Abstract
Although patients experiencing food insecurity commonly screen positive for a myriad of social determinants of health (SDOH) needs and chronic medical conditions influenced by diet, few studies have investigated associations within both uninsured and food insecure populations. We screened patients for food insecurity using the USDA six-item short form between October 2021 and April 2022. We then evaluated associations of food security status with nine separate SDOH needs and eight chronic medical conditions. In this cross-sectional study, of the 190 patients seen at a student-run free clinic serving patients without health insurance, 135 (71%) completed the SDOH survey. We identified chronic medical conditions via retrospective chart review and analyzed associations using multivariable logistic regressions adjusted for age and sex. Uninsured participants experiencing food insecurity (n = 22,16.3%) requested more support for: medications (adjusted odds ratio [AOR] = 7.28; 95% Confidence Interval [95% CI] = 2.33–23.2); p-value [P] = < 0.001, housing (AOR = 9.99; 95% CI = 2.29–48.7; P = 0.002), utilities (AOR = 3.94; 95% CI = 1.07–13.5; P = 0.03), mental health resources (AOR = 4.54; 95% CI = 1.66–12.5; P = 0.003), health insurance (AOR = 2.86; 95% CI = 1.09–8.22; P = 0.04), and dental care (AOR = 3.65; 95% CI = 1.26–13.3; P = 0.03). These participants were more likely to have anxiety (AOR = 3.26; 95% CI = 1.23–8.38; P = 0.02) and depression (AOR = 2.88; 95% CI = 1.01–7.80; P = 0.04) diagnoses or symptoms. We also discovered that individuals aged 18–50 experiencing food insecurity had a higher number of health conditions (AOR = 6.3455; 95% CI = 1.49–26.99; P = 0.01), underscoring the profound impact of SDOH in younger populations. Understanding the interplay between food insecurity, SDOH needs, and medical conditions informs interventions, including food distribution programs and enhanced mental health resources.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Background
The four main dimensions of food security encompass food availability, economic and physical access to food, food utilization, and stability of the aforementioned over time [1]. Disruption to any of these dimensions can lead to food insecurity, “a household-level economic and social condition of limited or uncertain access to adequate food,” which has significant implications for health and wellbeing [2, 3]. In the U.S., food insecurity disproportionately affects individuals aged 18–34, females, low-income individuals, and those identifying as non-Hispanic Black [4, 5]. Individuals experiencing food insecurity often face other social determinants of health (SDOH) challenges, such as a lack of health insurance and stable housing or the ability to afford medications and dental care [6,7,8]. Food insecurity is associated with a myriad of health issues, including cognitive dysfunction, mental health problems, obesity, diabetes, anemia, asthma, hypertension, chronic kidney disease, and hyperlipidemia [3, 9,10,11]. The COVID-19 pandemic has also exacerbated the issue for certain communities, with 10.5% of households experiencing food insecurity at some point during 2020 [12,13,14].
In spite of programs like the Supplemental Nutrition Assistance Program (SNAP), designed to combat food insecurity and reduce estimated annual healthcare costs, many households still struggle to access nutritious food options [15, 16]. The prevalence of food insecurity and its associations vary considerably based on community and population characteristics, complicating efforts to address the issue [17, 18]. This variability underscores the importance of local needs assessments and food security programs to cater to each community’s unique needs [19]. To date, there has been minimal research into social or health-related risk factors that may be associated with food insecurity among uninsured individuals [20, 21], with even fewer studies focusing on this population in Wisconsin.
In this study, we describe a 6-month needs assessment conducted at the Saturday Clinic for the Uninsured, the student-run free clinic associated with the Medical College of Wisconsin. Supported by a community hospital and staffed by volunteer physicians, pharmacists, and medical and pharmacy students, this clinic exclusively serves patients without health insurance, providing primary and specialty care, including mental health care, and social work services free of charge.
While many studies describe food insecurity associations between one to two SDOH needs or health outcomes [22, 23], we conducted a more comprehensive analysis of how food insecurity may predict association with nine other SDOH needs, including utility assistance, legal concerns, and substance use resources, not previously studied. Additionally, we explored food insecurity associations with eight chronic medical conditions and whether COVID-19 affected patient responses to the SDOH needs assessment. By understanding these diverse associations with food insecurity, we can not only inform the future development of an evidence-based, accessible food assistance program at Saturday Clinic for the Uninsured, but also gain valuable insights into the uninsured population.
