Abstract
Background
Human interferon-α1b (hIFN-α1b) is the first genetically engineered drug approved by the National Medical Product Administration for cancer therapy in China. hIFN-α1b is a relatively safe therapy and can improve survival in advanced melanoma and its long-term efficacy against resection of stage III melanoma is unknown.
Objective
The objective of this study is to assess the safety and efficacy of hIFN-α1b in patients with resected stage III melanoma.
Methods
The clinical data were collected from patients who underwent resection of stage IIIB or IIIC melanoma and received subcutaneous injection of hIFN-α1b every other day. The efficacy of hIFN-α1b was determined by rate of recurrence-free survival (RFS), distant metastasis-free survival (DMFS) and overall survival (OS). Safety data were acquired by review of adverse events at follow-ups.
Results
The study included a total of 61 patients. The median follow-up duration was 45 months. The RFS at 12, 24, and 36 months were observed to be 75.4%, 47.4%, and 37.2% respectively, while the DMFS rates were found to be 83.6%, 65.5%, and 62.2%. Furthermore, the OS rates at these time points were recorded as being 100%, 81.9%, and 71.5%. The overall tolerability of hIFN-α1b was satisfactory, with only 8.2% of the patients experiencing grade 3/4 toxicity and no treatment-related deaths observed.
Conclusion
Our findings suggest that adjuvant hIFN-α1b treatment is relatively safe and may potentially enhance the rate of RFS, DMFS and OS in patients who have undergone resection for stage IIIB or IIIC melanoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The patients diagnosed with stage III melanoma are at an elevated risk of recurrence and ultimately succumb to metastatic melanoma following locoregional resection. In recent years, the treatment landscape for stage III melanoma has undergone a remarkable transformation with the advent of targeted therapies, such as BRAF inhibitors (BRAFi) and MEK inhibitors (MEKi), as well as immune checkpoint inhibitors (ICIs), including programmed death protein-1 (PD-1) inhibitor alone or in combination with CTLA-4 inhibitor [1]. However, in the systematic management of metastatic melanoma, it has been observed that certain patients exhibit primary or secondary resistance to the aforementioned drug therapy [2]. Furthermore, in the Asian population, acral and mucosal melanoma are the predominant subtypes for which the application of ICIs do not appear to offer promising prospects [3]. Similarly, it is important to note that the utilization of BRAFi and MEKi in melanoma treatment among Asian populations has encountered obstacles due to the relatively low prevalence of BRAF mutation in Asian melanoma patients [4]. Therefore, this suggests the existence of a subset of patients who may not respond to current adjuvant therapies, highlighting the imperative to identify additional therapeutic strategies, for enhancing treatment outcomes among Asian melanoma patients.
Human IFN-α1b is approved by the National Medical Product Administration for melanoma therapy in China. The systemic administration of hIFN-α1b is a relatively safe therapeutic approach that has the potential to extend the survival of patients with unresectable metastatic melanoma, while exhibiting a lower incidence of serious adverse reactions compared to ICI and interferon-α2b (IFN-α2b) [5, 6]. Based on these promising findings, we conducted a retrospective analysis to evaluate the efficacy and safety of hIFN-α1b in patients who underwent surgical resection for stage IIIB or IIIC melanoma.
2 Methods
2.1 Patient selection and data collection
The data on patients who underwent locoregional resection and were histopathologically diagnosed with stage IIIB or IIIC melanoma between July 2009 and December 2020 was collected from the melanoma database of the Department of Dermatology at Xijing Hospital. This Study is reported as per the STROBE guideline (S1 STROBE Checklist). The study has obtained approval from the Institutional Ethics Committee at the Fourth Military Medical University. The study included patients who had received adjuvant hIFN-α1b therapy for a minimum duration of one month. The patients excluded from the study were those with unknown primary sites and those who had previously received other adjuvant therapy. The demographic and clinical information, including age, gender, date of diagnosis, primary tumor site, and stage, is recorded. The primary tumor sites were categorized as acral (the glabrous skin of the palms, soles, and nail beds), cutaneous (non-glabrous skin), and mucosal [7]. The tumor stage of each patient was determined in accordance with the seventh edition of the American Joint Committee on Cancer (AJCC) Cancer Staging Manual [8]. The safety data were obtained through the examination of adverse events during follow-up periods.
