https://doi.org/10.1242/dev.081927.
Jia J, Bian Z, Song Y. Dspp mutations disrupt mineralization homeostasis during odontoblast differentiation. Am J Transl Res. 2015;7(11):2379–96.
Jiang N, Xiang L, He L, et al. Exosomes mediate epithelium-mesenchyme crosstalk in organ development. ACS Nano. 2017. https://doi.org/10.1021/acsnano.7b01087.
Jin Y, Long D, Li J, et al. Extracellular vesicles in bone and tooth: A state-of-art paradigm in skeletal regeneration. J Cell Physiol. 2019. https://doi.org/10.1002/jcp.28303.
Kawai T, Katagiri W, Osugi M, Sugimura Y, Hibi H, Ueda M. Secretomes from bone marrow-derived mesenchymal stromal cells enhance periodontal tissue regeneration. Cytotherapy. 2015. https://doi.org/10.1016/j.jcyt.2014.11.009.
Kawashima N, Okiji T. Odontoblasts: Specialized hard-tissue-forming cells in the dentin-pulp complex. Congenit Anom (kyoto). 2016. https://doi.org/10.1111/cga.12169.
Kii I, Nishiyama T, Kudo A. Periostin promotes secretion of fibronectin from the endoplasmic reticulum. Biochem Biophys Res Commun. 2016. https://doi.org/10.1016/j.bbrc.2016.01.139.
Kim HS, Lee DS, Lee JH, et al. The effect of odontoblast conditioned media and dentin non-collagenous proteins on the differentiation and mineralization of cementoblasts in vitro. Arch Oral Biol. 2009. https://doi.org/10.1016/j.archoralbio.2008.09.011.
Koli K, Saxena G, Ogbureke KUE. Expression of matrix metalloproteinase (MMP)-20 and potential interaction with dentin sialophosphoprotein (DSPP) in human major salivary glands. J Histochem Cytochem. 2015. https://doi.org/10.1369/0022155415580817.
Kongkiatkamon S, Ramachandran A, Knoernschild KL, Campbell SD, et al. Dentin matrix protein 1 on titanium surface facilitates osteogenic differentiation of stem cells. Molecules. 2021. https://doi.org/10.3390/molecules26226756.
Kudo A. Periostin in fibrillogenesis for tissue regeneration: periostin actions inside and outside the cell. Cell Mol Life Sci. 2011. https://doi.org/10.1007/s00018-011-0784-5.
Kuzynski M, Goss M, Bottini M, et al. Dual role of the Trps1 transcription factor in dentin mineralization. J Biol Chem. 2014. https://doi.org/10.1074/jbc.M114.550129.
Li Z, Liang Y, Pan K, et al. Schwann cells secrete extracellular vesicles to promote and maintain the proliferation and multipotency of hDPCs. Cell Prolif. 2017. https://doi.org/10.1111/cpr.12353.
Li Y, Qiao Z, Yu F, et al. Transforming growth factor-β3/chitosan sponge (TGF-β3/CS) facilitates osteogenic differentiation of human periodontal ligament stem cells. Int J Mol Sci. 2019. https://doi.org/10.3390/ijms20204982.
Linde A, Goldberg M. Dentinogenesis. Crit Rev Oral Biol Med. 1993. https://doi.org/10.1177/10454411930040050301.
Liu H, Li W, Shi S, Habelitz S, Gao C, Denbesten P. MEPE is downregulated as dental pulp stem cells differentiate. Arch Oral Biol. 2005. https://doi.org/10.1016/j.archoralbio.2005.03.003.
Liu J, Saito K, Maruya Y, et al. Mutant GDF5 enhances ameloblast differentiation via accelerated BMP2-induced Smad1/5/8 phosphorylation. Sci Rep. 2016a. https://doi.org/10.1038/srep23670.
Liu L, Liu YF, Zhang J, Duan YZ, Jin Y. Ameloblasts serum-free conditioned medium: bone morphogenic protein 4-induced odontogenic differentiation of mouse induced pluripotent stem cells. J Tissue Eng Regen Med. 2016b. https://doi.org/10.1002/term.1742.
Liu X, Xu C, Tian Y, et al. RUNX2 contributes to TGF-β1-induced expression of Wdr72 in ameloblasts during enamel mineralization. Biomed Pharmacother. 2019. https://doi.org/10.1016/j.biopha.2019.109235.
