Abstract
Purpose
The purpose of this study was to explore the role of self-directed ageism in the relationship between frailty and quality of life in community-dwelling older adults.
Methods
Secondary data-analysis on data from the Belgian Ageing Studies. A stratified sample of 1895 participants, based on census data by gender and age, was drawn between 2017 and 2019. Frailty, quality of life and self-directed ageism were assessed by the Comprehensive Frailty Assessment Instrument, a numeric rating scale and a newly developed self-directed ageism scale, respectively. The validity of this new scale was assessed by exploratory factor analysis, while mediation analysis was used to explore if self-directed ageism mediates the relationship between frailty and quality of life.
Results
The self-directed ageism scale proved highly reliable (Cronbach’s α = 0.898, Spearman-Brown = 0.906), explaining 58.86% of the variance in self-directed ageism. Respondents scored an average of 23.6 on 40 for self-directed ageism, 26.94 on 100 for frailty, and a median of 8 on 10 for quality of life. Mediation analysis showed that frailty negatively correlates with quality of life, and that this relationship is partially mediated by self-directed ageism.
Conclusion
Most respondents were identified as mild frail, experienced self-directed ageism, and those 80 or older rated their quality of life lower. The present study showed that frailty negatively correlates with quality of life and this relationship is partially mediated by self-directed ageism. We conclude that every effort should be made to prevent frailty, ageism and self-directed ageism as they impact community-dwelling older people’s quality of life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Better living conditions along with technical and medical progress have contributed to an increased longevity. Also, on a worldwide scale, the population aged 60 and older is increasing faster than younger age groups and as a consequence the world population is aging [1]. Globally, the proportion of people aged 65 and over is approximately 10% in 2022 and is projected to reach about 16% in 2050 [2].This aging trend is also reflected in Belgium, where a quarter of the population was 60 and older in 2021 [3]. In the future, the proportion of older people will increase even further [4]. Actually, the majority of the older population lives at home and prefers to stay there for as long as possible [5].
Despite the increased longevity, Officer and colleagues [6] argue that there is little evidence that today’s older people enjoy better health than previous generations. They state that the little respect they receive, along with negative attitudes toward and omnipresent stereotypes about older people, or ageism, underlie this. Butler described and reported ‘age-ism’ or age discrimination as early as 1969 as “the prejudice by one age group toward other age groups”, and called it another form of bigotry [7]. The World Health Organization (WHO) considers ageism as a multidimensional social phenomenon and defines it as age-based stereotypes, prejudice, and discrimination, which may be explicit or implicit and manifest at various levels, such as institutional, interpersonal, or internalized (or self-directed). Ageism is widespread and occurs in various institutions and sectors of society; at work, in health care, in the media, and in the legal system, and on average, one in two people worldwide is ageist [8]. Although ageism can target both the young and the old [9], only ageism targeting the old will be discussed here.
A possible explanation for the phenomenon of ageism is given by Greenberg and colleagues [10]. According to their terror management theory, people are terrified of their own ultimate vulnerability and death and use various defense mechanisms to control this fear. Martens and colleagues [11] extended this perspective by arguing that this fear of transience and death also underlies ageism toward older people, in that older people remind young people of their own inevitably aging and mortality. Older people remind young people of their own fear of loss of dignity and self-worth, decay, and death, and in order to control this fear of death, non-older people develop negative reactions towards older people that are expressed in age-related thoughts (stereotypes), feelings (prejudice) and actions (discrimination). Unlike other forms of stereotypes, such as sexism and racism, ageism focuses on a group of people that ageists, if all goes well, will one day be a part of [12].
Montepare and Zebrowitz [13] state that ageism starts very early because children adopt the age stereotypes of their culture at a very young age. The lifetime exposure to negative age stereotypes makes these stereotypes richer, more accessible, and more deeply entrenched in older individuals. Additionally, an age-related decline in cognitive control makes it more difficult to suppress these negative beliefs [14], leading to self-directed ageism. Self-directed ageism was therefore found to be the most common form (81% of participants) by Allen et al. [15] in their study of the prevalence of everyday ageism and its relationship to health in 2035 older adults.
