Abstract
Anterior longitudinal ligament and annulus fibrosus removal in total disc replacement induces excessive spinal mobility with zygapophyseal joint overload and osteoarthritic changes causing chronic back pain. To control disc arthroplasty-induced hypermobility with a Kevlar® band. A 3 × 3 cm Kevlar® band implanted in twelve human lumbar cadaveric spines substituted the anterior longitudinal ligament and annulus in disc arthroplasty. Biomechanical studies compared the intact spine, after discectomy, post-disc arthroplasty, and with the Kevlar® band inserted. The Kevlar® band recovered the extension and axial rotation movement ranges without regaining the intact status. Improvement was moderate in lateral bending. The Instantaneous Axis of Rotation improved the discectomy and total disc prosthesis conditions without recovering the initial state. The disc above the operated one also showed increased mobility, particularly in extension and axial rotation, improved by Kevlar® band insertion without recovering the intact spine values. The Kevlar® band improves excess mobility ranges induced by anterior longitudinal ligament and anterior annulus removal in disc arthroplasty in the operated and supra-adjacent discs without recovering the baseline status.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Low back pain is a highly prevalent ailment [1,2,3] and a frequent cause of temporary sick leave and permanent disability [4,5,6]. It has dear consequences for the quality of life [7] and often restricts professional career progression [8,9,10].
When medical treatment is ineffective [11,12,13,14,15], surgery is an option, with discectomy, spinal fusion [16, 17], or disc arthroplasty [18]. Unfortunately, all three change spine column biomechanics, inducing medium and long-term index or adjacent level overload with disc degeneration and zygapophyseal osteoarthritic changes [7, 18], often requiring a new operation [7, 19].
Arthroplasty, compared to spinal arthrodesis [20,21,22], has a higher chance of returning to the same job [20, 23], a better quality of life [24, 25], a lower incidence of adjacent level disease [11,12,13, 22] and fewer reoperations [14]. Still, excessive spinal mobility [15,16,17] is associated with index [26] and adjacent level [27] zygapophyseal joint osteoarthritic changes, which can cause chronic low back pain [28]. This side effect is more prominent the more comprehensive the movement range (Charitè) [29, 30] and when the rotation axis is not within the disc posterior third (Prodisc™ [31], Activ-L™ [32]).
Total disc prosthesis implantation requires removing the anterior longitudinal ligament (ALL) and 2.5–3 cm of the annulus fibrous anterior part (AFAP) [33,34,35], structures that limit the extension, and axial rotation spine movement ranges [36]. As a result, once implanted, all total disc prostheses, no matter their design, allow excessive spinal mobility, particularly in these two axes [15,16,17], which causes index-level zygapophyseal joint overload with degeneration and osteoarthritic changes [37]. The postoperative scarring may somehow reduce this excessive mobility, but nobody proves if this happens and to what extent. The studies available are in finite element models [38,39,40,41] or cadaveric human lumbar spine specimens [42, 43] but not in patients.
Repairing ALL and AFAP is not technically simple. Most studies fix annular defects 3–6 mm in diameter [44,45,46,47,48], typical of a discectomy [49, 50]. Contrariwise, a lumbar disc arthroplasty needs a 2.5–3 × 0.8 cm annulus window, too big for suture or tissue engineering reconstruction. Using an allogenic ligament (AusBiotech, Sydney, Australia) or a fabric (LARS, Arc-sur-Tille, France) in 18 cervical arthroplasty patients [51] X-ray studies confirmed the excessive mobility reduction without recovering the intact values, but they provided no biomechanical.
Looking for alternatives, we assessed the Kevlar®, for its known tensile strength properties [52] and biocompatibility [53, 54]. We tested it with a total disc prosthesis (ADDISC, Advanced Disc Design In Spinal Concepts) [55].
We studied movement angle, Instantaneous Axis of Rotation (IAR), and load distribution in human spine cadaveric specimens under four conditions:
-
The intact spinal column ("I").
-
L4–L5 discectomy with ALL and AFAP removal ("L").
-
After ADDISC total disc prosthesis implantation ("P").
-
With ADDISC prosthesis + Kevlar band implanted ("K").
We hypothesize that ALL and AFAP substitution by a Kevlar® band will recover the intact spinal movement ranges after lumbar disc arthroplasty.
Material and Methods
The study used twelve human cadaveric lumbar spine specimens provided by the Faculty of Medicine and Dentistry, University of Valencia, Spain. The corpses were kept cold from death until we removed the lumbar spines. The donors' age ranged from 18 to 50 years. Exclusion criteria: previous surgical procedures, trauma, malignancy, infection, demineralization, or inflammatory diseases affecting the lumbar or sacral spine.
We performed simple lumbosacral radiographic studies after death unless otherwise available. We ruled out lumbar and sacral spine osteoporosis using Dual Energy X-ray (DEXA) absorptiometry (Malvern Panalytical Ltd, Malvern, UK). After removing all soft tissues, except ligaments and intervertebral discs, each spine was sectioned at the L1–L2 disc and sacroiliac joints and frozen at -18ºC. Each specimen was assigned a number for identification.
The study used the ADDISC total disc prosthesis designed by our group [55].
Selection of the Material to Substitute the ALL and AFAP
The material had to be thin to allow its implantation between the spine and large retroperitoneal vessels, highly resistant to withstand the enormous tensile and rotational forces required, and easy to anchor to the vertebral bodies. We selected the Kevlar® type C 120 g/m2 (Stephanie Kwolek, DuPont, DuPont™ de Nemours, Inc., Buffalo, New York, USA), a synthetic para-aramid fiber (polyparaphenylene terephthalate), five times stronger than steel [52, 56]. Additionally, it is lightweight and can withstand extreme temperatures [52].
Biomechanical Studies
The study used an IBV (Institute of Biomechanics of Valencia) machine that simulates three main spinal movement axes: flexion–extension, lateral bending, and axial rotation. The kinematic study employed photogrammetry techniques.
We performed a displacement kinematic study of the movement range and IAR on each specimen (L2–S1) fixed with acrylic bone cement (SR Triplex Cold, Ivoclar Vivadent AG, FL-9494 Schaan, Liechtenstein, Switzerland) to the study machine jaws by polyethylene bowls on the L2 vertebral body and sacrum, ensuring that the L4–L5 disc remained in the horizontal plane (Fig. 1).
For the test, specimens remained attached by the top and bottom polyethylene bowls to the testing machine's upper and lower jaws (Fig. 2).