2 Methods
2.1 Participants
The study population consists of patients who completed the SDOH survey during their in-person or telehealth visit at Saturday Clinic for the Uninsured in Milwaukee, WI between October 2021 and April 2022. The inclusion and exclusion criteria were based on the patients seen at the clinic, which exclusively serves adult patients (≥ 18 years of age) of all genders, ethnicities, and languages, without health insurance. Clinic volunteers verbally administered the SDOH survey during appointments after obtaining patient consent.
2.2 Data collection & measures
The SDOH survey questions were developed by the research team, clinic social worker, and medical director, based upon previously conducted research [24, 25], observed patient needs, and clinic processes. Participants responded Yes/No when asked if they: had ever skipped medications to save money, were worried about not having stable housing, needed assistance paying utility bills, had questions about legal issues related to immigration, child support, or eviction, were interested in learning about educational or work opportunities, would like resources for substance use, were interested in mental health services, would like information regarding health insurance options, and would like free or low-cost dental health. We refer to these SDOH needs through the following labels: medications, housing, utilities, legal concerns, education or work opportunities, substance abuse resources, mental health resources, health insurance, and dental care.
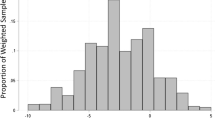
Food insecurity was assessed using the USDA “Household Food Security Survey Module: Six-Item Short Form,” a reliable and validated scale [26]. The USDA 6-item short form notes raw scores of 0–1 as high or marginal food security, scores of 2–4 as low food security, and scores of 5–6 as very low food security [26]. Regardless of score, we asked all participants if they would like food-related resources, which consisted of zip code-specific food pantries and services, information on Impact 2-1-1 (a local social services helpline), separate virtual visits to facilitate SNAP or Medicaid (BadgerCare) applications, health and diet-related fliers, and other tailored programs depending on eligibility.
We collected participant self-reported demographics, including age (date of birth), sex assigned at birth (male, female, unknown), race (American Indian/Alaskan Native, Asian, Black or African American, Native Hawaiian or other Pacific Islander, White, Unknown, Decline to Specify, and Other Race), Hispanic or Latino ethnicity (Yes, No, or Decline), and zip code (inferred county). We also asked participants if the COVID-19 pandemic affected any of their responses by reviewing the list of SDOH needs assessed.
A select group of medical student volunteers administered the SDOH survey as part of clinic procedures after patients provided verbal consent. These medical students were trained on verbal survey administration, data collection into a REDCap database [27], and documentation into the Electronic Health Record. Additionally, volunteers were trained on selection and distribution of resources based on patients’ social contexts. Clinic volunteers routinely assessed SDOH needs unless the patient completed the survey in the previous 4 weeks. Patients usually had follow-up clinic visits every three months and during these subsequent visits, if they completed the SDOH survey again, we collected information on the usefulness of resources they were previously provided. When necessary for communication with non-English speaking patients, clinic volunteers used certified medical interpreters via a telephone service.
The research team conducted chart review on participants that completed the SDOH survey to determine whether they had the following conditions based on diagnoses noted in the medical record, most recent lab values (if available in the last 6 months), and whether participants were on active medications for these conditions. The chart review was conducted at least one month after initial completion of the survey to ensure that new lab results were included in our data analysis. Lab records older than 6 months were excluded. We sought to standardize and objectively track these chronic medical conditions using multiple sources as EMR data can sometimes contain old or missing diagnoses [28]. The specific criteria for each chronic medical condition include:
2.2.1 Obesity
Diagnostic inclusion criteria included a clinical diagnosis and/or body mass index (BMI) ≥ 30 kg/m2 [29]. We calculated BMI using participant height and weight from the most recent clinic visit.
2.2.2 Hypertension
Diagnostic inclusion criteria included any 1 or more of the following: a clinical diagnosis, an active prescription for anti-hypertensive medications, and/or meeting American Heart Association criteria for hypertension (elevated systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg across 2 office visits) [30].