Liu L, Chen Y, Song D, Huang D. BMP9 is a potential therapeutic agent for use in oral and maxillofacial bone tissue engineering. Biochem Soc Trans. 2020. https://doi.org/10.1042/BST20200376.
Lok ZSY, Lyle AN. Osteopontin in vascular disease. Arterioscler Thromb Vasc Biol. 2019. https://doi.org/10.1161/ATVBAHA.118.311577.
Ma D, Zhang R, Sun Y, et al. A novel role of periostin in postnatal tooth formation and mineralization. J Biol Chem. 2011. https://doi.org/10.1074/jbc.M110.140202.
MacDougall M, Simmons D, Gu TT, Dong J. MEPE/OF45, a new dentin/bone matrix protein and candidate gene for dentin diseases mapping to chromosome 4q21. Connect Tissue Res. 2002. https://doi.org/10.1080/03008200290000556.
Maciejczyk M, Pietrzykowska A, Zalewska A, Knaś M, Daniszewska I. The significance of matrix metalloproteinases in oral diseases. Adv Clin Exp Med. 2016; https://doi.org/10.17219/acem/30428
Mazzoni A, Tjäderhane L, Checchi V, et al. Role of dentin MMPs in caries progression and bond stability. J Dent Res. 2015. https://doi.org/10.1177/0022034514562833.
McKee MD, Yadav MC, Foster BL, Somerman MJ, Farquharson C, Millán JL. Compounded PHOSPHO1/ALPL deficiencies reduce dentin mineralization. J Dent Res. 2013. https://doi.org/10.1177/0022034513490958.
Merkel A, Chen Y, George A. Endocytic trafficking of DMP1 and GRP78 complex facilitates osteogenic differentiation of human periodontal ligament stem cells. Front Physiol. 2019. https://doi.org/10.3389/fphys.2019.01175.
Minamizaki T, Yoshiko Y. The bioactive acidic serine- and aspartate-rich motif peptide. Curr Protein Pept Sci. 2015. https://doi.org/10.2174/1389203716666150206122839.
Morath I, Hartmann TN, Orian-Rousseau V. CD44: More than a mere stem cell marker. Int J Biochem Cell Biol. 2016. https://doi.org/10.1016/j.biocel.2016.09.009.
Nakashima M, Tachibana K, Iohara K, Ito M, Ishikawa M, Akamine A. Induction of reparative dentin formation by ultrasound-mediated gene delivery of growth/differentiation factor 11. Hum Gene Ther. 2003. https://doi.org/10.1089/104303403764539369.
Okubo M, Chiba R, Karakida T, et al. Potential function of TGF-β isoforms in maturation-stage ameloblasts. J Oral Biosci. 2019. https://doi.org/10.1016/j.job.2018.12.002.
Oldberg A, Franzén A, Heinegård D. The primary structure of a cell-binding bone sialoprotein. J Biol Chem. 1988a;263(36):19430–2.
Oldberg A, Franzén A, Heinegård D, Pierschbacher M, Ruoslahti E. Identification of a bone sialoprotein receptor in osteosarcoma cells. J Biol Chem. 1988b;263(36):19433–6.
Padial-Molina M, Volk SL, Rios HF. Preliminary insight into the periostin leverage during periodontal tissue healing. J Clin Periodontol. 2015. https://doi.org/10.1111/jcpe.12432.
Padovano JD, Ravindran S, Snee PT, Ramachandran A, Bedran-Russo AK, George A. DMP1-derived peptides promote remineralization of human dentin. J Dent Res. 2015. https://doi.org/10.1177/0022034515572441.
Paz J, Wade K, Kiyoshima T, et al. Tissue- and bone cell-specific expression of bone sialoprotein is directed by a 9.0 kb promoter in transgenic mice. Matrix Biol. 2005; https://doi.org/10.1016/j.matbio.2005.05.009
Prajapati S, Ruan Q, Mukherjee K, Nutt S, Moradian-Oldak J. The presence of MMP-20 reinforces biomimetic enamel regrowth. J Dent Res. 2018. https://doi.org/10.1177/0022034517728504.
Qiu SR, Wierzbicki A, Orme CA, et al. Molecular modulation of calcium oxalate crystallization by osteopontin and citrate. Proc Natl Acad Sci U S A. 2004. https://doi.org/10.1073/pnas.0307900100.