The study evaluated first the intact specimen (condition "I"), then after L4–L5 ALL, AFAP, and nucleus pulposus (NP) removal (condition "L), third post-ADDISC prosthesis implantation (condition "P"), and finally, with the Kevlar® band inserted (condition "K"), repeating at each step all biomechanical studies.
The testing machine generated flexion, extension, right and left lateral bending, and right and left axial rotation through a motor connected to a flexible cable, creating a torque onto the load cell connected to the upper jaw that held the specimen cranial end (Fig. 2). The spine caudal end was fixed and immobile in the machine's lower jaw.
The equipment comprised standard square 45 × 45 mm profiles (Bosch Rexroth AG, Würzburg, Germany, and a flexible cable 004000212-DB (BIAX Flexible Power, Schmid & Wezel GmbH, Sinsheim-Hilsbach, Germany) with 1960 Ncm maximum torque (Fig. 2).
A Nema 23-23HS22-2804S-HG50 motor (Stepperonline, OMC Corporation Ltd, Jiangning Nanjing, China) provided 25 Nm (absolute 40 Nm) maximum torque, 0.001125º maximum resolution, and 0.036º nominal precision. We calibrated the torque cell (20 Nm DYJN-130, CALTSensoR, Shanghai Qiyi Co., Ltd, Shanghai, China) to ± 10 Nm (cell range 2–200 Nm). We machined jaws and Cardan tightening parts at hoc and programmed the engine and load cell control software. Figure 2 shows the setup for the three-movement axes.
A DMM camera 22BUC03-ML (The Imaging Source, Bremen, Germany), resolution 744 × 480, capture frequency 30 fps (frames per second), and 5.5 mm optical recorded the spine movement and IAR capturing the movement of table-like markers (ChArUco, OpenCV, Intel, Santa Clara, CA, USA) with IC Capture software (The Imaging Source, Bremen, Germany) (Fig. 2).
For the test, we fixed each specimen on the testing machine. We glued five table-like markers (at upper and lower jaws and L3, L4, and L5 vertebral bodies) (Fig. 2) and applied flexion, extension, lateral bending, and axial rotation. Each movement cycle consisted of the load cell angular displacement reaching an 8 Nm fixed torque, first in one direction and then in the opposite one, recording throughout the range of movement. We established the neutral position for each specimen, condition, and motion axis, did conditioning with five cycles at 10º/s [57], and logged the data from 5 cycles at 10º/s.
The study variables were maximum and minimum angles of each movement axis, range (95th minus 5th percentile movement angles), and harmony (correlation between angle and angular acceleration, with values close to -1 indicating greater harmony and values close to zero showing less harmonic and more chaotic movement).
Technique to Anchor the Kevlar® Band to the Vertebral Bodies
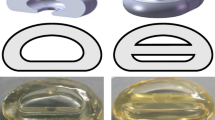
Once conducted the biomechanical studies in the intact spine, after L4–L5 discectomy with ALL and AFAP removal and post total disc prosthesis implantation, we secured a 3 × 3 cm Kevlar® band covering the surgical defect using 20 × 16 mm staples used to fasten tendons to bone (Acuña Fombona, Oviedo, Spain) (Fig. 3).
Two staples secured the Kevlar® band to each vertebral body (Fig. 4), and the biomechanical studies were repeated.
Statistical Study
We used the "R" (R Development Core Team) [58] and the Deducer user interface (I. Fellows, 'Deducer: A Data Analysis GUI for R', Journal of Statistical Software, Vol. 49, No 8,2012.) [59] and calculated movement angles and parameters using GNU Octave (GNU General Public License, https://www.gnu.org/software/octave/index)(65).
With an ANOVA test of related samples (paired), we compared the kinematic data (minimum, maximum, range, and harmony) between the different movement axes movement for each specimen in the four study statuses. We controlled the type I error (false positive) by comparing conditions by pairing through a post hoc analysis with a Bonferroni correction. We considered differences as statistically significant if p < 0.05.
Error bar charts show the data variability and estimate each condition's mean value with its statistical confidence level.
Results
The kinematic study analyzed the movement range first of the lumbosacral spine and second of its segments (L2–L3, L3–L4, L4–L5, and L5–S1).
Whole Lumbosacral Spine Kinematic Study
Flexion–Extension of the Whole Lumbosacral Spine
Table 1 shows the whole lumbosacral spine flexion and extension ANOVA statistical analysis. The extension increases maximally after ALL, AFAP, and NP removal (condition "L"), improves slightly after total disc prosthesis implantation (condition "P"), and ameliorates markedly after Kevlar® band insertion (condition "K") but without recovering the intact spine (condition "I") values. The flexion range with the Kevlar® band is smaller than the one for the intact spine; that is, it corrects the excess mobility created by conditions "L" and "P". Nevertheless, the movement range in flexion–extension of condition "K" is slightly above the "I" one because the decrease in flexion does not compensate for the increase in extension. The harmony deteriorates with the condition "L", improves in condition "P" but without recovering the intact spine values, and deteriorates markedly in condition "K", showing that the Kevlar® band improves the movement ranges of conditions "L" and "P", but with a less harmonic movement.
Table 2 shows the post hoc analysis with Bonferroni correction comparing the four conditions by pairing for the whole lumbosacral spine. There are statistically significant differences between almost all condition pairs and variables. Remarkedly, these differences are present when comparing conditions "I" and "K" in extension, range, and harmony but not for flexion. We expected these results because the Kevlar® band limits the extension but is less effective on flexion. At the same time, we see that comparing the "P" and "K" conditions, there are statistically significant differences only in extension, the movement the Kevlar® band restricts more.
Figure 5 shows the lumbosacral spine error bar charts with each study condition's mean values and confidence intervals for flexion, extension, range, and harmony. The movement range is more significant for condition "L", with values slightly lower than the intact spine for conditions "P" and "K". Perhaps by increasing the Kevlar® band tension, we could improve further the condition "K" extension range. The harmony is better for condition "I" and deteriorates gradually to condition "K", because the Kevlar® band only improves the movement ranges but not the harmony of movement.
In summary, there were statistically significant differences for the whole lumbosacral spine between the four study conditions for maximum extension, maximum flexion, range, and harmony. Condition "L" (after ALL, AFAP, and NP removal) undergoes a more significant movement range increase, which improves with total disc prosthesis implantation and Kevlar® band insertion, without recovering the intact spine status. The movement range is slightly higher in condition "K" than in the intact spine because the Kevlar® band replaces only partially the ALL and AFAP functions.