In the search for determinants of ageism, Marques and colleagues [16] identified several sets of determinants that contribute to other- and self-directed ageism. They found that age, fear of death and fear of aging were associated with other-directed ageism, while poor mental and physical health were more likely to be associated with self-directed ageism. Gekoski and Knox [17] found prejudice against frail or sick older adults, but concluded that it is not age itself, but rather specific age-related characteristics, such as slowness or depression in older people, that lead to negative beliefs and attitudes. The effect of age on mental health professionals perceptions was examined by James and Haley [18]. They concluded that not only age, but also poor health posed a risk for negative perceptions, as a result, older people in poorer health may be at double risk when seeking help and support.
In its general report on ageism, the WHO [8] concluded that ageism has a negative impact on the health, well-being and rights of people in general. Among older people, it is associated with reduced life expectancy, weaker physical and mental health, delayed recovery from disability and cognitive decline. In addition, it limits older people’s ability to express their sexuality and may increase the likelihood of violence and elder abuse. The study of Allen et al. [15] showed that self-directed ageism was associated with the largest increases in risk for all health outcomes studied (physical health, mental health, chronic health problems, and depressive symptoms).
Although aging at home appears to positively affect quality of life [19], it can also become problematic when people’s functional capacity declines with age. Moreover, advanced age is also associated with frailty, a condition in which there is a high likelihood of adverse health outcomes such as dependence, disability, falls, need for long-term care, and death [20]. It is widely acknowledged that frailty has a negative impact of the quality of life of older people [21,22,23,24,25] whether both concepts are viewed from a biomedical or multidimensional perspective [23].
As aging in place is increasingly the policy choice, more frail community-dwelling older people are to be expected. As mentioned above, frailty and quality of life are negatively related, and frailty poses a risk for ageism. Therefore, the purpose of this study is to explore to what extent self-directed ageism affects the relationship between frailty and quality of life in community-dwelling older adults.
2 Method
2.1 Aim
The aim of this study is to explore the role of self-directed ageism in the relationship between frailty and quality of life in community-dwelling older people. Although studies already explored the association between frailty and quality of life, and others explored the association between ageism and quality of life, with only a few exploring self-directed ageism [26], this is, to our knowledge, the first study to explore the association between self-directed ageism, frailty, and quality of life.
2.2 Study design and data collection
This study is a secondary data-analysis on data from the Belgian Ageing Studies (BAS), a research project collecting information on community-dwelling people aged 60 years and older [27], conducted in the Dutch speaking part of Belgium since 2004. Participant selection is described extensively in the methodological paper by De Donder and colleagues [28]. Data for this highly structured cross-sectional survey was collected using a self-administered questionnaire focusing on various aspects related to quality of life and living conditions in later life. The original questionnaire was expanded in 2009 and 2015 with questions on quality of life and the Comprehensive Frailty Assessment Instrument [29]. A stratified sample, based on census data by gender and age (60–69, 70–79, 80 +), was drawn in four communities between 2017 and 2019. A final total of 1895 participants were included, the minimum number of participants from one community was 319. All questionnaires were entered in Microsoft Access. The ethics committee of the Vrije Universiteit has approved the study protocol of the BAS (B.U.N. 143,201,111,521). More information on the BAS can be found in De Witte et al. [29].
2.3 Measures
All measurements used in this study are integral components of the Belgian Ageing Studies research project’s questionnaire.
2.3.1 Sociodemographic variables
The BAS collects several sociodemographic variables of community-dwelling older adults from which age, gender and marital status are selected for the current study.
2.3.2 Assessment of frailty
The Comprehensive Frailty Assessment Instrument (CFAI) is used to assess frailty in a multidimensional way. This self-report instrument was developed by De Witte and colleagues [29] to screen frailty in community-dwelling older people and the instrument displayed good psychometric properties. The CFAI consists of 23 items organized within four domains of frailty: the physical (general health), psychological (mood disorders and emotional loneliness), social (social loneliness and social support) and environmental domain (housing condition and location). Based on the author’s instructions, domain scores were calculated and summed to obtain a total score for the CFAI, resulting in a score ranging from 0 to 100. Higher scores on the CFAI are related to more severe frailty. A detailed description of the CFAI can be found in De Witte et al. [29].
2.3.3 Assessment of quality of life
For this study, we used respondents' quality of life assessment. For this purpose, they indicated the number corresponding to their quality of life at that time on a numeric rating scale. The scale ranged from zero to ten, with zero representing very poor quality of life and ten representing very good quality of life.