2.2 Treatment schedule
The human IFN-α1b (Hapgen, 50 µg/ml, 5 × 106 U/ml, specific activity 1.41 × 108 IU/mg tested in Madin-Darby bovine kidney cells) was administered subcutaneously every alternate day.
2.3 Assessments
Physical examination, complete blood count, and serum biochemical tests were performed prior to the therapy and at 3-month intervals. Patients underwent ultrasound evaluation of all lymph nodes and CT scans of the chest, abdomen, and pelvis at baseline and every 3 months for assessment of recurrence and distant metastases. Recurrence or metastatic lesions were confirmed through histopathological examination when possible. RFS was defined as the duration from diagnosis until the date of initial recurrence (local, regional, or distant metastasis) or death from any cause, while DMFS was defined as the duration from diagnosis to the date of initial distant metastasis or death. OS was defined as the duration from diagnosis until death from any cause. For patients without any event, follow-up was censored at the latest disease evaluation. The assessment of treatment-related adverse events was conducted in accordance with version 5.0 of the National Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE) [9].
2.4 Dose modification for adverse events
The dose was reduced by 33% of the initial dosage following the first instance of severe adverse events, and by 66% after the second occurrence. Treatment discontinuation was warranted upon the third dose-limiting adverse event [9].
2.5 Statistical analysis
The Kaplan-Meier method was utilized to estimate the rates of RFS, DMFS, and OS, which were then compared using the log-rank test. Univariate Cox hazard analysis was conducted to identify factors associated with RFS, DMFS or OS. A P value < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS software (SPSS, Chicago, IL, USA).
3 Results
3.1 Patients and treatment
Sixty-one patients were enrolled in the present study (Fig. 1). The baseline characteristics of the cohort are summarized in Table 1. The median age of the cohort was 55 years (range: 23–76 years), with males accounting for 37.7% (n = 23) of the patients. Regarding stage classification, 36.1% (n = 22) and 63.9% (n = 39) of the patients were categorized as stage IIIB and stage IIIC, respectively. As for the primary lesional site, 52.5% (n = 32) of the patients were cutaneous melanoma, while acral and mucosal melanoma accounted for 42.6% (n = 26) and 4.9% (n = 3), respectively. In terms of the treatment dosage of hIFN-α1b, the low dose cohort comprised 44.3% (n = 27) of the patients, whereas the high dose cohort consisted of 55.7% (n = 34). The completion lymph node dissection (CLND) was performed in 32.8% (n = 20) of patients, while therapeutic lymph node dissection (TLND, lymphadenectomy for palpable disease) was conducted in an equal proportion of patients (32.8%, n = 20). The remaining 21 patients (34.4%) were diagnosed with stage III based on the presence of in transit metastases or satellites without metastatic nodes, and therefore did not undergo relevant surgical intervention. The median follow-up duration, as of the cutoff date of April 1, 2022, was 45 months (ranging from 13 to 100 months).
3.2 Clinical response
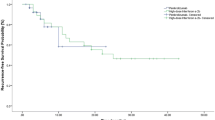
The occurrence of local recurrence and regional metastases was observed in 26 patients (42.6%), while distant metastases were found in 18 patients (29.5%). Additionally, progressive melanoma led to the death of 26 patients (42.6%). The rates of RFS at 12, 24, and 36 months were observed to be 75.4% (95% confidence interval [CI] 62.6–84.4), 47.4% (34.5–59.3), and 37.2% (25.2–49.2) respectively (Fig. 2A). The 12-month RFS rates for stage IIIB and IIIC groups were observed to be 63.6% (40.3–79.9) and 82.1% (66.0–91.0), respectively, while the corresponding rates at 24 months were found to be 45.5% (24.4–64.3) and 48.6% (32.3–63.1). Furthermore, at the end of the observation period (36 months), RFS rates stood at 35.8% (16.8–55.3) for stage IIIB group and at 37.8% (22.8–52.7) for stage IIIC group (Fig. 2B).