Regarding harmony, it worsens in conditions "L", "P", and "K" compared to the intact spine. This harmony impairment due to ALL, AFAP, and NP removal improves after lumbar disc arthroplasty but with values far from the intact spine. It worsens even further with Kevlar® band insertion, indicating that, although the range improves, the movement is less harmonic.
Lateral Bending of the Whole Lumbosacral Spine
Table 3 shows the whole lumbosacral spine lateral bending ANOVA statistical analysis. All kinematic variables showed statistically significant differences when comparing the study conditions. In left lateral bending, the movement range is smaller in the "L" than in conditions "I", "P", and "K", and Kevlar® band insertion restricts the motion range below the intact spine status. Meanwhile, in the right lateral bending, this range is lower in the intact spine, increasing in the other conditions, and the Kevlar® band allows a more comprehensive movement range than the other conditions, not recovering the intact spine values. These left–right differences could be due to asymmetric ALL, AFAP, and NP removal or Kevlar® band insertion, which we overlooked when conducting the study or reviewing the video recordings.
The movement range is slightly smaller for the "K" condition than the intact spine because the reduction in right lateral bending is more significant than the increase in the left.
The harmony improves after implanting the disc prosthesis (condition "P") compared to the intact spine (condition "I") and worsens with ALL, AFAP, and NP removal (condition "L") and especially with Kevlar® band insertion (condition "K"). Thus, this last situation improves the range but with less harmonic movement.
Table 4 shows the ANOVA post hoc analysis with Bonferroni correction of the whole lumbosacral spine in lateral bending, comparing the study conditions by pairing. Kevlar® band implantation presents statistically significant differences concerning the intact spine in the right lateral bending, range, and harmony but not in the left lateral bending. The "K" condition, compared with the "P" one, shows statistically significant differences in the right and left lateral bending and harmony but not in the movement range.
Figure 6 shows the whole lumbosacral spine error bar charts of the mean values with the confidence intervals for each study condition in the lateral bending movement. Kevlar® band insertion reduces the minimum movement range below the intact spine, but the maximum does not recover entirely, although it improves compared to ALL, AFAP, and NP removal and lumbar disc prosthesis implantation. The "K" condition movement range is more comprehensive than for "I", "L" and "P" ones. The harmony worsens even further after the Kevlar® band insertion, with a less harmonic movement than the intact spine or disc arthroplasty.
Axial Rotation of the Whole Lumbosacral Spine
Table 5 shows the whole lumbosacral spine in axial rotation ANOVA statistical analysis. The right and left axial rotation, range, and harmony present statistically significant differences. In the right axial rotation, the intact spine movement range (condition "I") increases with ALL, AFAP, and NP removal (condition "L"), raises even more with disc arthroplasty (condition "P"), and improves without recovering the intact spine status, with Kevlar® band insertion (condition "K"). Contrariwise, in the left axial rotation, the motion range is not significantly modified by ALL, AFAP, and NP removal (condition "L"), increases very markedly with total disc prosthesis implantation (condition "P"), and recovers with Kevlar® band insertion (condition "K"), with values even below those appreciated in the intact spine. As we discussed in the lateral bending movement, this could be due, at least in part, to an asymmetrical ALL, AFAP, and NP removal and Kevlar® band insertion. We also mentioned that this was not the team's impression when conducting the study or reviewing the videos.
The movement range is more significant after Kevlar® band insertion than for the intact spine. Still, it shows a considerable improvement compared to the situation after ALL, AFAP, and NP removal, and total disc prosthesis implantation.
The harmony also showed statistically significant differences, with lower values for conditions "L" and "K", but remarkably similar to the intact spine (condition "I") with total disc prosthesis implantation (condition "P"). Again, this fact shows that the Kevlar band limits the excessive movement ranges allowed after ALL, AFAP, and NP removal and total disc implantation but does not recover a harmonic movement.
Table 6 shows the ANOVA post hoc analysis with Bonferroni correction for the whole lumbosacral spine, comparing the study conditions by pairing. The "K" condition presents statistically significant differences concerning the intact spine in the maximum axial rotation movement, range, and harmony but not in the minimum. Thus, the Kevlar® band only effectively limits the maximum axial rotation. The condition "K" compared with total disc implantation shows statistically significant differences in the minimum axial rotation and harmony.
Figure 7 shows the error bar charts of the mean values with the confidence intervals for the whole lumbosacral spine for each study condition in axial rotation. The movement range is lower in condition "I" than in the others ("L", "P", and "K"). Disc arthroplasty (condition "P") has the smallest minimum range, and Kevlar® band insertion increases it compared to the intact spine. On the other hand, the maximum range is excessive in conditions "L", "P", and "K", indicating that Kevlar® band insertion fails to recover the intact spine movement range completely, unlike what happens in flexion–extension but similar to the situation in lateral bending.
In the movement range, Kevlar® band insertion improves compared to ALL, AFAP, and NP removal and disc arthroplasty, but it does not recover the intact spine status.
The harmony deteriorates after ALL, AFAP, and NP removal. It improves after disc arthroplasty but deteriorates further in condition "K". Thus, the Kevlar® band improves the whole lumbosacral spine movement range in axial rotation but with less harmonic movement.
Kinematic Study by Spinal Segments
Flexion–Extension of the Different Spinal Segments
Table 7 shows the descriptive and comparative values with a mixed linear model analyzing the study conditions' effect on each spinal segment flexion–extension movement range. The L2–L3, L3–L4, and L4–L5 discs show statistically significant differences, but not the L5–S1. As expected, the ranges undergo a few changes in the non-operated segments (L2–L3, L3–L4, and L5–S1), contrary to L4–L5. There, the flexion–extension increases markedly after ALL, AFAP, and NP removal (condition "L"), partially improves after disc arthroplasty (condition "P"), and further with Kevlar® band insertion (condition "K") without recovering the intact spine values. The non-operated discs L2–L3 and L3–L4 show a movement range increase with a concomitant reduction in the L5–S1. These results indicate that L4–L5 ALL, AFAP, and NP removal and total disc prosthesis implantation affect the movement range of the two discs above but not the one below.
Table 8 depicts the ANOVA post hoc statistical analysis with Bonferroni correction by spinal segments, comparing the study conditions by pairing. Kevlar® band insertion (condition "K") shows statistically significant differences concerning the intact spine (condition "I") for the L2–L3 and L4–L5 spinal segments but not for the L3–L4 and L5–S1 ones.
Figure 8 shows the error bar charts of the mean values with the confidence intervals for each spinal segment and condition in the flexion–extension movement. The movement ranges undergo moderate changes in the non-operated discs (L2–L3, L3–L4, and L5–S1) but are significant in the L4–L5 one. In this disc, the flexion–extension range increases very markedly after ALL, AFAP, and NP removal (condition "L"), partially improves with disc arthroplasty (condition "P"), and especially with Kevlar® band insertion (condition "K"), but the intact disc values are not recovered.