2.3.4 Assessment of self-directed ageism
The BAS also includes 11 statements assessing self-directed ageism in community-dwelling older people.
In previous research De Donder et al. [30] and Van Regenmortel et al. [31] already used these 11 statements to explore ageism. These statements are shown in Table 3. Respondents could indicate the extent to which they agreed with these statements on a 5-point Likert scale, ranging from completely disagree (score 1) to completely agree (score 5). An exploratory factor analysis was used to explore the underlying theoretical structure.
2.4 Data-analysis
First, the respondents were divided into the three age categories used by the BAS: one from 60 to 69 years, one from 70 to 79 years and one from 80 years and older. Subsequently, the 11 statements extracted from the Belgian Ageing Studies (BAS) were subjected to exploratory factor analysis to elucidate their grouping and to construct a questionnaire aimed at measuring the underlying variable of 'self-directed ageism'. Before conducting the factor analysis, a correlation matrix was generated to examine the interrelations among the statements. Given their collective relevance to self-directed ageism, these statements were expected to exhibit moderate correlations with each other. As per Field [32] excessively high (> 0.8) or low (< 0.3) correlations may respectively indicate redundancy or lack of association with the underlying construct of self-directed ageism. Subsequently, the appropriateness of performing exploratory factor analysis was determined through the Kaiser–Meyer–Olkin measure of sampling adequacy (KMO) and Bartlett’s test of sphericity. Following this, the varimax rotation method was employed to explore the underlying structure of the statements. Varimax rotation aims to optimize the dispersion of loadings within factors, facilitating clearer interpretation of factor clusters. Any statement with a factor loading below 0.3 was deemed insufficiently correlated and consequently excluded from further analysis, ensuring alignment between the theoretical model and the empirical data.
The internal consistency of the scale was assessed using Cronbach’s alpha coefficient, a widely utilized measure of scale reliability. Cronbach’s alpha assesses the extent of correlation among scale items, with values around 0.8 considered indicative of strong reliability [32]. Additionally, split-half reliability was evaluated using the Spearman-Brown coefficient, which was calculated via the odd–even method. This method involves dividing the scale into two halves based on the odd and even statements. Consistency between the results from these two versions indicates greater internal reliability of the instrument.
Next, the distribution of variables was assessed using normality test (skewness and kurtosis). According to the data distribution, the results were expressed as mean and standard deviation (normal distribution) or median. Next, scores on the ageism scale were calculated, with high scores indicating high self-directed ageism. In the next step, scores on CFAI were calculated, as suggested by the developers [29], with high scores indicating high frailty. To compare the scores on ageism, frailty, and quality of life among men and women and among the three age groups, a combination of statistical tests was used. Specifically, independent T-tests or Mann–Whitney U tests were used for comparisons between genders, and One-Way-Anova or Kruskal–Wallis tests were used to compare scores across the age groups. The choice between parametric and non-parametric tests was made based on the distribution of the data, homogeneity of variances was checked using Levene’s test. Correlations between variables were calculated for the total sample, as well as for men and women and for the three age groups, using Pearson’s correlation coefficient (normally distributed data) or Spearman’s rank correlation coefficient (non normally distributed data). Finally, to examine whether self-directed ageism was a mediating variable in the relationship between frailty and quality of life, a mediation analysis was conducted using Hayes PROCESS V3.5 macro in the statistical software SPSS. Gender, age, and marital status were entered as covariates. The significance level was set at p < 0.05 and all analyses were performed using IBM SPSS Statistics (Version 25).
To provide as much as possible information about the data distribution, mean, standard deviation and median were calculated for skewed data and when comparing groups.
3 Results
3.1 Respondents’ characteristics
Table 1 presents the descriptive statistics of 1895 respondents who participated in the BAS between 2016 and 2021. Their age varied between 60 and 101 years old, with an average age of 72.15 (SD = 8.80). Exactly 46% belonged to the category between 60 and 69 years, 30.5% to the category between 70 and 79 years and 23.5% to the category 80 years and older. The majority were female (52.8%) and married (64.5%), less than one fifth were widowed (17.7%) and almost one-tenth were divorced (9.3%).
