Abstract
Due to social distancing policies and concerns over patient and provider safety, early in the COVID-19 pandemic many healthcare institutions temporarily converted to various, non-traditional rounding models. The abrupt and unprecedented change in workflow has enabled re-assessment of the reasons for the traditional rounding structures in medical education and comparison to newer strategies for rounding which have developed out of necessity during the pandemic. In this Perspectives article, we examine the positive and negative aspects of rounding models borne out of the pandemic and suggest aspects which may be carried forward, as well as future directions for research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Review and discussion
In a traditional “bedside rounding” model in medical education, the junior team members (first year residents and students) will see patients independently, perform examinations and conduct histories, and then formulate a plan of care [1]. Their findings on these “pre-rounds” as well as their tentative plan as to next steps in patient care would then be discussed with the service (medical students, other residents, an attending and other members of the interdisciplinary team) as a whole at bedside. The team would then examine and interview the patient as well as formulate a final plan for next steps in patient care. While in the patient room additional history could be gleaned by the team, bedside teaching would take place, the patient’s bedside chart would be reviewed (if present), and orders or recommendations may be entered into the chart at bedside (if present or urgent). Despite this comprehensive and time honored approach, bedside rounds have been demonstrated to have a limited effect on patient centered outcomes, and time spent at bedside has not correlated with patient agreement in care or patient experience ratings [2, 3]. “Walk rounds” are similar to bedside rounds but with presentations/clinical decisions typically happening outside the patient’s room, followed by a brief group encounter with the patient [1]. Although rounds in some instances may make up much of the day, the simplified outline above belies a much more complex workday with competing responsibilities [4].
In the modern era where electronic medical records are the default charting system in the United States, visiting the patient’s bedside strictly for the purposes of chart review, placing orders or relaying recommendations to a primary service or nurse is no longer necessary (as electronic communication, such as through the EMR, pager, or phone may expediently handle these tasks). The change from charting at bedside to reliance on EMR has been an enormous sea change in Medicine over the past three decades. Although learning a new program may be difficult and has led to more time in front of the computer as opposed to with the patient, EMR use has been associated with reduced mortality, readmissions and other metrics of clinical quality [5, 6]. Despite changes in how and where care is ordered and documented, the traditional group bedside and walk rounding model in medical education, previously based around bedside charting and group evaluation and teaching, has persisted. That is, until the recent pandemic began.
At the emergence of COVID-19 in the United States, there were no effective proven therapies, no effective proven vaccines, there were personal protective equipment (PPE) shortages and debates about the modes of transmission and best practices for infection control in relation to suspected and documented cases of this novel coronavirus. To prevent nosocomial spread of SARS-CoV-2 to other patients and health care providers we relied exclusively on non-pharmacologic interventions, which included universal masking and social distancing. As part of social distancing, it was not uncommon to see new limitations on maximum occupancy of workspaces, elevators, or other venues in the hospital, which may impact the size of a physical rounding team [7].
The degree to which social distancing impacted rounding of primary and consultative inpatient services varied inter-institutionally as well as within services within organizations. Innovative strategies to round on inpatients included patient-remote rounding (communication with patients via video or phone only) [8], or pre-rounding physically on patients by different team members but discussing their care in a virtual videoconference (sometimes inclusive of family) [9]. Locally, our children’s hospital developed a hybrid, provider-limited, rounding model with synchronous in-person and virtual participation [10]. Mixed teams of in-person and virtual providers (used preferentially for COVID patients) proliferated elsewhere [11]. Recent years additionally have seen the rise of videoconference robots remotely controlled by medical teams to provide patient care synchronously. This methodology has actually been found to increase team communication without negative impacts on dynamics such as team trust, role responsibilities or morale [12]. A study of virtual rounding by videoconference robot compared to standard in-person rounds resulted in similar length of stay, morbidity and patient satisfaction among post-operative patients [13].
The learner-provider group most likely impacted by strict hospital social distancing rules were medical students, who, in many cases, saw their clinical rotations, the lifeblood of their final years of medical school, go from in-person to, in some cases, exclusively remote and virtual [14]. Incorporation of remote students led to innovations in videoconferencing students into surgeries, table rounds and even bedside rounding with the on-service attending [15,16,17,18,19]. When assessed in the aforementioned studies, students did review their virtual courses highly, possibly due to convenience and reduced cost and wanting to appear eager on evaluations; however, medical students still need, at a minimum, training in physical examination skills, history taking, building relationships with patients and the interdisciplinary team—practices which are not readily developed remotely.
But what of house staff and attendings? One take away from the pandemic has been the success of asynchronous rounding (which we will define as different team members seeing the patient independently, and then discussing together via videoconference or at in-person table rounds (also called “card flipping”) [9]. While this is not an entirely novel concept unique to the pandemic, utilization of this approach likely increased when inpatient teams were confronted with social distancing issues.