2.2.3 Type 2 Diabetes
Diagnostic inclusion criteria included a clinical diagnosis, elevated hemoglobin A1c (HbA1c) values ≥ 6.5% (Normal < 5.7%, Prediabetes 5.7% to 6.4%) [31], or an active prescription for a diabetes medication. We did not consider fasting blood glucose values as these are not routinely obtained at the study clinic.
2.2.4 Dyslipidemia
Diagnostic inclusion criteria included a clinical diagnosis, abnormal lipid panel values (total cholesterol > 200 mg/dL, HDL < 40 mg/dL, LDL cholesterol > 130 mg/dL, and triglycerides > 150 mg/dL) [32], and/or active prescriptions for cholesterol or lipid lowering medications.
2.2.5 Chronic kidney disease (CKD)
Diagnostic inclusion criteria included a clinical diagnosis or abnormal values for creatinine (> 1.2 mg/dL) and eGFR (< 60 ml/min) [33].
2.2.6 Gastroesophageal reflux disease (GERD)
Diagnostic inclusion criteria included a recorded diagnosis or GERD-specific medication prescriptions. GERD is a clinical diagnosis.
2.2.7 Anxiety
Diagnostic inclusion criteria included a clinical diagnosis, abnormal Generalized Anxiety Disorder 7-item (GAD-7) scores (score ≥ 9, range 0–21), and/or active prescriptions for anxiolytic medication prescriptions. The GAD-7 questionnaire is widely used to screen for anxiety and has strong internal reliability and external validity [34]. GAD-7 scores range from 0–21 with scores of 0–4 signifying minimal anxiety, 5–9: mild anxiety, 10–14: moderate anxiety, and 15–21: severe anxiety.
2.2.8 Depression
Diagnostic inclusion criteria included a clinical diagnosis, abnormal Patient Health Questionnaire-9 (PHQ-9) scores (score ≥ 9, range 0–27), or anti-depressant medication prescriptions. The PHQ-9 is a widely used questionnaire to screen for depression and has strong internal reliability and external validity [35]. PHQ-9 scores range from 0–27 with scores of 1–4 signifying minimal depression, 5–9: mild depression, 10–14: moderate depression, 15–19: moderately severe depression, and 20–27: severe depression.
2.3 Analysis
To enhance statistical power, we grouped participants with scores of 0–1 as food secure and scores of 2–6 as food insecure like previous studies [19, 36]. We conducted statistical analysis using R 4.1.2. (R Foundation for Statistical Computing, Vienna, Austria) and the gtsummary [37] and MASS packages [38]. After excluding incomplete SDOH surveys, we calculated odds ratios using binomial multivariable logistic regression, with food security status as the independent variable and each SDOH need (Table 2) or chronic medical condition (Table 3) as the dependent variable and adjusting for participant age and sex. A separate model was created for each SDOH need or chronic medical condition and tested for significance (P ≤ 0.05).
Another model of ordered logistic regression was conducted by stratifying participants’ total number of health conditions into 0, 1, 2–3, and 4 + groups with food security status as the independent variable and adjusting for participant sex. To account for the known increase in health conditions with age, we stratified the analysis by age groups: "Under 50" and "50 and Over." Like the other models, significance was set to P ≤ 0.05.
3 Results
Of the 190 unique patients seen at the clinic from October 2021 to April 2022, 157 (82.63%) patients were administered the SDOH survey. We included 135 (71.1%) participants who responded to the complete SDOH survey in our analyses. Most participants completed the survey in-person (n = 132, 97.8%), fell between 50–59 years of age (mean age = 48.44 years ± 14.99 years), were female (n = 86, 64%), and resided in Milwaukee County (n = 124, 91.9%) (Table 1). The race of most participants was Black or African American (n = 55, 40.7%) and 36 participants (26.7%) were Hispanic or Latino (Table 1). Among SDOH needs and chronic medical conditions, most participants wanted resources for dental care (n = 81, 60%) and were diagnosed with hypertension (n = 71, 52.6%) (Table 1).
Among those experiencing food insecurity (n = 22, 16.3%), most came from Milwaukee County (n = 21, 95.5%) (Table 1). At the end of the SDOH survey, participants were asked if the COVID-19 pandemic affected their responses, and 24 participants (17.8%) responded “Yes” with most (n = 9, 37.5%) specifying a change in food security. Participants were asked if they would like food-related resources regardless of their food insecurity score and 36 participants (26.7%) requested some resources. Based on social context and interest, 30 (22.2%) participants received information on food pantries and 16 (11.9%) on SNAP (some received both resources). When participants visited the clinic again during this study period (~ 3 months later) and were asked about the usefulness of the resources they were provided, 7 (58.3%) out of 12 respondents found SNAP useful and 12 (66.7%) out of 18 respondents found food pantries useful.