The 12-month, 24-month, and 36-month DMFS rates were observed to be 83.6% (95% CI 71.7–90.8), 65.5% (52.2–76.0), and 62.2% (48.8–73.0) respectively (Fig. 3A). The 12-month DMFS rates were 72.7% (58.7–96.4) and 89.7% (74.9–96.0) in stage IIIB and IIIC, respectively, while the 24-month DMFS rates were 54.5% (32.1–72.4) and 71.8% (54.9–83.3). Furthermore, the 36-month DMFS rates in stage IIIB and IIIC were observed to be 54.5% (32.1–72.4) and 66.5% (49.3–79.0, Fig. 3B). The OS rates at 12, 24, and 36 months were recorded as 100%, 81.9% (69.7–89.5), and 71.5% (58.1–81.2) respectively (Fig. 4).
The univariate Cox hazard analysis was performed for RFS, DMFS, and OS based on factors including gender, age, primary tumor sites, lymph node dissection status, AJCC stage, dose administration, and presence or absence of ulceration. The aforementioned analysis revealed no statistically significant factors associated with RFS (Table 2). Patients who did not undergo lymph node surgery (diagnosed based on the presence of in transit metastases or satellites without metastatic nodes) demonstrated a significant increase in DMFS (Hazard rate [HR] = 0.236, P = 0.027) (Supplementary Table S1 and S2). Conversely, the presence of ulceration was associated with decreased DMFS (HR = 5.296, P = 0.024) and OS (HR = 5.220, P = 0.029) (Supplementary Table S2). Other factors were not significantly with RFS, DMFS and OS.
3.3 Toxicity evaluation
The results presented in Table 3 indicate that a total of 58 patients (95.1%) experienced adverse events related to the treatment, with the majority being classified as mild or moderate in intensity. Grade 3 and grade 4 toxicities were observed in 6.6% (n = 4) and 1.6% (n = 1) of the patients, respectively, while no treatment-related death was documented within the cohort. Grade 3 toxicities included fever (n = 3), and stomatitis (n = 1). The Grade 4 toxic case, characterized by an initial elevation in aspartate aminotransferase levels upon treatment initiation without affecting subsequent therapy, returned to normal following oral administration of polyene phosphatidylcholine. The occurrence of grade 3/4 toxicities was observed in four patients receiving low dosages and one patient receiving high dosages.
The most frequently reported adverse event was fever, which occurred in 67.2% (n = 41) of the patients. Three patients developed grade 3 fever all from the 300 µg treatment dose group. The occurrence of fever is commonly observed during the initial two administrations and can be mitigated by the administration of celecoxib. The second most frequently reported adverse event, fatigue, was observed in 31.2% (n = 19) of the patients. Nausea was observed in 6.6% (n = 4) of the patients, while mild or moderate anorexia was experienced by 9.8% (n = 6) of the patients. The occurrence of mood changes was infrequent, as only three patients exhibited indications of depression. The incidence rate of vitiligo, a dermatological event, was found to be 9.8% (n = 6). Alopecia was observed in 13.1% (n = 8) of the patients. Typically, alopecia manifested within 1 to 3 months after treatment initiation.
Hematological and biochemical toxicities were also observed in this study, with 26.2% (n = 16) of the patients experiencing a decrease in lymphocyte count and 3.3% (n = 2) experiencing anemia. The levels of alanine aminotransferase and aspartate aminotransferase were found to be increased in 3.3% (n = 2) and 1.6% (n = 1) of the patients, respectively.