With many hospital systems expanding in the face of a predominantly unchanged number of graduate medical education positions [20], inpatient censuses relative to number of house staff may be expanding and improved rounding efficiency may be one way to deal with increased volumes. Avoiding whole-team bedside or walk rounds by utilizing an asynchronous rounding structure may increase the efficiency of the group in that multiple team members will not need to travel to the same patient rooms multiple times in one day. As many large medical centers occupy multiple buildings and floors, the travel time between patient rooms on a team’s census may be profound unless there has been intentional geographic cohorting (although for many consultants, this will never be the case) [1]. Team members may find that seeing the patient separately from one another could also be more efficient in shorter interview and exam times, as only one person instead of multiple would be in communication with a patient at a time, and it may be quicker for fewer providers to don/doff protective equipment before entering or leaving a patient room with a smaller rounding team. The efficiency gained by limiting certain providers (residents or fellows) from group walking or bedside rounds may result in the ability to more expediently place orders, call consults, relay recommendations and schedule exams or procedures. In fact, when surveyed, about half of hospitalists preferred seeing patients independent of a team [21]. The time saved on whole group bedside rounding may improve the timeliness of patient care, an important consideration for patients’ quality of life on the wards, as well as their safety and comfort (consider if an endoscopy is not ordered until the end of a multiple hour walk-round session delaying a procedure until the next day, or if a patient is waiting for an order of pain medication while a medical team is traversing multiple buildings seeing patients in person). Sleep is also notoriously difficult for patients in the hospital (due to vitals, alarms, labs, exams, among other issues), and it is possible that being seen by smaller teams may lead to fewer disruptions in rest [22].
During COVID, a model where a Vascular Surgery rounding complement was reduced to 1–3 providers physically present in a patient’s room, with the remainder of the team available via call, was actually rated highly by providers and patients [23]. Glasglow et. al noted upon survey the providers felt rounding with a smaller team was more efficient and conserved PPE during the shortages associated with COVID-19. Patients in this study also preferred fewer providers being physically present at once in the room and thought an adequate level of care was maintained. In an era of incentivization of discharges early in the day as well as minimization of length of stay, any method which may contribute to higher efficiency of care would surely be welcomed [24]. As some patients experience anxiety over the size of the team visiting them, a slimmer rounding team would likely be less intimidating for some inpatients [1]. Patients may additionally benefit from asynchronous rounding in that multiple providers from the same team are seeing them at varying time points in the day, which allows for sequential assessment of clinical status and symptoms, which is missing from a classical rounding structure of seeing the patient twice in the morning (pre-rounds at 7:30am, attending rounds at 9am, for example). A study of asynchronous multi-disciplinary rounds on ICU patients found that this strategy was non-inferior for ICU bundle compliance and was associated with reduced ventilator days, denoting clinical efficacy of this type of model [25]. Apart from the above potential benefits to the patient, different rounding strategies should also consider the wellness of team members and how it is impacted by the amount of time spent at work. There is a logical and demonstrable negative association between happiness and hours worked [26], and more efficient rounding structures may help to allay that. All members of the interdisciplinary medical team may have various family responsibilities, research and administrative roles in addition to patient care responsibilities—and these roles may be encroached upon by time spent on prolonged, inefficient bedside or walk rounding.
On the contrary, utilization of an asynchronous rounding strategy beyond the current pandemic could have downsides as well. While medical students likely derive the most benefit from in-person rounding with an expert clinician, there are benefits to residents and fellows as well. However, as senior house staff trainees have already passed competency benchmarks by their admission to residency and fellowship, the magnitude of the experience gained from being in the room with an attending and patient simultaneously is likely diminished in comparison with early students. For the express purposes of education, it should be perfectly acceptable and even reinforced to have a whole medical team simultaneously see a patient with an unusual finding, an incomplete exam or history or a clinical pearl which can only be demonstrated in person. However, in the instances where the patient-medical team interaction solely involves telling the patient the plan, introducing a team member or asking if the patient has questions about their care, there are no obvious large benefits to many learners in exchange for the “ask” of spending hours walking throughout the hospital as a group to see patients (who they have already seen at least once during the day). When there is minimal interaction between a patient and a team leader, or minimal additional teaching during this time spent on walk or bedside rounds, the “contract” of formal group bedside or walk rounding is being broken at the potential consequences of added time to the clinical day, less efficient care and increased vulnerability to burnout. Medical trainees and academic leaders agree that one of the central purposes of rounds is education; however, this aspect is progressively fading from team walking or bedside rounds, which has been attributed to time constraints, among other factors [27]. If group bedside or walk rounding is not logistically feasible for all patients, then selective bedside rounding on a particular few patients where there is educational and/or clinical benefit from being seen as a team would be appropriate; however, for the remainder of the census asynchronous rounding could be performed and perhaps provide more expedient care. Notably, trainees at geographically distinct institutions have positively reviewed an asynchronous rounding model [28]. That being said, we do still place a high value on the medical student, if present, being able to see all patients with more senior clinicians for educational benefit.