Lateral Bending of the Different Spinal Segments
Table 9 shows the descriptive and comparative values with a mixed linear model analyzing the study conditions' effect on each spinal segment on the lateral bending movement range. The values show statistically significant differences in the L3–L4 and L4–L5 discs, which increase with ALL, AFAP, and NP removal (condition ("L") and further with disc arthroplasty (condition "P") but improve after Kevlar® band insertion (condition "K"), without recovering the intact disc values. The L2–L3 range increases but reduces for L3–L4 and L5–S1. Contrariwise to flexion–extension, in lateral bending, the L3–L4 disc, the one above the operated one (L4–L5), reduces its movement range after adjacent level disc arthroplasty.
Table 10 shows the results of the comparative post hoc analysis with Bonferroni correction of the different spinal segments comparing the four conditions by pairing in the lateral bending movement. Kevlar® band insertion (condition "K"), compared to the intact spine, shows no statistically significant differences for any spinal segment. These differences are present only in the L3–L4 disc (not operated) and in the L4–L5 (operated) when comparing the intact spine with the condition after disc arthroplasty and in the L3–L4 disc comparing the "P" and "K" conditions. This situation indicates that disc arthroplasty and Kevlar® band insertion induce movement range changes in the adjacent level (L3–L4).
Figure 9 shows the error bar charts for each spinal segment of the mean values with the confidence intervals for each study condition in the lateral bending movement. The L4–L5 disc shows a marked increase with ALL, AFAP, and NP removal (condition "L"), which increases even further with disc arthroplasty (condition "P") and improves with Kevlar band® insertion (condition "K"), but the intact spine range is not recovered.
Axial Rotation of the Different Spinal Segments
Table 11 shows the descriptive and comparative values obtained using a mixed linear model that analyzes the effect of the study conditions on the axial rotation movement range for the different spinal segments. The values show statistically significant differences in the L3–L4 and L4–L5 discs. In the latter, there is an increase in condition "L", especially after disc arthroplasty, which improves with Kevlar® band insertion without returning to the intact spine status. This motion range increases for the L3–L4 disc but remains almost unchanged for L2–L3 and L5–S1. This fact shows that L4–L5 disc arthroplasty changes the axial rotation motion range of the non-operated above disc.
Table 12 shows the results of the post hoc comparative analysis with the Bonferroni correction of each spinal segment by pairing the study conditions on axial rotation. There are statistically significant differences between the intact spine and Kevlar® band insertion for the L3–L4 (non-operated) and L4–L5 (operated) discs but not for the L2–L3 and L5–S1 ones.
Figure 10 shows the error bar charts for each spinal segment of the mean values with the confidence intervals comparing by pairing the four conditions in axial rotation. In the L4–L5 disc, the movement range markedly increases with condition "L" (ALL, AFNP, and NP removal), partially improves with condition "P" (disc arthroplasty), and with further improvement with condition "K" (Kevlar® band insertion), but without returning to the condition "I" (intact spine) values.
Instantaneous Axis of Rotation (IAR)
The IAR is an imaginary point in a rigid body or mechanical system where, at any given time, all the body or system particles are spinning without slipping. In other words, it is the point at which all the rigid body of system particles have an equal magnitude of rotational velocity but opposite direction, so there is no relative movement between them.
The graphs show how the IAR position varies depending on the study conditions, forces, or movements.
Instantaneous Axis of Rotation in the Flexion–Extension Movement
Figure 11 (anteroposterior or y-axis) and Fig. 12 (vertical or z-axis) show the IAR displacement in flexion–extension. It moves forward with flexion and backward with extension and descends vertically with the maximum flexion and extension. At the same time, it remains at a higher point with minimum flexion and extension. The Kevlar® band partially recovers the IAR compared to disc arthroplasty without recovering the intact spine values, particularly in the vertical axis (z-axis).
Instantaneous Axis of Rotation in the Lateral Bending Movement
Figure 13 (right-left or x-axis) and Fig. 14 (vertical or z-axis) show the IAR displacement in lateral bending. The Kevlar® band improves the situation after disc arthroplasty but does not reproduce the intact spine values.
Instantaneous Axis of Rotation in the Axial Rotation Movement
Figure 15 (right-left or x-axis) and Fig. 16 (anteroposterior or y-axis) show the IAR displacement in the axial rotation movement. The Kevlar® band insertion improves the situation on the x-axis compared to disc arthroplasty but does not reproduce the intact spine values, particularly on the y-axis.
Force–Displacement Curves
The mean force–displacement curves represent each specimen's average force or torque variation value concerning the angle displaced for each study condition.
In flexion–extension, the Kevlar® band limits the extension without recovering the intact spine status. The limitation in flexion is less significant but with values more closely resembling those of condition "I" (Fig. 17). The Kevlar® band improves the operated level biomechanics compared to disc arthroplasty, making them more similar to those of the intact spine.
Kevlar® band insertion, compared to the intact spine, restricts the movement range more in the right than in the left lateral bending (Fig. 18). The curve does not entirely mimic the condition "I" values. Still, there is a significant improvement compared to ALL, AFAP, and ANP removal (condition "L") and disc arthroplasty (condition "P"). Kevlar® band improves the biomechanical behavior in extension, making it more similar to the intact spine.
ALL, AFAP, and NP removal (condition "L") significantly increase the movement range, particularly in right axial rotation. Kevlar® band insertion improves these ranges but is higher than the intact spine and disc arthroplasty, particularly in the left axial rotation (Fig. 19).
Discussion
There are many reports on techniques and materials for repairing the annulus fibrosus [44,45,46,47,48, 60,61,62,63,64,65,66]. However, the studies focus on experimental lesions 1–6 mm in diameter [38, 39, 67,68,69] or the annulotomy on a lumbar discectomy [51, 70]. Contrariwise, implanting a total disc prosthesis requires removing an ALL and AFNP section 2.5–3 cm × 8 mm in size 431.432. Sutures or polymeric materials with or without stem cells cannot repair such broad defects [71, 72].
Ligament injury increases vertebral segment instability [73, 74]. On the cervical spine, many recommend posterior longitudinal ligament removal (PLL) [75,76,77] to improve spinal cord decompression [12, 40, 78]. However, this surgical maneuver increases the mobility to non-physiological ranges, particularly in extension and axial rotation [75,76,77]. Inserting a total disc prosthesis 2 mm taller than the original disc corrects this hypermobility [41] as it tightens the remaining ligaments [31]. However, it is unclear if this can foster their degeneration and, thus, future problems.