4 Discussion
Our research indicates that hIFN-α1b adjuvant therapy is both efficacious and safe for patients with resected stage IIIB or IIIC melanoma, as demonstrated by favorable rates of RFS, DMFS, and OS. The treatment was generally well-tolerated, with only 8.2% of patients experiencing grade 3/4 toxicity and no instances of treatment-related mortality.
Interferon alpha (IFN-α), a member of the type I interferon family of cytokines, consists of several subtypes, which can mediate antiviral, antiproliferative, antitumor, and immune-modulating effect [10]. The amino acid sequences in IFN-α1b exhibit an 80% homology to IFN-α2b, which was the first drug approved worldwide for the treatment of melanoma [11]. Our group previously reported that hIFN-α1b enhanced the anticancer activity of natural killer cells, natural killer T cells, and CD3 + CD8 + T cells isolated from melanoma patients, and exhibited a more potent inhibitory effect on melanoma cell growth compared to IFN-a2b [12]. The prospective clinical study data demonstrated that IFN-α1b exhibited potent gene modulatory effects on IFN-stimulated genes, demonstrated favorable tolerance and elicited anti-tumor responses in cancer patients, thereby establishing its potential for clinical application in melanoma treatment [13]. The efficacy and safety of hIFN-α1b in treating advanced melanoma have been demonstrated in two retrospective studies conducted by our group. hIFN-α1b monotherapy exhibited favorable tolerability among patients with stage IV melanoma, resulting in a mOS of 14.1 months [5]. Another retrospective study analyzed patients with stage IV melanoma who underwent combination therapy involving hIFN-α1b and PD-1 inhibitor. The objective response rate was found to be 32.8%. The mOS was determined to be 18 months, while only 8.6% of the cases experienced grade 3/4 adverse events [6]. Therefore, in terms of efficacy, the survival improvement observed in advanced melanoma patients treated with hIFN-α1b clearly surpasses the reported data for IFN-α2b [14]. More importantly, although the adverse event profiles of IFN-α1b and IFN-α2b were similar, the incidence of serious adverse events (SAEs) was relatively low with IFN-α1b.
In the present study, the hIFN-α1b further exhibits promising potential as a viable option for resected stage III melanoma, with a 12-month RFS rate of 75.4%. This rate is comparable to the pembrolizumab group’s 12-month RFS rate of 75.3% and surpasses the placebo group’s 12-month RFS rate of 60.0% in KEYNOTE- 054 [15]. Furthermore, it outperforms ipilimumab (63.5%) and placebo (56.1%) in terms of their respective RFS rates at the same time point, as reported in EORTC-18,071 [16]. Moreover, in our cohort, the 12-month and 36-month DMFS rate was 83.6% and 62.2%, which demonstrated comparability to the pembrolizumab group’s 12-month and 36-month DMFS rate of 82.8% and 68.2% and superiority over the placebo group’s 12-month and 36-month DMFS rate of 69.8% and 51.5% observed in KEYNOTE-054 [15]. In our cohort, the OS rates at 12 and 36 months were 100% and 71.5%, respectively, surpassing the corresponding 12-month OS rates of the nivolumab group (95.9%), pembrolizumab group (98.2%), and dabrafenib plus trametinib group (96.9%) in a real-world study, as well as exceeding the reported 36-month OS rate of 64.9% from a retrospective study analyzing data of patients diagnosed during 2013–2014 in the era of novel melanoma therapies [17, 18].