Ramachandran A, Ravindran S, Huang CC, George A. TGF beta receptor II interacting protein-1, an intracellular protein has an extracellular role as a modulator of matrix mineralization. Sci Rep. 2016. https://doi.org/10.1038/srep37885.
Ramachandran A, He K, Huang CC, Shahbazian-Yassar R, Shokuhfar T, George A. TRIP-1 in the extracellular matrix promotes nucleation of calcium phosphate polymorphs. Connect Tissue Res. 2018. https://doi.org/10.1080/03008207.2018.1424146.
Rangiani A, Jing Y, Ren Y, Yadav S, Taylor R, Feng JQ. Critical roles of periostin in the process of orthodontic tooth movement. Eur J Orthod. 2016. https://doi.org/10.1093/ejo/cjv071.
Ravindran S, George A. Dentin matrix proteins in bone tissue engineering. Adv Exp Med Biol. 2015. https://doi.org/10.1007/978-3-319-22345-2_8.
Rilla K, Mustonen AM, Arasu UT, Härkönen K, Matilainen J, Nieminen P. Extracellular vesicles are integral and functional components of the extracellular matrix. Matrix Biol. 2019. https://doi.org/10.1016/j.matbio.2017.10.003.
Rios H, Koushik SV, Wang H, et al. periostin null mice exhibit dwarfism, incisor enamel defects, and an early-onset periodontal disease-like phenotype. Mol Cell Biol. 2005. https://doi.org/10.1128/MCB.25.24.11131-11144.2005.
Ripamonti U, Parak R, Klar RM, Dickens C, Dix-Peek T, Duarte R. The synergistic induction of bone formation by the osteogenic proteins of the TGF-β supergene family. Biomaterials. 2016. https://doi.org/10.1016/j.biomaterials.2016.07.018.
Ritchie H. The functional significance of dentin sialoprotein-phosphophoryn and dentin sialoprotein. Int J Oral Sci. 2018. https://doi.org/10.1038/s41368-018-0035-9.
Rizk A, Rabie ABM. Human dental pulp stem cells expressing transforming growth factor β3 transgene for cartilage-like tissue engineering. Cytotherapy. 2013. https://doi.org/10.1016/j.jcyt.2013.01.012.
Rowe PS, de Zoysa PA, Dong R, et al. MEPE, a new gene expressed in bone marrow and tumors causing osteomalacia. Genomics. 2000. https://doi.org/10.1006/geno.2000.6235.
Saeki K, Hilton JF, Alliston T, et al. Elevated TGF-beta2 signaling in dentin results in sex related enamel defects. Arch Oral Biol. 2007. https://doi.org/10.1016/j.archoralbio.2007.01.015.
Saito MT, Silvério KG, Casati MZ, Sallum EA, Nociti FH. Tooth-derived stem cells: Update and perspectives. World J Stem Cells. 2015. https://doi.org/10.4252/wjsc.v7.i2.399.
Salmon B, Bardet C, Khaddam M, et al. MEPE-derived ASARM peptide inhibits odontogenic differentiation of dental pulp stem cells and impairs mineralization in tooth models of X-linked hypophosphatemia. PLoS ONE. 2013. https://doi.org/10.1371/journal.pone.0056749.
Salmon B, Bardet C, Coyac BR, et al. Abnormal osteopontin and matrix extracellular phosphoglycoprotein localization, and odontoblast differentiation. X-Linked Hypophosphatemic Teeth Connect Tissue Res. 2014. https://doi.org/10.3109/03008207.2014.923864.
Sassá Benedete AP, Sobral APV, Lima DMC, Kamibeppu L, Soares FA, Lourenço SV. Expression of transforming growth factor-beta 1, -beta 2, and -beta 3 in human developing teeth: immunolocalization according to the odontogenesis phases. Pediatr Dev Pathol. 2008. https://doi.org/10.2350/07-09-0333.1.
Schrauwen I, Valgaeren H, Tomas-Roca L, et al. Variants affecting diverse domains of MEPE are associated with two distinct bone disorders, a craniofacial bone defect and otosclerosis. Genet Med. 2019. https://doi.org/10.1038/s41436-018-0300-5.
Seki D, Takeshita N, Oyanagi T, et al. Differentiation of odontoblast-like cells from mouse induced pluripotent stem cells by Pax9 and Bmp4 transfection. Stem Cells Transl Med. 2015. https://doi.org/10.5966/sctm.2014-0292.