Finite element analyses and ex vivo animal cadaveric spine studies show that ALL and AFAP removal create excessive spinal mobility in extension and axial rotation [70, 79,80,81]. This hypermobility occurs with all lumbar disc prostheses, irrespective of their design, and is only partially corrected when a substitute, such as a ligamentous band, is implanted, covering the anterior aspect of the removed disc in disc arthroplasty [73, 82]. Only one clinical study on 18 cervical spine patients describes this technique [51], but more data are needed to confirm its usefulness and find the best material. It is an option to remember in disc arthroplasty, particularly at the lumbar level.
Perhaps postoperative scarring will reduce mobility to physiological ranges, but it is an area that needs further research.
Finally, the ideal material for ALL and AFAP repair requires further research. Our study shows that Kevlar® type C band insertion has a role in this field because it can reduce the excessive spinal movement range, particularly in extension, and less effectively in lateral bending and axial rotation, but at the price of a less harmonic movement. Likewise, the IAR improves with Kevlar® band insertion without recovering the intact spine values. To evaluate these data, we must consider that our study does not entail a centrally applied axial load, which would have provided a better total disc prosthesis grip on the nearby vertebral endplates.
We did not study the effect of the Kevlar® band tension on insertion and to what extent tightening it further might or might not improve the results. We plan to investigate it in future studies.
An unexpected finding was that ALL, AFAP and NP removal, disc arthroplasty, and Kevlar® band insertion) changed the L3–L4 (non-operated disc) movement ranges above the operated one. Contrarywise, these ranges are not changed significantly for the caudal adjacent level (L5–S1). These data confirm previous biomechanical cadaveric studies [42].
Further research is needed to see what type of Kevlar®, band size, and fixation method achieves the best results. We do not know, once implanted inside the human body at the prevertebral level, which scar reaction will cause and to what extent this scar will modify the movement ranges, making them even closer to the intact spine, especially in lateral bending and axial rotation, are the least improved after Kevlar® band insertion.
Limitations
This study has many limitations, such as an in vitro experiment, a small sample size, cadaver specimens without muscle, and an acute analysis without considering implant wear and tear. We have tested only a type of Kevlar®, so it would be interesting to assess diverse types of this material to see which one best suits and do biocompatibility studies. We should control the tension at which the Kevlar® band is inserted. In future studies, we should ensure that the ALL and AFAP removal is symmetrical.
Strengths
Each specimen has been its control. We have done extensive biomechanical studies.
Conclusions
The L4–L5 disc, after discectomy and disc arthroplasty, showed an increase in the extension, reduced by Kevlar® band insertion but without recovering the intact spine values.
In lateral bending, conditions "L", "P", and "K" showed a more substantial mobility range compared to "I" one. The Kevlar® band insertion, compared to the intact spine, showed no statistically significant differences for any spinal segment. When comparing the intact spine with disc arthroplasty, these differences are present in the L3–L4 (not operated) and the L4–L5 (operated) discs.
In axial rotation, there were statistically significant differences between the intact spine (condition "I") and condition "K" (Kevlar® band inserted) for the L3–L4 (non-operated) and L4–L5 (operated) discs but not for the L2–L3 and L5–S1 ones.
The Kevlar® band recovers only partially the intact spine IAR in flexion–extension, particularly in the vertical axis (z-axis). In lateral bending, it improves the IAR after disc arthroplasty but does not reproduce the intact spine values. In axial rotation, it improves the IAR in the x-axis compared to the total disc replacement but does not recover baseline status, particularly in the y-axis.
In conclusion, our study confirms that repairing the ALL and the AFAP in disc arthroplasty improves the spinal movement range without completely recovering the intact spine status. The range improves significantly, particularly in extension and maximum rotation, but at the price of a less harmonic movement.
Data Availability
Data are the property of a private company, and authors need permission to make them available to third parties.
References
F. Fatoye, T. Gebrye, I. Odeyemi, Real-world incidence and prevalence of low back pain using routinely collected data. Rheumatol. Int. 39(4), 619–626 (2019)
R.D. Meucci, A.G. Fassa, N.M.X. Faria, Prevalence of chronic low back pain: systematic review. Rev. Saude Publica 49 (2015)
L. Manchikanti, V. Singh, F.J.E. Falco, R.M. Benyamin, J.A. Hirsch, Epidemiology of low back pain in adults. Neuromodul. Octubre de 17(Suppl 2), 3–10 (2014)
L. Manchikanti, V. Pampati, A.D. Kaye, J.A. Hirsch, Therapeutic lumbar facet joint nerve blocks in the treatment of chronic low back pain: cost utility analysis based on a randomized controlled trial. Korean J. Pain. 31(1), 27–38 (2018)
J. Zeckser, M. Wolff, J. Tucker, J. Goodwin, Multipotent mesenchymal stem cell treatment for discogenic low back pain and disc degeneration. Stem Cells Int. 2016, 3908389 (2016)
A. Mahmoudzadeh, Z.S. Rezaeian, A. Karimi, J. Dommerholt, The effect of dry needling on the radiating pain in subjects with discogenic low-back pain: a randomized control trial. J. Res. Med. Sci. 21, 86 (2016)