The RFS rates at 24 months (47.4%) and 36 months (37.2%) for hIFN-α1b were notably lower when compared to the rates observed in the KEYNOTE-054 trial for pembrolizumab (68%, 63.7%) and in the EORTC-18,071 trial for ipilimumab (51.5%, 46.5%) [16, 19]. The DMFS rates at 24 months in our cohort (65.5%) were also lower than those of pembrolizumab in the KEYNOTE-054 trial (73.5%) [15]. This discrepancy can be attributed to TLND experienced by some patients in our cohort, whereas all patients underwent CLND in the aforementioned studies with pembrolizumab and ipilimumab treatment regimens employed respectively. Furthermore, it is worth noting that our cohort lacked stage IIIA patients who typically have a relatively favorable prognosis, unlike their inclusion within the above two studies.
Safety is a crucial consideration in the formulation of adjuvant therapy strategies. In the context of immunotherapy, it is noteworthy that over 50% of patients undergoing combination therapy with ipilimumab and nivolumab necessitate immunosuppressive treatment. Although rare, there have been reported instances of treatment-related fatalities [20]. The European Medicines Agency (EMA) conducted a pooled analysis of safety data, reviewing a total of 1,551 patients included in the pivotal CheckMate 037, 066, 06 and 069 trials [20,21,22,23]. The combination of ipilimumab plus nivolumab resulted in severe adverse events (CTCAE grade 3/4) in 54% of patients, while nivolumab alone led to such events in 14% of patients, and ipilimumab alone caused them in 27% [24]. Overall, there were five treatment-related fatalities, with three occurring among those receiving ipilimumab plus nivolumab. The causes of death included pneumonitis, ventricular arrhythmia, cardiac arrest, neutropenia, and one sudden death with an unclear etiology [8]. However, within our cohort study group, only 8.2% (n = 5) of the patients experienced grade 3/4 toxicities without any instances of grade 5 toxicities or treatment-related deaths.
Encouragingly, our preliminary data suggest that the efficacy and safety of IFN-α1b adjuvant monotherapy in patients with stage IIIB or IIIC melanoma is comparable to the results reported by the KEYNOTE054 trial and EORTC18071. It also demonstrates a substantial improvement in long-term patient survival. In addition, as we have observed previously in systemic therapy, the therapy was generally safe. Therefore, we posit that IFN-α1b could serve as a novel alternative to ICIs for adjuvant monotherapy in patients diagnosed with stage IIIB or IIIC melanoma. The current study, however, should be noted for its relatively small sample size, underscoring the necessity for further validation through a prospective study encompassing a larger cohort. In addition, the present study exclusively focused on Chinese patients; therefore, caution should be exercised when extrapolating our findings to cohorts of different ethnic backgrounds. Moreover, our previous study had shown that combination of hIFN-α1b and PD‑1 monoclonal antibody increased objective response rates and prolong the overall survival in stage IV melanoma. Therefore, the future of melanoma treatment may lie in combinational approaches and the combination of hIFN-α1b and PD-1 antibody to treat resected melanoma is worth studying.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- hIFN-α1b:
-
Human interferon-α1b
- RFS:
-
Recurrence-free survival
- DMFS:
-
Distant metastasis-free survival
- OS:
-
Overall survival
- ICIs:
-
Immune checkpoint inhibitors
- PD-1:
-
Programmed death protein-1
- IFN-α2b:
-
Interferon-α2b
- AJCC:
-
American joint committee on cancer
- CTCAE:
-
National cancer institute common terminology criteria for adverse events
- CLND:
-
Completion lymph node dissection
- TLND:
-
Therapeutic lymph node dissection
- CI:
-
Confidence interval
- HR:
-
Hazard ratio
- IFN-α:
-
Interferon alpha
References
Namikawa K, Yamazaki N. Targeted therapy and immunotherapy for melanoma in Japan. Curr Treat Options Oncol. 2019;20(1):7. https://doi.org/10.1007/s11864-019-0607-8.
Morad G, Helmink BA, Sharma P, et al. Hallmarks of response, resistance, and toxicity to immune checkpoint blockade. Cell. 2022;185(3):576. https://doi.org/10.1016/j.cell.2022.01.008.