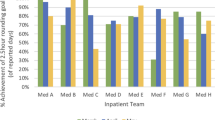
Some critiques of a partial or total asynchronous rounding model may be that it would require increased communication between team members as decisions about care would not be relayed to one another at bedside [1]; however, table rounding/card flipping would create space for shared decision making amongst team members while electronic communication can facilitate any changes to care which may need to be made at other times during the day. Additionally, team bedside or walk rounding may serve additional functions from patient care and education, opening opportunities for career development or research through informal conversations in between patient rooms. It may also serve to build relationships between team members, but there are other avenues for fostering this type of collaboration as well. Certain patients may also prefer to have teams just visit simultaneously to avoid confusion about their care plan or roles on the team [1, 29], but as mentioned above a slimmer rounding team has also previously been positively reviewed by most patients in one study—and may be less frightening or overwhelming to some. Figures 1 and 2 compare risks and benefits of rounding models to health care providers and patients in summary form.
2 Conclusion
We recognize fully that many opinions expressed here are simply that, as there have not been many formal studies of traditional team based synchronous rounding compared to asynchronous rounding models (selecting a few patients to see altogether or having various team members visit patients separately from one another). As a potential beneficial contribution to quality (timeliness) of care, clinical efficacy and provider well-being, comparative studies should be done to determine the real-world implications of this newer asynchronous rounding model compared to traditional team-based rounds. Studies of other rounding interventions on patient reported outcomes, clinical efficiency and provider preferences have previously been conducted, so these questions are practically able to be studied [29]. While additional evaluation of asynchronous rounding is ongoing, for teams or services which are particularly challenged by large clinical volumes, covering large geographic areas within medical centers, clinical efficiency or health care worker wellness, these novel asynchronous rounding structures may represent a viable trial option which can be utilized at any health care center with collaborative care teams.
References
Ricotta DN, Freed JA, Hale AJ. Things We Do for No Reason™: Card Flipping Rounds. J Hosp Med. 2020 Aug;15(8):498–501. https://doi.org/10.12788/jhm.3374
Ratelle JT, Sawatsky AP, Kashiwagi DT, Schouten WM, Erwin PJ, Gonzalo JD, et al. Implementing bedside rounds to improve patient-centred outcomes: a systematic review. BMJ Qual Saf. 2019;28:317–26.
Ratelle JT, Herberts M, Miller D, Kumbamu A, Lawson D, Polley E, et al. Relationships between time-at-bedside during hospital ward rounds, clinician-patient agreement, and patient experience. J Patient Exp. 2021. https://doi.org/10.1177/23743735211008303.
Malhotra S, Jordan D, Shortliffe E, Patel VL. Workflow modeling in critical care: piecing together your own puzzle. J Biomed Inform. 2007;40:81–92.
Lin HL, Wu DC, Cheng SM, Chen CJ, Wang MC, Cheng CA. Association between electronic medical records and healthcare quality. Medicine (United States). 2020. https://doi.org/10.1097/MD.0000000000021182.
Do electronic medical records improve quality of care? YES-Donna P. Manca MD MClSc FCFP NO-Michelle Greiver MSc MD CCFP FCFP. www.cfp.ca.
Donnon T, Lee M, Cairncross S. Using item analysis to assess objectively the quality of the Calgary-Cambridge OSCE Checklist. Can Med Educ J. 2011;2(1):16–22. https://doi.org/10.36834/cmej.36556.
Renner A, Paajanen J, Reijula J. Tele-rounding in a university hospital pulmonary ward during the COVID-19 pandemic: a pilot study. Infect Dis. 2020;52:669–70. https://doi.org/10.1080/2374423520201776382.
Wang H, Poehler JL, Ziegler JL, Weiler CC, Khan SA. Patient care rounds in the intensive care unit during COVID-19. Jt Comm J Qual Patient Saf. 2020;46:600.
Orlov NM, Mattson C, Kraft A, Wagner E, Mallick S, Cunningham P, Arora VM. LEAPFROG Rounds: Maximizing the Rounding Experience for the Interprofessional Team During the COVID-19 Pandemic. Acad Pediatr. 2021 Jul;21(5):917–919. https://doi.org/10.1016/j.acap.2021.04.008
Becker NV, Hirner JP, Bakshi S. Provider experience and satisfaction with a novel “virtual team rounding” program during the COVID-19 pandemic header: “Virtual team rounding.” https://academic.oup.com/intqhc/advance-article/doi/https://doi.org/10.1093/intqhc/mzab111/6332352. Accessed 10 Aug 2021.