3.2 Development of self-directed ageism scale
The correlation matrix, generated prior to conducting the exploratory factor analysis, is presented in Table 2. As indicated in the table, correlations for several statements (8, 10, and 11) were below 0.30. The absence of correlations exceeding 0.80 indicates the absence of multicollinearity, thus all 11 statements underwent exploratory factor analysis to explore the underlying structure of the data and enhance the reliability of the measurement instrument. The results of the factor analysis are presented in Table 3. The Kaiser-Meyer Olkin measure of sampling adequacy was found to be good (0.923), and a significant (p < 0.001) Bartlett’s test of sphericity indicated that factor analysis was appropriate.
Initially, a model was tested, including al items (model 1). This proposed a two-component solution, explaining 57.05% of the variance. However, as observed in Table 3, some statements showed high loadings on both components (e.g. statements 2 and 6). Furthermore, statement 8 was identified as problematic during reliability analysis (corrected item total correlation: 0.185), and was subsequently removed, resulting in model 2. Model 2 represents a one-component solution, explaining 51.25% of the variance, with all factors loading above 0.3. The Cronbach’s alpha of this model was 0.886, with a low corrected item—total correlation of 0.327 for item 10. Removing item 10 suggested an increase of Cronbach’s alpha. Thus, item 10 was eliminated, yielding model 3. Factor analysis of this third model revealed a one-component solution explaining 55.53% of the variance. Reliability analysis on this model showed a Cronbach’s alpha of 0.897. Item 11 exhibited the lowest corrected item-total correlation, and its removal suggested an increased Cronbach’s alpha. Consequently, item 11 was omitted in model 4, resulting in the final model explaining 58.86% of the variance with a Cronbach’s alpha of 0.898., indicating good overall reliability. Further deletions of other items led to a decrease in Cronbach’s alpha, confirming model 4 as the definitive model. Finally, split-half reliability was assessed using the odd–even method, resulting in Spearman-Brown coefficient of 0.906.
The exploratory factor analysis resulted in a new self-directed ageism scale consisting of eight items. The scale has a range of 8 to 40, with higher scores indicating more self-directed ageism.
3.3 Scores on frailty, self-directed ageism, and quality of life
Center and dispersion measures were calculated for frailty, self-directed ageism, and quality of life and are presented in Table 4. Respondents had a mean score of 26.94 on frailty with a minimum of 0 and a maximum of 73.96. After applying the cut-offs, as determined by De Witte and colleagues [33], this resulted in 36.9% classified as no to low frail, 42.9% as mild frail and 20.2% as high frail.
Women scored significantly higher on frailty than men (t(1537.49) = − 4.63, p < 0.001). Additionally, significant differences in frailty scores were detected across all age groups (H(2) = 126.39, p < 0.001). Post-hoc pairwise comparisons indicated that the 60–69 years and the 70–79 years groups scored significantly lower than the 80 and older group.
Regarding self-directed ageism, the mean score of 23.62 was calculated from the total sample. No significant differences in self-directed ageism scores were found between women and men (t(1740) = 0.010, p = 0.992), nor across age groups (H(2) = 5.095, p = 0.078).
For quality of life, the median score was 8, ranging from 0 to 10. No significant differences in quality of life ratings between women and men were found (U = 429,509.50, p = 0.162). However, a significant difference was observed among age groups (H(2) = 25.28, p < 0.001). Post-hoc pairwise comparisons indicated that the group aged 80 and older reported significantly lower quality of life compared to the 60–69 years and 70–79 years groups.
3.4 Correlations between frailty, self-directed ageism, and quality of life
Self-directed ageism correlated positively with frailty. Quality of life was negatively correlated with frailty and with ageism. Similar associations were found for age groups and gender, with slightly higher correlations for women and those in the 60–69 age group. A summary of these correlations is shown in Table 5.
3.5 Mediation analysis
The outcomes of the mediation analysis are summarized in Table 6. The result shows that when self-directed ageism is not included in the model, as seen in C-path, frailty negatively predicts quality of life (ß = − 0.051) explaining 24.54% of the variance.