Sfeir C, Lee D, Li J, Zhang X, Boskey AL, Kumta PN. Expression of phosphophoryn is sufficient for the induction of matrix mineralization by mammalian cells. J Biol Chem. 2011. https://doi.org/10.1074/jbc.M110.209528.
Singh A, Gill G, Kaur H, Amhmed M, Jakhu H. Role of osteopontin in bone remodeling and orthodontic tooth movement: a review. Prog Orthod. 2018. https://doi.org/10.1186/s40510-018-0216-2.
Siyam A, Wang S, Qin C, et al. Nuclear localization of DMP1 proteins suggests a role in intracellular signaling. Biochem Biophys Res Commun. 2012. https://doi.org/10.1016/j.bbrc.2012.07.037.
Sodek J, Ganss B, McKee MD. Osteopontin. Crit Rev Oral Biol Med. 2000. https://doi.org/10.1177/10454411000110030101.
Soenjaya Y, Foster BL, Nociti FH, et al. Mechanical forces exacerbate periodontal defects in Bsp-null mice. J Dent Res. 2015. https://doi.org/10.1177/0022034515592581.
Song W, Wang Y, Chu Q, et al. Loss of transforming growth factor-β1 in epithelium cells affects enamel formation in mice. Arch Oral Biol. 2018. https://doi.org/10.1016/j.archoralbio.2018.09.003.
Suzuki K, Zhu B, Rittling SR, et al. Colocalization of intracellular osteopontin with CD44 is associated with migration, cell fusion, and resorption in osteoclasts. J Bone Miner Res. 2002. https://doi.org/10.1359/jbmr.2002.17.8.1486.
Tanabe H, Takayama I, Nishiyama T, et al. Periostin associates with Notch1 precursor to maintain Notch1 expression under a stress condition in mouse cells. PLoS ONE. 2010. https://doi.org/10.1371/journal.pone.0012234.
Tjäderhane L, Palosaari H, Wahlgren J, Larmas M, Sorsa T, Salo T. Human odontoblast culture method: the expression of collagen and matrix metalloproteinases (MMPs). Adv Dent Res. 2001. https://doi.org/10.1177/08959374010150011401.
Toledano M, Yamauti M, Osorio E, Osorio R. Zinc-inhibited MMP-mediated collagen degradation after different dentine demineralization procedures. Caries Res. 2012. https://doi.org/10.1159/000337315.
Um S, Lee JH, Seo BM. TGF-β2 downregulates osteogenesis under inflammatory conditions in dental follicle stem cells. Int J Oral Sci. 2018. https://doi.org/10.1038/s41368-018-0028-8.
Unterbrink A, O’Sullivan M, Chen S, MacDougall M. TGF beta-1 downregulates DMP-1 and DSPP in odontoblasts. Connect Tissue Res. 2002. https://doi.org/10.1080/03008200290000565.
Van Doren SR. Matrix metalloproteinase interactions with collagen and elastin. Matrix Biol. 2015. https://doi.org/10.1016/j.matbio.2015.01.005.
Verdelis K, Szabo-Rogers HL, Xu Y, et al. Accelerated enamel mineralization in Dspp mutant mice. Matrix Biol. 2016. https://doi.org/10.1016/j.matbio.2016.01.003.
Villarreal-Ramirez E, Eliezer D, Garduño-Juarez R, Gericke A, Perez-Aguilar JM, Boskey A. Phosphorylation regulates the secondary structure and function of dentin phosphoprotein peptides. Bone. 2017. https://doi.org/10.1016/j.bone.2016.10.028.
Wan C, Yuan G, Luo D, et al. The dentin sialoprotein (DSP) domain regulates dental mesenchymal cell differentiation through a novel surface receptor. Sci Rep. 2016. https://doi.org/10.1038/srep29666.
Wei X, Ling J, Wu L, Liu L, Xiao Y. Expression of mineralization markers in dental pulp cells. J Endod. 2007. https://doi.org/10.1016/j.joen.2007.02.009.
Wiesen RM, Padial-Molina M, Volk SL, et al. The expression of periostin in dental pulp cells. Arch Oral Biol. 2015. https://doi.org/10.1016/j.archoralbio.2015.02.008.
Wu LNY, Sauer GR, Genge BR, Valhmu WB, Wuthier RE. Effects of analogues of inorganic phosphate and sodium ion on mineralization of matrix vesicles isolated from growth plate cartilage of normal rapidly growing chickens. J Inorg Biochem. 2003. https://doi.org/10.1016/s0162-0134(03)00003-5.