Mao L, Qi Z, Zhang L, et al. Immunotherapy in acral and mucosal melanoma: current status and future directions. Front Immunol. 2021;12:680407. https://doi.org/10.3389/fimmu.2021.680407.
Rabbie R, Ferguson P, Molina-Aguilar C, et al. Melanoma subtypes: genomic profiles, prognostic molecular markers and therapeutic possibilities. J Pathol. 2019;247(5):539–51. https://doi.org/10.1002/path.5213.
Shi Q, Liu L, Zhang W, et al. Interferon-α1b for the treatment of metastatic melanoma: results of a retrospective study. Anticancer Drugs. 2021;32(10):1105–10. https://doi.org/10.1097/cad.0000000000001120.
Zhu G, Shi Q, Zhao B, et al. Efficacy and safety of interferon-alpha 1b combined with PD-1 monoclonal antibody in patients with unresectable stage IV melanoma: a retrospective study. J Cancer Res Clin Oncol. 2023;149(9):6263–9. https://doi.org/10.1007/s00432-023-04596-3.
Collins LK, Chapman MS, Carter JB, et al. Cutaneous adverse effects of the immune checkpoint inhibitors. Curr Probl Cancer. 2017;41(2):125–8. https://doi.org/10.1016/j.currproblcancer.2016.12.001.
Kähler KC, Hassel JC, Heinzerling L, et al. Side effect management during immune checkpoint blockade using CTLA-4 and PD-1 antibodies for metastatic melanoma - an update. J Dtsch Dermatol Ges. 2020;18(6):582–609. https://doi.org/10.1111/ddg.14128.
Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47. https://doi.org/10.1016/j.ejca.2008.10.026.
Xu P, Chen X, Xu Y, et al. Trastuzumab in combination with PEGylated interferon-α1b exerts synergistic antitumor activity through enhanced inhibition of HER2 downstream signaling and antibody-dependent cellular cytotoxicity. Am J Cancer Res. 2022;12(2):549–61.
Weissmann C, Nagata S, Boll W, et al. Structure and expression of human IFN-alpha genes. Philos Trans R Soc Lond B Biol Sci. 1982;299(1094):7–28. https://doi.org/10.1098/rstb.1982.0102.
Liu Y, Ma J, Yang Y, et al. Impact of Interferon-alpha1b (IFN-α1b) on antitumor immune response: an interpretation of the promising therapeutic effect of IFN-alpha1b on melanoma. Med Sci Monit. 2020;26:e922790. https://doi.org/10.12659/msm.922790.
Masci P, Olencki T, Wood L, et al. Gene modulatory effects, pharmacokinetics, and clinical tolerance of interferon-alpha1b: a second member of the interferon-alpha family. Clin Pharmacol Ther. 2007;81(3):354–61. https://doi.org/10.1038/sj.clpt.6100081.
Agarwala SS, Lee SJ, Yip W, et al. Phase III randomized study of 4 weeks of high-dose interferon-α-2b in stage T2bNO, T3a-bNO, T4a-bNO, and T1-4N1a-2a (microscopic) melanoma: a trial of the Eastern Cooperative Oncology Group-American College of Radiology Imaging Network Cancer Research Group (E1697). J Clin Oncol. 2017;35(8):885–92. https://doi.org/10.1200/jco.2016.70.2951.
Eggermont AMM, Blank CU, Mandalà M, et al. Adjuvant pembrolizumab versus placebo in resected stage III melanoma (EORTC 1325-MG/KEYNOTE-054): distant metastasis-free survival results from a double-blind, randomised, controlled, phase 3 trial. Lancet Oncol. 2021;22(5):643–54. https://doi.org/10.1016/s1470-2045(21)00065-6.
Eggermont AM, Chiarion-Sileni V, Grob JJ, et al. Adjuvant ipilimumab versus placebo after complete resection of high-risk stage III melanoma (EORTC 18071): a randomised, double-blind, phase 3 trial. Lancet Oncol. 2015;16(5):522–30. https://doi.org/10.1016/s1470-2045(15)70122-1.