K. Hashimoto, T. Aizawa, H. Kanno, E. Itoi, Adjacent segment degeneration after fusion spinal surgery—a systematic review. Int. Orthop. 43(4), 987–993 (2019)
C.F. Müller, T. Monrad, F. Biering-Sørensen, E. Darre, A. Deis, P. Kryger, The influence of previous low back trouble, general health, and working conditions on future sick-listing because of low back trouble. A 15-year follow-up study of risk indicators for self-reported sick-listing caused by low back trouble. Spine 24(15), 1562–1570 (1999)
S. Bartys, P. Frederiksen, T. Bendix, K. Burton, System influences on work disability due to low back pain: an international evidence synthesis. Health Policy 121(8), 903–912 (2017)
J.W. Geurts, P.C. Willems, J.W. Kallewaard, M. van Kleef, C. Dirksen, The impact of chronic discogenic low back pain: costs and patients’ burden. Pain Res. Manag. 2018, 4696180 (2018)
F. Ding, Z. Jia, Z. Zhao, L. Xie, X. Gao, D. Ma et al., Total disc replacement versus fusion for lumbar degenerative disc disease: a systematic review of overlapping meta-analyses. Eur. Spine J. 26(3), 806–815 (2017)
D.Y. Bai, L. Liang, B.B. Zhang, T. Zhu, H.J. Zhang, Z.G. Yuan et al., Total disc replacement versus fusion for lumbar degenerative diseases—a meta-analysis of randomized controlled trials. Medicine (Baltimore) 98(29), e16460 (2019)
J. Zigler, M.F. Gornet, N. Ferko, C. Cameron, F.W. Schranck, L. Patel, Comparison of lumbar total disc replacement with surgical spinal fusion for the treatment of single-level degenerative disc disease: a meta-analysis of 5-year outcomes from randomized controlled trials. Global Spine J. 8(4), 413–423 (2018)
K. Radcliff, J. Spivak, B. Darden, M. Janssen, T. Bernard, J. Zigler, Five-year reoperation rates of 2-level lumbar total disk replacement versus fusion: results of a prospective, Randomized Clinical Trial. Clin. Spine Surg. 31(1), 37–42 (2018)
R.C. Huang, F.P. Girardi, F.P. Cammisa, T.M. Wright, The implications of constraint in lumbar total disc replacement. J. Spinal Disord. Tech. 16(4), 412–417 (2003)
J. Choi, D.A. Shin, S. Kim, Biomechanical effects of the geometry of ball-and-socket artificial disc on lumbar spine: a finite element study. Spine 42(6), E332–E339 (2017)
H. Schmidt, F. Galbusera, A. Rohlmann, T. Zander, H.J. Wilke, Effect of multilevel lumbar disc arthroplasty on spine kinematics and facet joint loads in flexion and extension: a finite element analysis. Eur. Spine J. 21(Suppl 5), S663-674 (2012)
D. Abi-Hanna, J. Kerferd, K. Phan, P. Rao, R. Mobbs, Lumbar disk arthroplasty for degenerative disk disease: literature review. World Neurosurg. 109, 188–196 (2018)
A. Drysch, R.M. Ajiboye, A. Sharma, J. Li, T. Reza, D. Harley et al., Effectiveness of reoperations for adjacent segment disease following lumbar spinal fusion. Orthopedics 41(2), e161–e167 (2018)
R.D. Guyer, P.C. McAfee, R.J. Banco, F.D. Bitan, A. Cappuccino, F.H. Geisler et al., Prospective, randomized, multicenter Food and Drug Administration investigational device exemption study of lumbar total disc replacement with the CHARITE artificial disc versus lumbar fusion: five-year follow-up. Spine J. 9(5), 374–386 (2009)
M. Panjabi, G. Malcolmson, E. Teng, Y. Tominaga, G. Henderson, H. Serhan, Hybrid testing of lumbar CHARITE discs versus fusions. Spine 32(9), 959–966 (2007). (discussion 967)
M.F. Gornet, J.K. Burkus, R.F. Dryer, J.H. Peloza, F.W. Schranck, A.G. Copay, Lumbar disc arthroplasty versus anterior lumbar interbody fusion: 5-year outcomes for patients in the Maverick disc investigational device exemption study. J. Neurosurg. Spine 31, 1–10 (2019)
R.D. Guyer, K. Pettine, J.S. Roh, T.A. Dimmig, D. Coric, P.C. McAfee et al., Five-year follow-up of a prospective, randomized trial comparing two lumbar total disc replacements. Spine 41(1), 3–8 (2016)
P. Clavel, G. Ungureanu, I. Catalá, G. Montes, X. Málaga, M. Ríos, Health-related quality of life in patients undergoing lumbar total disc replacement: a comparison with the general population. Clin. Neurol. Neurosurg. 160, 119–124 (2017)
X.D. Cui, H.T. Li, W. Zhang, L.L. Zhang, Z.P. Luo, H.L. Yang, Mid- to long-term results of total disc replacement for lumbar degenerative disc disease: a systematic review. J. Orthop. Surg. Res. 13(1), 326 (2018)
M.H. Shin, K.S. Ryu, N.K. Rathi, C.K. Park, Segmental translation after lumbar total disc replacement using Prodisc-L®: associated factors and relation to facet arthrosis. J. Neurosurg. Sci. 61(1), 14–21 (2017)
X. Hu, K. Li, Stress changes of upper lumbar facet joint after discectomy and artificial disc replacement. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 19(6), 427–430 (2005)
C. Hellum, L. Berg, Ø. Gjertsen, L.G. Johnsen, G. Neckelmann, K. Storheim et al., Adjacent level degeneration and facet arthropathy after disc prosthesis surgery or rehabilitation in patients with chronic low back pain and degenerative disc: second report of a randomized study. Spine 37(25), 2063–2073 (2012)
J.I. Choi, S.H. Kim, D.J. Lim, S.K. Ha, S.D. Kim, Biomechanical changes in disc pressure and facet strain after lumbar spinal arthroplasty with CharitéTM in the human cadaveric spine under physiologic compressive follower preload. Turk. Neurosurg. 27(2), 252–258 (2017)
E. Sariali, J.P. Lemaire, H. Pascal-Mousselard, H. Carrier, W. Skalli, In vivo study of the kinematics in axial rotation of the lumbar spine after total intervertebral disc replacement: long-term results: a 10–14 years follow up evaluation. Eur. Spine J. 15(10), 1501–1510 (2006)
A. Rohlmann, T. Zander, G. Bergmann, Effect of total disc replacement with ProDisc on intersegmental rotation of the lumbar spine. Spine 30(7), 738–743 (2005)
T. Zander, A. Rohlmann, G. Bergmann, Influence of different artificial disc kinematics on spine biomechanics. Clin. Biomech. (Bristol, Avon) 24(2), 135–142 (2009)