Wu H, Teng PN, Jayaraman T, et al. Dentin matrix protein 1 (DMP1) signals via cell surface integrin. J Biol Chem. 2011. https://doi.org/10.1074/jbc.M110.194746.
Wu L, Wang F, Donly KJ, et al. Establishment of immortalized mouse Bmp2 knock-out dental papilla mesenchymal cells necessary for study of odontoblastic differentiation and odontogenesis. J Cell Physiol. 2015. https://doi.org/10.1002/jcp.25061.
Yadav MC, Bottini M, Cory E, et al. Skeletal mineralization deficits and impaired biogenesis and function of chondrocyte-derived matrix vesicles in phospho1(-/-) and phospho1/Pi t1 double-knockout mice. J Bone Miner Res. 2016. https://doi.org/10.1002/jbmr.2790.
Yamamoto R, Oida S, Yamakoshi Y. Dentin sialophosphoprotein-derived proteins in the dental pulp. J Dent Res. 2015. https://doi.org/10.1177/0022034515585715.
Yamashiro T, Tummers M, Thesleff I. Expression of bone morphogenetic proteins and Msx genes during root formation. J Dent Res. 2003. https://doi.org/10.1177/154405910308200305.
Yang W, Harris MA, Cui Y, Mishina Y, Harris SE, Gluhak-Heinrich J. Bmp2 is required for odontoblast differentiation and pulp vasculogenesis. J Dent Res. 2012. https://doi.org/10.1177/0022034511424409.
Zhang H, Wang J, Deng F, et al. Canonical Wnt signaling acts synergistically on BMP9-induced osteo/odontoblastic differentiation of stem cells of dental apical papilla (SCAPs). Biomaterials. 2015. https://doi.org/10.1016/j.biomaterials.2014.11.007.
Zhao Z, Liu HC, Huang ZN, et al. The effect of different factors on forming-dentin differentiation of rat dental mesenchymal cells. Shanghai Kou Qiang Yi Xue. 2014; PMID: 25636278.
Zhou M, Kawashima N, Suzuk N, et al. Periostin is a negative regulator of mineralization in the dental pulp tissue. Odontology. 2015. https://doi.org/10.1007/s10266-014-0152-7.
Zhu B, Suzuki K, Goldberg HA, et al. Osteopontin modulates CD44-dependent chemotaxis of peritoneal macrophages through G-protein-coupled receptors: evidence of a role for an intracellular form of osteopontin. J Cell Physiol. 2004. https://doi.org/10.1002/jcp.10394.
Zhu Y, Zhang P, Gu RL, Liu YS, Zhou YS. Origin and clinical applications of neural crest-derived dental stem cells. Chin J Dent Res. 2018. https://doi.org/10.3290/j.cjdr.a40435.
Zhu YS, Gu Y, Jiang C, Chen L. Osteonectin regulates the extracellular matrix mineralization of osteoblasts through P38 signaling pathway. J Cell Physiol. 2020. https://doi.org/10.1002/jcp.29131.
Zohar R, Suzuki N, Suzuki K, et al. Intracellular osteopontin is an integral component of the CD44-ERM complex involved in cell migration. J Cell Physiol. 2000. https://doi.org/10.1002/(SICI)1097-4652(200007)184:1%3c118::AID-JCP13%3e3.0.CO;2-Y.
Acknowledgements
Not applicable
Funding
This work was supported by the National Sciences Foundation of China (81625005 to Z.P.F.), CAMS Innovation Fund for Medical Sciences (2019-I2M-5-031 to Z.P.F.), and the Program for “Hundred-Thousand-Ten Thousand” Talents in Beijing (2018A16 to Z.P.F.).
Author information
Authors and Affiliations
Contributions
Haoqing Yang conceptualized the review. Haoqing Yang prepared the table. Haoqing Yang and Zhipeng Fan revised the manuscript. Zhipeng Fan supervised the work. All authors contributed to writing the manuscript and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. Author Zhipeng Fan is an Associate Editor for Current Medicine. The paper was handled by the other Editor and has undergone rigrous peer review process. Author Zhipeng Fan was not involved in the journal's review of, or decisions related to, this manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yang, H., Fan, Z. The functional extracellular matrix on the regulation of odontogenic differentiation of stem cells. Curr Med 1, 10 (2022). https://doi.org/10.1007/s44194-022-00012-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44194-022-00012-z