We found that in comparison to participants who were food secure, those experiencing food insecurity had greater odds of needing support for medications (adjusted odds ratio [AOR] = 7.28; 95% Confidence Interval [95% CI] = 2.33–23.2); p-value [P] = < 0.001, housing (AOR = 9.99; 95% CI = 2.29–48.7; P = 0.002), utilities (AOR = 3.94; 95% CI = 1.07–13.5; P = 0.03), mental health resources (AOR = 4.54; 95% CI = 1.66–12.5; P = 0.003), health insurance (AOR = 2.86; 95% CI = 1.09–8.22; P = 0.04), and dental care (AOR = 3.65; 95% CI = 1.26–13.3; P = 0.03). (Table 2). We identified that food security status did not increase the odds of seeking resources for legal concerns, education or work opportunities, or substance use.
Participants experiencing food insecurity had higher odds of having anxiety (AOR = 3.26; 95% CI = 1.23–8.38; P = 0.02) and depression (AOR = 2.88; 95% CI = 1.01–7.80; P = 0.04) diagnoses or symptoms but not diagnoses of obesity, hypertension, diabetes, dyslipidemia, CKD, or GERD (Table 3). After stratifying participants by age into two groups, 'Under 50' and '50 and Over', we explored the association between food insecurity, sex, and the categorized number of health conditions (0, 1, 2–3, 4 +). Among individuals under 50 years of age, food insecurity significantly increased the likelihood of having a higher number of health conditions (AOR = 6.35; 95% CI = 1.49–26.99; P = 0.01), indicating a substantial impact of food insecurity on health outcomes in this younger cohort. Conversely, for participants aged 50 and over, food insecurity did not significantly influence the number of health conditions, suggesting the effects of food insecurity on health conditions may diminish with age or be overshadowed by other factors in older populations.
4 Discussion
In this 6-month cross-sectional study at a student-run free clinic, we applied the SDOH conceptual framework to evaluate relationships between food security status, various SDOH, and chronic medical conditions. The SDOH framework emphasizes the interconnectedness of various social, economic, and environmental factors that influence health outcomes. Our study also incorporated an exploration of the impact of the COVID-19 pandemic on participant responses to the SDOH needs assessment.
Our findings bolster existing evidence that supports the SDOH theoretical framework, underscoring the interconnectedness of various SDOH domains. Corroborating previous research, we found that low food security correlates with other financially-related SDOH, including the lack of health insurance, medication unaffordability, and housing cost burden [5, 8, 39,40,41]. Notably, our study confirms these associations in patients without insurance, an understudied population, and broadens the scope of these connections to utility assistance, dental care, and mental health services. Similar to past studies, we found a heightened risk of anxiety and depression diagnoses or symptoms among participants with food insecurity [13, 42].
Among the participants who reported that the COVID-19 pandemic affected their responses to the SDOH needs assessment, most noted an effect on their food security status. This highlights the profound influence of large-scale socioeconomic disruptions, such as a pandemic, on individual SDOH needs. The pandemic deepened pre-existing inequities within the workforce, triggering a ripple effect that has exacerbated food insecurity across diverse communities [14, 43]. From April 2021 to April 2022, the urban consumer price index for food in the Midwest region drastically increased, significantly affecting food affordability [44]. Consequently, participants likely faced decreased purchasing power during the study period.
Our stratified analysis offers a nuanced perspective on the relationship between food insecurity and health outcomes, revealing significant age-related disparities. While prior research has identified associations between food insecurity and various chronic medical conditions [9, 11, 45,46,47], our findings indicate that these associations are more pronounced in younger individuals under 50 years of age. Specifically, we observed a substantial increase in the likelihood of accumulating health conditions among younger participants experiencing food insecurity. Conversely, in the older cohort (50 and over), food insecurity did not significantly influence the number of health conditions, suggesting that the impact of food insecurity on chronic disease development may diminish with age or be mitigated by other factors prevalent in older populations.