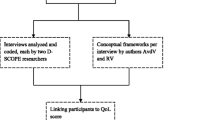
Frailty positively affects self-directed ageism (ß = 0.150), see A-path, while self-directed ageism in turn has a negative affect on quality of life (ß = − 0.019), see B-path. Indirect effects analysis shows that self-directed ageism significantly mediates the relationship between frailty and quality of life (ab = − 0.003). The 95% confidence interval does not include zero, pointing towards, although small, a genuine indirect effect. The results also suggest that even after accounting for the mediating role of self-directed ageism, frailty still has a negative impact on quality of life (ß = − 0.048) (C’-path). The model with self-directed ageism as a mediator explains 25.34% of the variance in quality of life. The negative coefficient indicates that quality of life decreases as frailty and/or self-directed ageism increases. A conceptual model with self-directed ageism as mediator is shown in Fig. 1.
4 Discussion
The present study explored the relationship between frailty, self-directed ageism, and quality of life in a sample of 1895 Flemish older people living at home. The underlying structure of the 11 statements on self-directed ageism was investigated through exploratory factor analysis. The structure of the new self-directed ageism scale captures the same underlying construct of self-directed ageism as identified by Van Regenmortel et al. [31]. The advantages of our new self-directed ageism scale include robust internal consistency (Cronbach’s alpha = 0.898, Spearman-Brown coefficient = 0.906), a single-component structure, and minimal participant burden owing to its concise nature of only 8 statements. As Burton et al. [34] suggest the use of brief measures is advantageous when broad assessments are necessary. The self-directed ageism scale explained 58.86% of the variance in self-directed ageism, showed to be internally consistent, with a Cronbach’s α of 0.898, which is, according to Field [32], high.
In this study, a prevalent phenomenon of self-directed ageism was identified among the majority of respondents, manifesting itself to varying degrees. Remarkably, only a minority reported experiencing no self-directed ageism at all. Furthermore, no differences between men and women, nor between age groups were found. These results are in line with the findings of Palmore [35] and partially contrary to the findings of Rippon et al. [36] who saw ageism increasing with age, peaking in the oldest age group. Concerning frailty, the majority of respondents were identified as mild to highly frail, with women and the oldest age group scoring highest. The latter was also reported by Collard et al. [37] and Gobbens and van der Ploeg [38]. Regarding quality of life, the oldest age group reported the lowest scores on quality of life, as reported by Bowling [39], Gobbens and van der Ploeg [38] and Henchoz [40].
Correlations between self-directed ageism, frailty and quality of life are consistent with previous findings. A positive correlation between self-directed ageism and frailty was found, which confirms the study of Zora et al. [41], while quality of life correlated negatively with frailty, which is in line with Papathanasiou et al. [42], Vanleerberghe et al. [22] and Veronese et al. [43], and ageism as explored by Chang et al. [44].
Mediation analysis indicated frailty and self-directed ageism as predictors of quality of life in community-dwelling older people. Frailty increases self-directed ageism, while self-directed ageism reduces quality of life. The direct effect of frailty on quality of life, in presence of self-directed ageism as mediator, was found significant. Therefore, it can be concluded that, in this study, self-directed ageism partially mediated the relationship between frailty and quality of life.
According to Levy and Banaji [45] and Montepare and Zebrowitz [13], age stereotyping already starts in childhood. Thus, by the time a person belongs to the older age group , they had already been exposed to age stereotypes for many years. Since this was done subconsciously, no defenses were built up against its negative impact, making older people being particularly susceptible to self-directed ageism. Our results indicate that frailty positively influences self-directed ageism, making frail older persons even more susceptible, which in turn negatively impacts on their quality of life. Since frailty has a negative impact on quality of life directly, but also indirectly, through ageism, efforts should be made to reduce frailty and reduce ageism. Indeed, early detection of frailty allows appropriate interventions to reduce frailty, whereas combating ageism will result in a decrease of ageism as well as self-directed ageism, which will undoubtedly have a positive impact on the quality of life of older people living at home.
This study has a number of limitations. First, we conducted a cross-sectional study; consequently, no causality or evolution in time can be determined [46]. Therefore, longitudinal research or life span studies in future research are recommended. Second, self-administered questionnaires were used, a data-collection method susceptible to social desirability bias. However, due to the subjective nature of frailty, self-directed ageism and quality of life this limitation will have, in our opinion, a limited effect. Third, our results reflect only the Flemish situation. Therefore, international studies are recommendable. On the other hand, the large dataset of community dwelling older people and the proportional stratified sampling of the BAS are strong points in this study. Moreover, to the best of our knowledge, this is the first study exploring the relationship between frailty, quality of life and self-directed ageism.