Schumann K, Mauch C, Klespe KC, et al. Real-world outcomes using PD-1 antibodies and BRAF + MEK inhibitors for adjuvant melanoma treatment from 39 skin cancer centers in Germany, Austria and Switzerland. J Eur Acad Dermatol Venereol. 2023;37(5):894–906. https://doi.org/10.1111/jdv.18779.
Song Y, Tieniber AD, Gimotty PA, et al. Survival outcomes of patients with clinical stage III melanoma in the era of novel systemic therapies. Ann Surg Oncol. 2019;26(13):4621–30. https://doi.org/10.1245/s10434-019-07599-y.
Eggermont AMM, Blank CU, Mandala M, et al. Longer follow-up confirms recurrence-free survival benefit of adjuvant pembrolizumab in high-risk stage III melanoma: updated results from the EORTC 1325-MG/KEYNOTE-054 trial. J Clin Oncol. 2020;38(33):3925–36. https://doi.org/10.1200/jco.20.02110.
Hodi FS, Chiarion-Sileni V, Gonzalez R, et al. Nivolumab plus ipilimumab or nivolumab alone versus ipilimumab alone in advanced melanoma (CheckMate 067): 4-year outcomes of a multicentre, randomised, phase 3 trial. Lancet Oncol. 2018;19(11):1480–92. https://doi.org/10.1016/s1470-2045(18)30700-9.
Weber JS, D’Angelo SP, Minor D, et al. Nivolumab versus chemotherapy in patients with advanced melanoma who progressed after anti-CTLA-4 treatment (CheckMate 037): a randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2015;16(4):375–84. https://doi.org/10.1016/s1470-2045(15)70076-8.
Robert C, Long GV, Brady B, et al. Five-year outcomes with nivolumab in patients with wild-type BRAF advanced melanoma. J Clin Oncol. 2020;38(33):3937–46. https://doi.org/10.1200/jco.20.00995.
Hodi FS, Chesney J, Pavlick AC, et al. Combined nivolumab and ipilimumab versus ipilimumab alone in patients with advanced melanoma: 2-year overall survival outcomes in a multicentre, randomised, controlled, phase 2 trial. Lancet Oncol. 2016;17(11):1558–68. https://doi.org/10.1016/s1470-2045(16)30366-7.
Hassel JC, Heinzerling L, Aberle J, et al. Combined immune checkpoint blockade (anti-PD-1/anti-CTLA-4): evaluation and management of adverse drug reactions. Cancer Treat Rev. 2017;57:36–49. https://doi.org/10.1016/j.ctrv.2017.05.003.
Acknowledgements
The authors would like to express our gratitude to all of the participants for their cooperation and to all of the staff.
Funding
This study was funded by National Natural Science Foundation of China (No. 82273716), National Key Research and Development Program of China (2021YFA1101003), Young Eagle Project of Fourth Military Medical University (No. 2020cyjhsq), and National Natural Science Foundation of China (No. 82172607 and 82273182).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Meiyan Gao, Yuehua Li, Wenjing Tang. The first draft of the manuscript was written by Meiyan Gao and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approval for the study was granted by the Ethics Committee of the Fourth Military Medical University (approval no.KY20151214-3), and it was conducted in accordance with the 1964 Helsinki Declaration and comparable ethical standards. Informed consent was waived by our Institutional Review Board due to the retrospective nature of the study.
Consent for publication
All authors approval for submission.
Competing Interests
The authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gao, M., Li, Y., Tang, W. et al. Real-world clinical outcome and safety of adjuvant human Interferon-alpha1b in resected stage IIIB or IIIC melanoma: results of a retrospective study. Holist Integ Oncol 3, 21 (2024). https://doi.org/10.1007/s44178-024-00087-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44178-024-00087-8