These findings highlight the complex interplay between food insecurity, age, and health outcomes as contrary to prior research, we found no association between food insecurity and several chronic medical conditions, including obesity, hypertension, diabetes, and dyslipidemia, and CKD [9, 11, 45,46,47]. This lack of correlation may also be due to our study’s temporal context—the pandemic may have recently thrust some participants into food insecurity, making it difficult to observe the potential long-term effects within our study period. Another explanation may be that the role of insurance status is a greater driving factor than food insecurity status in chronic disease development. Both explanations warrant further investigations.
The prevalence of food insecurity in Wisconsin (7.2%) and Milwaukee County (11.8%) are lower than this study population (16.3%) [48]. However, the true prevalence may be even higher, as several participants requested food-related resources despite not screening as food insecure. This discrepancy could stem from the stigma associated with admitting food insecurity or limitations of the assessment tool, the USDA 6-item short form [26], which we had chosen to decrease respondent burden. To capture a more nuanced understanding of food insecurity, future studies could consider employing the more detailed 18-item survey [49].
Our preliminary findings on participant feedback for resources provided suggest that more than half of the participants that returned to clinic found SNAP and food pantry resources useful. We plan to continue collecting and analyzing data on resource usefulness to better tailor these offerings and effectively address the needs of patients served by this study clinic.
5 Limitations
Limitations of this study include the small sample size and cross-sectional design. The large confidence intervals from regression modeling have the potential to overemphasize or underestimate the associations investigated in this study. Another limitation is that the assessment tool we used to identify food insecurity, while validated, may not fully capture the complexity of food insecurity in households with children. Another critical consideration is the temporal context of the COVID-19 pandemic, which may have introduced unique, short-term influences on food insecurity and health outcomes not typically present outside such global crises. Based on these limitations, we interpret our findings with caution and recommend a deeper assessment into these associations in a larger study population of participants without health insurance.
6 New contribution to the literature
Our study underscores the importance of incorporating an SDOH needs assessment as part of standard clinical practice, especially within clinics serving vulnerable patient populations, such as those without insurance. The intricate interplay between food security associated SDOH needs, and chronic medical conditions, especially with respect to younger individuals, revealed by our study highlights the necessity of adopting a comprehensive, multi-faceted approach to patient care. This data provides valuable context to plan interventions such as food distribution campaigns or other financial SDOH interventions tailored for uninsured populations. Healthcare providers caring for patients with food insecurity should also consider the mental health implications, as our study found these individuals to be more susceptible to anxiety and depression diagnoses or symptoms. Follow-up studies on SDOH needs, health outcomes, and resource usefulness would provide valuable insights into food insecurity trends over time for individuals without health insurance and inform the development of robust interventions.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
FAO I, UNICEF WFP, WHO. The state of food security and nutrition in the world 2022: repurposing food and agricultural policies to make healthy diets more affordable. 2022.
Definitions of Food Security. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-u-s/definitions-of-food-security/. Accessed 15 May 2024.
Gundersen C, Ziliak JP. Food insecurity and health outcomes. Health Aff. 2015;34:1830–9. https://doi.org/10.1377/hlthaff.2015.0645.
Walker RJ, Garacci E, Dawson AZ, Williams JS, Ozieh M, Egede LE. Trends in food insecurity in the United States from 2011–2017: disparities by age, sex, race/ethnicity, and income. Popul Health Manag. 2021;24:496–501. https://doi.org/10.1089/pop.2020.0123.
Kamimura A, Jess A, Trinh HN, Aguilera G, Nourian MM, Assasnik N, Ashby J. Food insecurity associated with self-efficacy and acculturation. Popul Health Manag. 2017;20:66–73. https://doi.org/10.1089/pop.2015.0179.
Berkowitz SA, Seligman HK, Choudhry NK. Treat or eat: food insecurity, cost-related medication underuse, and unmet needs. Am J Med. 2014;127(303–310): e303. https://doi.org/10.1016/j.amjmed.2014.01.002.
Giannoni M, Grignon M. Food insecurity, home ownership and income-related equity in dental care use and access: the case of Canada. BMC Public Health. 2022;22:497. https://doi.org/10.1186/s12889-022-12760-6.
Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med. 2006;21:71–7. https://doi.org/10.1111/j.1525-1497.2005.00278.x.