5 Conclusion
The purpose of this study was to explore the role of self-directed ageism in the relationship between frailty and quality of life in community-dwelling older adults. Most respondents were identified as mild frail, experienced self-directed ageism, and those 80 or older rated their quality of life lower. The present study showed that frailty negatively correlates with quality of life and this relationship is partially mediated by self-directed ageism. Efforts to reduce frailty, ageism and self-directed ageism are therefore strongly recommended as they impact community-dwelling older people’s quality of life.
Data availability
The data that support the findings of this study are available from Belgian Ageing Studies (BAS), but restrictions apply to the availability of these data, which were used under license for the current study and so are not publicly available. The data are, however, available from the authors upon reasonable request and with the permission of Belgian Ageing Studies (BAS).
References
United Nations Department of Economic and Social Affairs. World population prospects: the 2017 revision, key findings and advance table. 2017. Report No.: ESA/P/WP/248. https://www.un.org/development/desa/publications/world-population-prospects-the-2017-revision.html.
United Nations Department of Economic and Social Affairs. World population prospects 2022: summary of results. 2022. Report No.: UN DESA/POP/2022/TR/NO. 3.
Statbel. (n.d.). Belgium in figures [Data file]. https://bestat.statbel.fgov.be. Accessed 4 Mar 2022.
Federaal Planbureau en Statbel. Demografische vooruitzichten 2020–2070. [Demographic outlook 2020–2070]. 2021.
De Witte N, Smetcoren AS, De Donder L, Dury S, Buffel T, Kardol T, et al. Een huis? Een thuis!: over ouderen en wonen [A house? A home!: about older people and living]. Brugge: Vanden Broele; 2012.
Officer A, Schneiders ML, Wu D, Nash P, Thiyagarajan JA, Beard JR. Valuing older people: time for a global campaign to combat ageism. Bull World Health Organ. 2016;94(10):710-710A. https://doi.org/10.2471/blt.16.184960.
Butler RN. Age-ism: another form of bigotry. Gerontologist. 1969;9(4_Part_1):243–6. https://doi.org/10.1093/geront/9.4_part_1.243.
World Health Organization. Global report on ageism. 2021. https://www.who.int/teams/social-determinants-of-health/demographic-change-and-healthy-ageing/combatting-ageism/global-report-on-ageism. Accessed 10 Apr 2022.
Bratt C, Abrams D, Swift HJ. Supporting the old but neglecting the young? The two faces of ageism. Dev Psychol. 2020;56(5):1029. https://doi.org/10.1037/dev0000903.
Greenberg J, Pyszczynski T, Solomon S. The causes and consequences of a need for self-esteem: a terror management theory. In: Baumeister RF, editor. Public self and private self. New York: Springer New York; 1986. p. 189–212.
Martens A, Goldenberg JL, Greenberg J. A terror management perspective on ageism. J Soc Issues. 2005;61(2):223–39. https://doi.org/10.1111/j.1540-4560.2005.00403.x.
Palmore E. Ageism comes of age. Gerontologist. 2003;43(3):418–20. https://doi.org/10.1093/geront/43.3.418.
Montepare JM, Zebrowitz LA. A social-developmental view of ageism. In: Nelson TD, editor. Ageism: stereotyping and prejudice against older persons. Cambridge (MA): MIT Press; 2002. p. 77–125. https://doi.org/10.7551/mitpress/1157.003.0007.
Henry JD, Coundouris SP, Craik FI, von Hippel C, Grainger SA. The cognitive tenacity of self-directed ageism. Trends Cogn Sci. 2023. https://doi.org/10.1016/j.tics.2023.03.010.
Allen JO, Solway E, Kirch M, Singer D, Kullgren JT, Moïse V, et al. Experiences of everyday ageism and the health of older US adults. JAMA Netw Open. 2022;5(6): e2217240-e. https://doi.org/10.1001/jamanetworkopen.2022.17240.
Marques S, Mariano J, Mendonça J, De Tavernier W, Hess M, Naegele L, et al. Determinants of ageism against older adults: a systematic review. Int J Environ Res Public Health. 2020;17(7):2560. https://doi.org/10.3390/ijerph17072560.