Lazzara EH, Benishek LE, Patzer B, Gregory ME, Hughes AM, Heyne K, et al. Utilizing telemedicine in the trauma intensive care unit: does it impact teamwork? Telemed e-Health. 2015;21:670–6.
Ellison LM, Nguyen M, Fabrizio MD, Soh A, Permpongkosol S, Kavoussi LR. Postoperative robotic telerounding a multicenter randomized assessment of patient outcomes and satisfaction. Arch Surg. 2007. https://doi.org/10.1001/archsurg.142.12.1177.
Asaad M, Glassman GE, Allam O. Virtual rotations during COVID-19: an opportunity for enhancing diversity. J Surg Res. 2021;260:516–9.
Hofmann H, Harding C, Youm J, Wiechmann W. Virtual bedside teaching rounds with patients with COVID-19. Med Educ. 2020;54:959–60.
Sandhu N, Frank J, von Eyben R, Miller J, Obeid J-P, Kastelowitz N, et al. Virtual radiation oncology clerkship during the COVID-19 pandemic and beyond. Int J Radiat Oncol Biol Phys. 2020;108:444.
Pennell CE, Kluckow H, Chen SQ, Wisely KM, Walker BL. Live-streamed ward rounds: a tool for clinical teaching during the COVID-19 pandemic. Med J Aust. 2020;213:306-308.e1. https://doi.org/10.5694/mja2.50765.
Sukumar S, Zakaria A, Lai CJ, Sakumoto M, Khanna R, Choi N. Designing and implementing a novel virtual rounds curriculum for medical students’ internal medicine clerkship during the COVID-19 pandemic. MedEdPORTAL. 2021;17:11106.
Bala L, Kinross J, Martin G, Koizia LJ, Kooner AS, Shimshon GJ, et al. A remote access mixed reality teaching ward round. Clin Teach. 2021;18:386–90. https://doi.org/10.1111/tct.13338.
Boyle P. Medical school enrollments grow, but residency slots haven’t kept pace. AAMC. 2019. Available from: https://www.aamc.org/news-insights/medical-school-enrollments-grow-residency-slots-haven-t-kept-pace
Mirabella AC, McAmis NE, Kiassat C, Feinn R, Singh G. Preferences to improve rounding efficiency amongst hospitalists: a survey analysis. J Community Hosp Intern Med Perspect. 2021;11:501–6.
Kulpatcharapong S, Chewcharat P, Ruxrungtham K, Gonlachanvit S, Patcharatrakul T, Chaitusaney B, et al. Sleep quality of hospitalized patients, contributing factors, and prevalence of associated disorders. Sleep Disord. 2020;2020:1–7.
Glasgow S, Saha P, Moore H, James B, Newsholme W, Zayed H. Perception and acceptability of virtual ward round reviews of vascular inpatients to preserve resources and reduce infection risk in the COVID-19 era. Eur J Vasc Endovasc Surg. 2021;61:527.
Lichstein PR, Atkinson HH. Patient-centered bedside rounds and the clinical examination. Med Clin N Am. 2018;102:509–19. https://doi.org/10.1016/j.mcna.2017.12.012.
O'Leary Martland AM (2023). Evaluation of a novel hybrid approach to multidisciplinary rounds to improve intensive care unit liberation bundle compliance [Doctoral dissertation, Georgetown University]. http://hdl.handle.net/10822/1082669
Virtanen M, Stansfeld SA, Fuhrer R, Ferrie JE, Kivimäki M. Overtime work as a predictor of major depressive episode: a 5-year follow-up of the whitehall ii study. PLoS ONE. 2012;7:1–5.
Hulland O, Farnan J, Rabinowitz R, Kearns L, Long M, Monash B, Bhansali P, Fromme HB. What's the Purpose of Rounds? A Qualitative Study Examining the Perceptions of Faculty and Students. J Hosp Med. 2017 Nov;12(11):892–897. https://doi.org/10.12788/jhm.2835
Savage DJ. The COVID-19 pandemic as a catalyst for medical education innovation: a learner’s perspective. FASEB Bioadv. 2021;3:449.
Gonzalo JD, Chuang CH, Huang G, Smith C. The return of bedside rounds: an educational intervention. J Gen Intern Med. 2010;25:792–800.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
The authors have both made substantial contributions to the development, writing and revising of the above article. Conceptualization: MC, CL; Formal Analysis and Investigation: MC; Supervision: MC; Writing—Original Draft Preparation: MC; Writing—Review and Editing: CL.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This opinion piece supported by citations is not human subjects research and therefore IRB approval was not sought.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Czapka, M., Lehmann, C. Pandemic insights: what COVID-19 has revealed about traditional rounding structure. Discov Soc Sci Health 3, 24 (2023). https://doi.org/10.1007/s44155-023-00054-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44155-023-00054-0