Mendy VL, Vargas R, Cannon-Smith G, Payton M, Enkhmaa B, Zhang L. Food insecurity and cardiovascular disease risk factors among Mississippi adults. Int J Environ Res Public Health. 2018. https://doi.org/10.3390/ijerph15092016.
Walker RJ, Garacci E, Ozieh M, Egede LE. Food insecurity and glycemic control in individuals with diagnosed and undiagnosed diabetes in the United States. Prim Care Diabetes. 2021;15:813–8. https://doi.org/10.1016/j.pcd.2021.05.003.
Banerjee T, Crews DC, Wesson DE, Dharmarajan S, Saran R, Rios Burrows N, Saydah S, Powe NR. Food insecurity, CKD, and subsequent ESRD in US adults. Am J Kidney Dis. 2017;70:38–47. https://doi.org/10.1053/j.ajkd.2016.10.035.
Food Security and Nutrition Assistance. https://www.ers.usda.gov/data-products/ag-and-food-statistics-charting-the-essentials/food-security-and-nutrition-assistance/#:~:text=In%202020%2C%2089.5%20percent%20of,from%2010.5%20percent%20in%202019. Accessed 15 May 2024.
Lauren BN, Silver ER, Faye AS, Rogers AM, Woo-Baidal JA, Ozanne EM, Hur C. Predictors of households at risk for food insecurity in the United States during the COVID-19 pandemic. Public Health Nutr. 2021;24:3929–36. https://doi.org/10.1017/S1368980021000355.
Niles MT, Beavers AW, Clay LA, Dougan MM, Pignotti GA, Rogus S, Savoie-Roskos MR, Schattman RE, Zack RM, Acciai F, et al. A multi-site analysis of the prevalence of food insecurity in the United States, before and during the COVID-19 Pandemic. Curr Dev Nutr. 2021. https://doi.org/10.1093/cdn/nzab135.
Berkowitz SA, Seligman HK, Rigdon J, Meigs JB, Basu S. Supplemental nutrition assistance program (SNAP) participation and health care expenditures among low-income adults. JAMA Intern Med. 2017;177:1642–9. https://doi.org/10.1001/jamainternmed.2017.4841.
Keith-Jennings B, Llobrera J, Dean S. Links of the supplemental nutrition assistance program with food insecurity, poverty, and health: evidence and potential. Am J Public Health. 2019;109:1636–40. https://doi.org/10.2105/AJPH.2019.305325.
Murimi MW, Kanyi MG, Mupfudze T, Mbogori TN, Amin MR. Prevalence of food insecurity in low-income neighborhoods in west texas. J Nutr Educ Behav. 2016;48(625–630): e621. https://doi.org/10.1016/j.jneb.2016.07.003.
Hunt BR, Benjamins MR, Khan S, Hirschtick JL. Predictors of food insecurity in selected Chicago community areas. J Nutr Educ Behav. 2019;51:287–99. https://doi.org/10.1016/j.jneb.2018.08.005.
Smith S, Malinak D, Chang J, Perez M, Perez S, Settlecowski E, Rodriggs T, Hsu M, Abrew A, Aedo S. Implementation of a food insecurity screening and referral program in student-run free clinics in San Diego. California Prev Med Rep. 2017;5:134–9. https://doi.org/10.1016/j.pmedr.2016.12.007.
Daniel H, Bornstein SS, Kane GC, Carney JK, Gantzer HE, Henry TL, Lenchus JD, Li JM, et al. Addressing social determinants to improve patient care and promote health equity: an American college of physicians position paper. Ann Intern Med. 2018. https://doi.org/10.7326/M17-2441.
Sonik RA. Health insurance and food insecurity: sparking a potential virtuous cycle. Am J Public Health. 2019;109:1163–5. https://doi.org/10.2105/AJPH.2019.305252.
Knight CK, Probst JC, Liese AD, Sercye E, Jones SJ. Household food insecurity and medication “scrimping” among US adults with diabetes. Prev Med. 2016;83:41–5. https://doi.org/10.1016/j.ypmed.2015.11.031.
Heerman WJ, Wallston KA, Osborn CY, Bian A, Schlundt DG, Barto SD, Rothman RL. Food insecurity is associated with diabetes self-care behaviours and glycaemic control. Diabet Med. 2016;33:844–50. https://doi.org/10.1111/dme.12896.