Gekoski WL, Knox VJ. Ageism or healthism? Perceptions based on age and health status. J Aging Health. 1990;2(1):15–27. https://doi.org/10.1177/089826439000200102.
James JW, Haley WE. Age and health bias in practicing clinical psychologists. Psychol Aging. 1995;10(4):610. https://doi.org/10.1037/0882-7974.10.4.610.
Bowling A, Gabriel Z, Dykes J, Dowding LM, Evans O, Fleissig A, et al. Let’s ask them: a national survey of definitions of quality of life and its enhancement among people aged 65 and over. Int J Aging Hum Dev. 2003;56(4):269–306. https://doi.org/10.2190/BF8G-5J8L-YTRF-6404.
Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci. 2004;59(3):M255–63. https://doi.org/10.1093/gerona/59.3.M255.
Bilotta C, Bowling A, Casè A, Nicolini P, Mauri S, Castelli M, et al. Dimensions and correlates of quality of life according to frailty status: a cross-sectional study on community-dwelling older adults referred to an outpatient geriatric service in Italy. HealthQual Life Outcomes. 2010;8(56):5. https://doi.org/10.1186/1477-7525-8-56.
Vanleerberghe P, De Witte N, Claes C, Verté D. The association between frailty and quality of life when aging in place. Arch Gerontol Geriatr. 2019;85:8. https://doi.org/10.1016/j.archger.2019.103915.
Renne I, Gobbens RJ. Effects of frailty and chronic diseases on quality of life in Dutch community-dwelling older adults: a cross-sectional study. Clin Interv Aging. 2018;13:325. https://doi.org/10.2147/cia.s156116.
Gobbens RJJ, van Assen MALM. Associations between multidimensional frailty and quality of life among Dutch older people. Arch Gerontol Geriatr. 2017;73:69–76. https://doi.org/10.1016/j.archger.2017.07.007.
Sánchez-García S, García-Peña C, Salvà A, Sánchez-Arenas R, Granados-García V, Cuadros-Moreno J, et al. Frailty in community-dwelling older adults: association with adverse outcomes. Clin Interv Aging. 2017;12:1003. https://doi.org/10.2147/CIA.S139860.
Steward AT, Hasche L, Laser JA. Do internalized age stereotypes mediate the relationship between volunteering and social connectedness for adults 50+? J Aging Stud. 2022;61:101031. https://doi.org/10.1016/j.jaging.2022.101031.
Verté D, De Witte N, De Donder L. Schaakmat of aan zet? Monitor voor lokaal ouderenbeleid in vlaanderen. [Checkmate or to move? Guidelines for local policy towards older people in flanders]. Vandenbroele; 2007.
De Donder L, Dury S, Buffel T, De Witte N, Verté D. Ouderen als actieve bouwers aan beleid: Belgian Ageing Studies als case [Older people as active policy builders: Belgian Ageing Studies as a case study]. Tijdschrift Klinische Psychologie. 2012;42(1):54–64.
De Witte N, Gobbens R, De Donder L, Dury S, Buffel T, Schols J, et al. The comprehensive frailty assessment instrument: development, validity and reliability. Geriatr Nurs. 2013;34(4):274–81. https://doi.org/10.1016/j.gerinurse.2013.03.002.
De Donder L, De Witte N, Dury S, Buffel T, Verté D. Individual risk factors of feelings of unsafety in later life. Eur J Ageing. 2012;9:233–42. https://doi.org/10.1007/s10433-012-0226-8.
Van Regenmortel S, De Donder L, Smetcoren A-S, Lambotte D, De Witte N, Verté D. Accumulation of disadvantages: Prevalence and categories of old-age social exclusion in Belgium. Soc Indic Res. 2018;140(3):1173–94. https://doi.org/10.1007/s11205-017-1817-8.
Field A. Discovering statistics using IBM SPSS statistics. 4th ed. Newcastle upon Tyne: Sage; 2013.
De Witte N, Hoeyberghs L, Vertè E, De Donder L, Dierckx E, Verté D, Kempen GIJM, Schols JMGA. The comprehensive frailty assessment instrument enables to detect multidimensional frailty in community dwelling older people. Healthy Aging Res. 2018. https://doi.org/10.12715/har.2018.7.13.