T. David, Lumbar disc prosthesis. Surgical technique, indications and clinical results in 22 patients with a minimum of 12 months follow-up. Eur. Spine J. 1(4), 254–259 (1993)
P. Tropiano, R.C. Huang, F.P. Girardi, F.P. Cammisa, T. Marnay, Lumbar total disc replacement. Surgical technique. J. Bone Jt. Surg. Am. 88, 50–64 (2006)
F.H. Geisler, Surgical technique of lumbar artificial disc replacement with the Charité artificial disc. Neurosurgery 56(1 Suppl), 46–57 (2005)
M. Sharabi, A. Levi-Sasson, R. Wolfson, K.R. Wade, F. Galbusera, D. Benayahu et al., The mechanical role of the radial fibers network within the annulus fibrosus of the lumbar intervertebral disc: a finite elements study. J. Biomech. Eng. 141, 021006 (2018)
B. Cakir, R. Schmidt, T. Mattes, C.R. Fraitzl, H. Reichel, W. Käfer, Index level mobility after total lumbar disc replacement: is it beneficial or detrimental? Spine 34(9), 917–923 (2009)
J.J. Yang, F. Li, K.C. Hung, S.H. Hsu, J.L. Wang, Intervertebral disc needle puncture injury can be repaired using a gelatin-poly (γ-glutamic acid) hydrogel: an in vitro bovine biomechanical validation. Eur. Spine J. 27(10), 2631–2638 (2018)
K. Rickers, M. Bendtsen, D.Q.S. Le, A.J. der Veen, C.E. Bünger, Biomechanical evaluation of annulus fibrosus repair with scaffold and soft anchors in an ex vivo porcine model. SICOT J. 4, 38 (2018)
J.S. Ham, J.H. Kim, J.H. Yoon, S.H. Hwang, S.H. Yoon, Progression of ossification of the posterior longitudinal ligament after cervical total disc replacement. Korean J. Neurotrauma. 15(2), 135–142 (2019)
A. Faizan, V.K. Goel, S.R. Garfin, C.M. Bono, H. Serhan, A. Biyani et al., Do design variations in the artificial disc influence cervical spine biomechanics? A finite element investigation. Eur. Spine J. 21(Suppl 5), 653–662 (2012)
S.K. Ha, S.H. Kim, D.H. Kim, J.Y. Park, D.J. Lim, S.K. Lee, Biomechanical study of lumbar spinal arthroplasty with a semi-constrained artificial disc (activ L) in the human cadaveric spine. J. Korean Neurosurg. Soc. 45(3), 169–175 (2009)
K. Kafchitsas, M. Kokkinakis, B. Habermann, M. Rauschmann, Effect of lumbar disc replacement on the height of the disc space and the geometry of the facet joints: a cadaver study. J. Bone Jt. Surg. Br. 92(4), 595–601 (2010)
E. Roebke, D. Jacho, O. Eby, S. Aldoohan, H. Elsamaloty, E. Yildirim-Ayan, Injectable cell-laden nanofibrous matrix for treating annulus fibrosus defects in porcine model: an organ culture study. Life (Basel) 12(11), 1866 (2022)
A.G. Scheibler, T. Götschi, J. Widmer, C. Holenstein, T. Steffen, R.S. Camenzind et al., Feasibility of the annulus fibrosus repair with in situ gelating hydrogels—a biomechanical study. PLoS ONE 13(12), e0208460 (2018)
T.J. DiStefano, K. Vaso, C.J. Panebianco, G. Danias, H.N. Chionuma, K. Kunnath et al., Hydrogel-embedded poly(lactic-co-glycolic acid) microspheres for the delivery of hMSC-derived exosomes to promote bioactive annulus fibrosus repair. Cartilage 13(3), 19476035221113960 (2022)
R. Deng, R. Kang, X. Jin, Z. Wang, X. Liu, Q. Wang et al., Mechanical stimulation promotes MSCs healing the lesion of intervertebral disc annulus fibrosus. Front. Bioeng. Biotechnol. 11, 1137199 (2023)
M.R. Saghari Fard, J.P. Krueger, S. Stich, P. Berger, A.A. Kühl, M. Sittinger et al., A biodegradable polymeric matrix for the repair of annulus fibrosus defects in intervertebral discs. Tissue Eng. Regen. Med. 19(6), 1311–1320 (2022)
S. Helm Ii, T.T. Simopoulos, M. Stojanovic, S. Abdi, M.A. El Terany, Effectiveness of thermal annular procedures in treating discogenic low back pain. Pain Physician 20(6), 447–470 (2017)
J.J. Yue, C. Telles, T.P. Schlösser, S. Hermenau, R. Ramachandran, W.D. Long, Do presence and location of annular tear influence clinical outcome after lumbar total disc arthroplasty? A prospective 1-year follow-up study. Int. J. Spine Surg. 6, 13–17 (2012)
R.J. Mobbs, J.X.J. Li, K. Phan, Anterior longitudinal ligament reconstruction to reduce hypermobility of cervical and lumbar disc arthroplasty. Asian Spine J. 11(6), 943–950 (2017)
Q. He, S. Cao, Y. Wang, S. Xuan, P. Wang, X. Gong, Impact resistance of shear thickening fluid/Kevlar composite treated with shear-stiffening gel. Composites A 106, 82–90 (2018)
J.D. Henderson, R.H. Mullarky, D.E. Ryan, Tissue biocompatibility of kevlar aramid fibers and polymethylmethacrylate, composites in rabbits. J. Biomed. Mater. Res. 21(1), 59–64 (1987)
S. De La Garza-Castro, C.E. González-Rivera, F. Vílchez-Cavazos, R. Morales-Avalos, F.J. Barrera-Flores, R.E. Elizondo-Omaña et al., Clinical, biomechanical and morphological assessment of anterior cruciate ligament Kevlar®-based artificial prosthesis in rabbit model. J. Appl. Biomater. Funct. Mater. 15(3), 251–261 (2017)
A. Vanaclocha, V. Vanaclocha, C.M. Atienza, P. Jorda-Gomez, C. Diaz-Jimenez, J.A. Garcia-Lorente et al., ADDISC lumbar disc prosthesis: analytical and FEA testing of novel implants. Heliyon 9(2), e13540 (2023)
A. Srivastava, A. Majumdar, B.S. Butola, Improving the impact resistance performance of Kevlar fabrics using silica based shear thickening fluid. Mater. Sci. Eng. A 529, 224–229 (2011)
J.M. Popovich, J.B. Welcher, T.P. Hedman, W. Tawackoli, N. Anand, T.C. Chen et al., Lumbar facet joint and intervertebral disc loading during simulated pelvic obliquity. Spine J. 13(11), 1581–1589 (2013)
R: The R Project for Statistical Computing [Internet]. 2020. https://www.r-project.org/. Accessed 6 June 2020
I. Fellows, Deducer: a data analysis GUI for R. J. Stat. Softw. 49, 1–15 (2012)
T. Aihara, K. Endo, H. Suzuki, Y. Sawaji, M. Urushibara, Y. Matsuoka et al., Long-term outcomes following lumbar microendoscopic diskectomy and microendoscopic decompression: minimum 10-year follow-up evaluation performed using a patient-based outcome measure. J. Neurol. Surg. A 81(2), 163–169 (2020)