Moen M, Storr C, German D, Friedmann E, Johantgen M. A review of tools to screen for social determinants of health in the United States: a practice brief. Popul Health Manag. 2020;23:422–9. https://doi.org/10.1089/pop.2019.0158.
Social Determinants of Health: guide to social needs screening. American Academy of Family Physicians 2019.
Blumberg SJ, Bialostosky K, Hamilton WL, Briefel RR. The effectiveness of a short form of the household food security scale. Am J Public Health. 1999;89:1231–4. https://doi.org/10.2105/ajph.89.8.1231.
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. https://doi.org/10.1016/j.jbi.2019.103208.
Wells BJ, Chagin KM, Nowacki AS, Kattan MW. Strategies for handling missing data in electronic health record derived data. EGEMS. 2013;1:1035. https://doi.org/10.13063/2327-9214.1035.
Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in obesity among adults in the United States, 2005 to 2014. JAMA. 2016;315:2284–91. https://doi.org/10.1001/jama.2016.6458.
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, Ramirez A, Schlaich M, Stergiou GS, Tomaszewski M, et al. 2020 international society of hypertension global hypertension practice guidelines. Hypertension. 2020;75:1334–57. https://doi.org/10.1161/HYPERTENSIONAHA.120.15026.
American Diabetes A. 2 Classification and diagnosis of diabetes: standards of medical care in diabetes-2020. Diabetes Care. 2020;43:S14–31. https://doi.org/10.2337/dc20-S002.
Jacobson TA, Maki KC, Orringer CE, Jones PH, Kris-Etherton P, Sikand G, La Forge R, Daniels SR, Wilson DP, Morris PB, et al. National lipid association recommendations for patient-centered management of dyslipidemia: part 2. J Clin Lipidol. 2015;9(S1–122): e121. https://doi.org/10.1016/j.jacl.2015.09.002.
Chen TK, Knicely DH, Grams ME. Chronic kidney disease diagnosis and management: a review. JAMA. 2019;322:1294–304. https://doi.org/10.1001/jama.2019.14745.
Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–7. https://doi.org/10.1001/archinte.166.10.1092.
Gilbody S, Richards D, Brealey S, Hewitt C. Screening for depression in medical settings with the patient health questionnaire (PHQ): a diagnostic meta-analysis. J Gen Intern Med. 2007;22:1596–602. https://doi.org/10.1007/s11606-007-0333-y.
Hamilton WL, Cook JT, ThompsonWW, Buron LF, Frongillo Jr, EA, Olson CM, Wehler CA. 1997 Household Food Security in the United States in 1995: Summary Report of the Food Security Measurement Project; United States Department of Agriculture.
Sjoberg DD, Whiting K, Curry M, Lavery JA, Larmarange J. Reproducible summary tables with the gtsummary package. R J. 2021;13:570–80. https://doi.org/10.32614/RJ-2021-053.
Venables WN, Ripley BD. Modern applied statistics with S. New York: Springer; 2002.
Banks AR, Bell BA, Ngendahimana D, Embaye M, Freedman DA, Chisolm DJ. Identification of factors related to food insecurity and the implications for social determinants of health screenings. BMC Public Health. 2021;21:1410. https://doi.org/10.1186/s12889-021-11465-6.
Seo BK, Park GR. Food insecurity and housing affordability among low-income families: does housing assistance reduce food insecurity? Public Health Nutr. 2021;24:4339–45. https://doi.org/10.1017/S1368980021001002.
Dean EB, French MT, Mortensen K. Food insecurity, health care utilization, and health care expenditures. Health Serv Res. 2020;55(Suppl 2):883–93. https://doi.org/10.1111/1475-6773.13283.
Cai J, Bidulescu A. The association between food insecurity and cognitive impairment among the US adults: The mediation role of anxiety or depression. J Affect Disord. 2023;325:73–82. https://doi.org/10.1016/j.jad.2022.12.071.
Pryor S, Dietz W. The COVID-19, obesity, and food insecurity syndemic. Curr Obes Rep. 2022. https://doi.org/10.1007/s13679-021-00462-w.
U.S. Bureau of Labor Statistics. 2022 Consumer Price Index, Midwest Region—April 2022.