Burton A, Dean S, Demeyin W, Reeves J. Questionnaire measures of self-directed ageing stereotype in older adults: a systematic review of measurement properties. Eur J Ageing. 2021;18:117–44. https://doi.org/10.1007/s10433-020-00574-7.
Palmore E. The ageism survey: first findings. Gerontologist. 2001;41(5):572–5. https://doi.org/10.1093/geront/41.5.572.
Rippon I, Kneale D, de Oliveira C, Demakakos P, Steptoe A. Perceived age discrimination in older adults. Age Ageing. 2014;43(3):379–86. https://doi.org/10.1093/ageing/aft146.
Collard RM, Boter H, Schoevers RA, Oude Voshaar RC. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc. 2012;60(8):1487–92. https://doi.org/10.1111/j.1532-5415.2012.04054.x.
Gobbens RJ, van der Ploeg T. The development of multidimensional frailty over seven years A longitudinal study among Dutch community-dwelling older people using the Tilburg Frailty Indicator. Arch Gerontol Geriatr. 2021;95:104393. https://doi.org/10.1016/j.archger.2021.104393.
Bowling A. Enhancing later life: how older people perceive active ageing? Aging Ment Health. 2008;12(3):293–301. https://doi.org/10.1080/13607860802120979.
Henchoz Y, Abolhassani N, Büla C, Guessous I, Goy R, Santos-Eggimann B. Change in quality of life among community-dwelling older adults: population-based longitudinal study. Qual Life Res. 2019;28(5):1305–14. https://doi.org/10.1007/s11136-019-02108-w.
Zora S, Cella A, Poli S, Veronese N, Zini E, Giannoni P, et al. “Ageism” is associated with self-reported multidimensional frailty in community-dwelling older subjects: a population-based study. Front Med. 2021. https://doi.org/10.3389/fmed.2021.734636.
Papathanasiou IV, Rammogianni A, Papagiannis D, Malli F, Mantzaris DC, Tsaras K, et al. Frailty and quality of life among community-dwelling older adults. Cureus. 2021. https://doi.org/10.7759/cureus.13049.
Veronese N, Noale M, Cella A, Custodero C, Smith L, Barbagelata M, et al. Multidimensional frailty and quality of life: data from the English Longitudinal Study of Ageing. Qual Life Res. 2022;31(10):2985–93. https://doi.org/10.1007/s11136-022-03152-9.
Chang E-S, Kannoth S, Levy S, Wang S-Y, Lee JE, Levy BR. Global reach of ageism on older persons’ health: a systematic review. PLoS ONE. 2020;15(1): e0220857. https://doi.org/10.1371/journal.pone.0220857.
Levy BR, Banaji MR. Implicit ageism. In: Nelson TD, editor. Ageism: stereotyping and prejudice against older persons. Cambridge: MIT Press; 2002. p. 49–75. https://doi.org/10.7551/mitpress/1157.003.0006.
Field A. Discovering statistics using SPSS. 3rd ed. Newcastle upon Tyne: Sage; 2009.
Acknowledgements
The first author wishes to express her deep gratitude to the founders of the Belgian Ageing Studies for using their data and to the Education Centre Nursing and Research Centre 360° Care and Well-being of University of Applied Sciences HOGENT for supporting this research.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualization: Patricia Vanleerberghe, Nico De Witte. Methodology: Patricia Vanleerberghe, Nico De Witte. Formal analysis and investigation: Patricia Vanleerberghe, Jorrit Campens, Dominique Verté, Nico De Witte. Writing—original draft preparation: Patricia Vanleerberghe, Nico De Witte. Writing—review and editing: Claudia claes, Jorrit Campens, Dominique Verté, Nico De Witte. Supervision: Claudia Claes, Nico De Witte.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study is a secondary data-analysis on data from the BAS. The BAS were performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the Vrije Universiteit Brussel (B.U.N. 143,201,111,521). Candidates were verbally invited to participate in the BAS (primary study); implied consent was obtained by completing the questionnaire.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vanleerberghe, P., Claes, C., Campens, J. et al. The mediating role of self-directed ageism on frailty and quality of life in community-dwelling older people. Discov Soc Sci Health 4, 27 (2024). https://doi.org/10.1007/s44155-024-00087-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44155-024-00087-z