Q. Wei, D. Liu, G. Chu, Q. Yu, Z. Liu, J. Li et al., TGF-β1-supplemented decellularized annulus fibrosus matrix hydrogels promote annulus fibrosus repair. Bioact. Mater. 19, 581–593 (2022)
A.S. Croft, S. Ćorluka, J. Fuhrer, M. Wöltje, J. Silva-Correia, J.M. Oliveira et al., Repairing annulus fibrosus fissures using methacrylated gellan gum combined with novel silk. Materials (Basel) 16(8), 3173 (2023)
S. Wang, Y. He, J. Ma, L. Yu, J. Wen, X. Ye, Dynamic bioreactor culture for infiltration of bone mesenchymal stem cells within electrospun nanofibrous scaffolds for annulus fibrosus repair. Orthop. Surg. 12(1), 304–311 (2020)
C. Liu, Z. Jin, X. Ge, Y. Zhang, H. Xu, Decellularized annulus fibrosus matrix/chitosan hybrid hydrogels with basic fibroblast growth factor for annulus fibrosus tissue engineering. Tissue Eng. Part A 25(23–24), 1605–1613 (2019)
J. Ma, Y. He, X. Liu, W. Chen, A. Wang, C.Y. Lin et al., A novel electrospun-aligned nanoyarn/three-dimensional porous nanofibrous hybrid scaffold for annulus fibrosus tissue engineering. Int. J. Nanomed. 15(13), 1553–1567 (2018)
R.G. Long, S.G. Rotman, W.W. Hom, D.J. Assael, S. Illien-Jünger, D.W. Grijpma et al., In vitro and biomechanical screening of polyethylene glycol and poly(trimethylene carbonate) block copolymers for annulus fibrosus repair. J. Tissue Eng. Regen. Med. 12(2), e727–e736 (2018)
M.I. Page, J.T. Easley, A.F. Bonilla, V.V. Patel, C.M. Puttlitz, Biomechanical evaluation of a novel repair strategy for intervertebral disc herniation in an ovine lumbar spine model. Front. Bioeng. Biotechnol. 10, 1018257 (2022)
R.G. Long, S.J. Ferguson, L.M. Benneker, D. Sakai, Z. Li, A. Pandit et al., Morphological and biomechanical effects of annulus fibrosus injury and repair in an ovine cervical model. JOR Spine 3(1), e1074 (2019)
T. Nukaga, D. Sakai, J. Schol, M. Sato, M. Watanabe, Annulus fibrosus cell sheets limit disc degeneration in a rat annulus fibrosus injury model. JOR Spine 2(2), e1050 (2019)
L. Marchi, L. Oliveira, E. Coutinho, L. Pimenta, The importance of the anterior longitudinal ligament in lumbar disc arthroplasty: 36-month follow-up experience in extreme lateral total disc replacement. Int. J. Spine Surg. 6, 18–23 (2012)
M.A. Cruz, W.W. Hom, T.J. DiStefano, R. Merrill, O.M. Torre, H.A. Lin et al., Cell-seeded adhesive biomaterial for repair of annulus fibrosus defects in intervertebral discs. Tissue Eng. Part A 24(3–4), 187–198 (2018)
M. Cabraja, M. Endres, A.A. Hegewald, S. Vetterlein, C. Thomé, C. Woiciechowsky et al., A 3D environment for anulus fibrosus regeneration. J. Neurosurg. Spine 17(2), 177–183 (2012)
V.K. Goel, A. Faizan, V. Palepu, S. Bhattacharya, Parameters that effect spine biomechanics following cervical disc replacement. Eur. Spine J. 21(Suppl 5), S688-699 (2012)
R. Schmidt, U. Obertacke, J. Nothwang, C. Ulrich, J. Nowicki, H. Reichel et al., The impact of implantation technique on frontal and sagittal alignment in total lumbar disc replacement: a comparison of anterior versus oblique implantation. Eur. Spine J. 19(9), 1534–1539 (2010)
L.I. Voronov, R.M. Havey, P.P. Tsitsopoulos, S. Khayatzadeh, J. Goodsitt, G. Carandang et al., Does resection of the posterior longitudinal ligament affect the stability of cervical disc arthroplasty? Int J Spine Surg. 12(2), 285–294 (2018)
C.C. Yu, D.J. Hao, Y.L. Ma, D.G. Huang, H.K. Li, H. Feng et al., The role of posterior longitudinal ligament in cervical disc replacement: an ovine cadaveric biomechanical analysis. Med. Sci. Monit. 22, 1843–1849 (2016)
B. Cakir, M. Richter, W. Schmoelz, R. Schmidt, H. Reichel, H.J. Wilke, Resect or not to resect: the role of posterior longitudinal ligament in lumbar total disc replacement. Eur. Spine J. 21(Suppl 5), S592-598 (2012)
J. Zhu, Q. Lu, X. Zhan, S. Huang, C. Zhou, S. Wu et al., To infer the probability of cervical ossification of the posterior longitudinal ligament and explore its impact on cervical surgery. Sci. Rep. 13, 9816 (2023)
H.J. Wilke, R. Schmidt, M. Richter, W. Schmoelz, H. Reichel, B. Cakir, The role of prosthesis design on segmental biomechanics: semi-constrained versus unconstrained prostheses and anterior versus posterior centre of rotation. Eur. Spine J. 21(Suppl 5), S577-584 (2012)
A. Rohlmann, A. Mann, T. Zander, G. Bergmann, Effect of an artificial disc on lumbar spine biomechanics: a probabilistic finite element study. Eur. Spine J. 18(1), 89–97 (2009)
M. Mumtaz, J. Mendoza, S. Tripathi, A. Kelkar, N. Nishida, A. Sahai et al., Total disc replacement alters the biomechanics of cervical spine based on sagittal cervical alignment: a finite element study. J. Craniovertebr. Junct. Spine 13(3), 278–287 (2022)
G.R. Buttermann, B.P. Beaubien, Biomechanical characterization of an annulus sparing spinal disc prosthesis. Spine J. 9(9), 744–753 (2009)
Acknowledgements
We thank Amelia Gomez for her assistance and help.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interests (such as honoraria, educational grants, participation in speaker's bureaus, membership, employment, consultancies, stock ownership, or other equity interest, and expert testimony or patent-licensing arrangements), or non-financial interests (such as personal or professional relationships, affiliations, knowledge or belief(s) in the subject matter or materials discussed in this manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vanaclocha, A., Vanaclocha, V., Atienza, C.M. et al. Prevertebral Anchored Kevlar Band to Recover Intact Spine Movement Ranges in Lumbar Disc Arthroplasty. Biomedical Materials & Devices 2, 1102–1124 (2024). https://doi.org/10.1007/s44174-023-00143-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44174-023-00143-3