Shin JI, Bautista LE, Walsh MC, Malecki KC, Nieto FJ. Food insecurity and dyslipidemia in a representative population-based sample in the US. Prev Med. 2015;77:186–90. https://doi.org/10.1016/j.ypmed.2015.05.009.
Casagrande SS, Bullard KM, Siegel KR, Lawrence JM. Food insecurity, diet quality, and suboptimal diabetes management among US adults with diabetes. BMJ Open Diabetes Res Care. 2022. https://doi.org/10.1136/bmjdrc-2022-003033.
Ghazaryan A, Carlson A, Rhone AY, Roy K. Association between the nutritional quality of household at-home food purchases and chronic diseases and risk factors in the United States, 2015. Nutrients. 2021. https://doi.org/10.3390/nu13093260.
America, F. Map the Meal Gap: How We Got the Map Data. https://www.feedingamerica.org/research/map-the-meal-gap/how-we-got-the-map-data. Accessed 2024.
Bickel G, Nord M, Price C, Hamilton W, Cook J. 2000 Guide to measuring household food security.
Acknowledgements
We would like to thank and acknowledge Jeff Fritz, Ph.D., MS, MATL, and Malika Siker, MD for their review of this manuscript. We extend our gratitude to the patients and healthcare providers of the Saturday Clinic for the Uninsured (SCU) in Milwaukee, Wisconsin for their participation and feedback. We are also grateful to many of the clinic volunteers that made this project possible, including Nicole Runkle, MD, Ashley Pohlman, MD, Erica Engstrand, Donglin Zhang, Madeline Zamzow, Owen Bowie, Anna Lyons, Delaney Weiland, Shivani Kumar, Nathan Luzum, and Jennifer Terrell. We received permission to acknowledge those named in this section.
Funding
This work received support from the Medical College of Wisconsin Departments of Community Engagement, Family and Community Medicine, and Robert D. and Patricia E. Kern Institute for the Transformation of Medical Education. S.K.T. is a member of the Medical Scientist Training Program at MCW, which is partially supported by a training grant from the National Institute of General Medical Sciences, T32-GM080202.
Author information
Authors and Affiliations
Contributions
Conceptualization: Suma Thareja, Spenser Marting, Benjamin Liu, Thomas Ritter, Rebecca Lundh, and Staci Young; Methodology: Suma Thareja, Spenser Marting, William Davies, Benjamin Liu, Thomas Ritter, Jessica Miller, and Rebecca Lundh; Formal analysis and investigation: Suma Thareja, Spenser Marting, William Davies, Santhosi Samudrala, Ramsey Rayes, Marie Balfour, Ana Mia Corujo-Ramirez, Frances Carter, Benjamin Liu, Dylan Trinh, and Thomas Ritter; Writing—original draft preparation: Spenser Marting, William Davies, Santhosi Samudrala, Ramsey Rayes, Marie Balfour, Ana Mia Corujo-Ramirez, Frances Carter, and Coleman Fine; Writing—review and editing: Suma Thareja, Benjamin Liu, Dylan Trinh, Thomas Ritter, Jessica Miller, Coleman Fine, Rebecca Lundh, and Staci Young; Funding acquisition: Rebecca Lundh, and Staci Young; Resources: William Davies, Frances Carter, Dylan Trinh, Rebecca Lundh, and Staci Young; Supervision: Rebecca Lundh and Staci Young.
Corresponding author
Ethics declarations
Ethics approval and content to participate
This research has been approved and granted exempt status by the Institutional Review Board (IRB) at the Medical College of Wisconsin (PRO00028616). The study uses social determinants of health (SDOH) data, which are routinely collected as part of the standard clinic workflow. Additionally, a retrospective chart review was performed to examine patients' chronic medical conditions. Prior to completing the SDOH survey, patients provided verbal informed consent, which is the standard procedure in the clinic. All data collected for this study have been handled with strict confidentiality and in accordance with the guidelines set forth by the IRB and the US Federal Regulations for the Protection of Human Subjects. Any identifying information has been removed to ensure the privacy and anonymity of the participants.
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Thareja, S.K., Marting, S., Davies, W. et al. Associated SDOH needs of patients without health insurance and experiencing food insecurity. Discov Soc Sci Health 4, 25 (2024). https://doi.org/10.1007/s44155-024-00084-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44155-024-00084-2