Abstract
Background
Tobacco smoking still represents one of the most significant preventable causes of death and poor health, and higher success rates for people trying to quit smoking would benefit both public and individual health. Achieving this requires better knowledge of factors that might improve the chances of successful quitting. This study aims to investigate cessation activities and explore associations between outcomes of smoking cessation attempts and use of cessation aids, previous cessation attempts, and attempt-planning.
Methods
Using data from a national web panel (N = 1424), smoking cessation activities and use of smoking cessation aids by people who smoke or have smoked are studied bivariately and in adjusted models.
Results
Almost half the sample had not used a cessation aid in the last quit attempt. Snus was the most common cessation aid, followed by NRTs and ECs. In adjusted models, snus use increased the likelihood of quitting. Planning an attempt and earlier quit attempts were associated with less quitting.
Conclusion
Presently, switching to snus seems to be the most effective and efficacious method for quitting smoking in Norway.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Background
Cigarette smoking represents one of the most significant preventable causes of death and poor health globally [1], improved knowledge of factors that could increase smoking cessation rates is both relevant and essential, and would clearly benefit public and individual health. In Norway, after decades of increasingly strict anti-tobacco regulations, 14% of adults still smoke [2]. An important reason for this is that quitting is challenging for people with an established smoking habit. Results from international studies suggest that while 40% of people who smoke try to quit in a given year [3], only around 1 in 3 of these attempters manage to renounce cigarettes [4]. Additionally, there tends to be large variation in success rates depending on the methods used in the cessation attempt [4, 5].
Smoking cessation aids, i.e., products people use for the purpose of quitting smoking [6], can loosely be divided into the three sub-groups counselling, medicinal drugs, and alternative tobacco and nicotine sources. The counselling group includes face-to-face advice from health personnel, smoking cessation courses, self-help books, and various digital resources and quit lines. A relatively new addition to this group of aids in Norway is a mobile app called “slutta” (“Quitting”). Such mobile smartphone-based smoking cessation interventions have been developed in many countries, but their contents might differ substantially [7]. The Norwegian mobile app offers daily motivational messages, quitting advice, and facts on the health risks of smoking, in addition to the tracking of abstinence period (Norwegian Directorate of Health). Prescription drugs, e.g., varenicline and bupropion, and nicotine replacement therapies (NRTs) lies within the class of medicinal drugs. In Norway, NRTs do not require a prescription, and are available in pharmacies and grocery stores for everyone over the legal age [18 years]. Within the class of alternative nicotine and tobacco sources lies products that are used as smoking cessation aids, despite not being licensed or approved by health authorities. Generally, these products are less harmful to use than combustible tobacco [8, 9]. In the Norwegian context, two alternative tobacco and nicotine sources are currently available, namely Swedish moist snuff (snus) and e-cigarettes (ECs).
Snus is an established product that has been on the Norwegian market for several decades. In 2021, the prevalence for all current snus use was 25% of men and 10% of women [10]. The public health consequences of the availability of snus is a topic for considerable debate, and while there is general concern for snus use among adolescents [11] studies have also argued that it may have led to a sharper decline in smoking both in Norway [12] and in neighbouring country Sweden [13].
ECs has been available in Norway for approximately a decade and are thus a much more recent addition to our nicotine market. Domestic shops are only allowed to sell EC devices and non-nicotine e-liquids, while nicotine-containing e-liquids must be bought from abroad, usually from online shops. Despite this obstacle, there are currently around 150.000 EC users in Norway [14], with the vast majority of them being people who smoke or have smoked [15]. A recent study did not find any association between the use of ECs and smoking cessation in Norway [7], but internationally a recent Cochrane review found moderate‐certainty evidence that ECs with nicotine increased quit rates compared to NRTs and compared to ECs without nicotine [16].
Despite the relatively large supply of various cessation aids, current information suggests that a high proportion of quit attempts are unassisted in Norway [7] and internationally [17,18,19,20,21,22]. Studies indicate that chances for smoking abstinence might increase if smoking cessation aids are used [23], although the evidence is not necessarily very solid. Under ideal conditions, i.e. with support from the health care system, positive effects of NRTs and prescription drugs are reported in some reviews [24, 25] but disputed in others [26]. In real-life situations, the evidence is even less robust, and concerns for the real-world effectiveness of smoking cessation interventions have been expressed both in a systematic review [27] and in recent single studies [18, 28].
In addition to the use of cessation aids, research has pointed to other factors that might influence the probability of successful quitting. Spontaneous quit attempts have, in some studies, been found to be more successful than planned quit attempts [29, 30]. Furthermore, some quit attempts involve a gradual reduction in daily cigarettes, but findings are inconclusive regarding the effect of this strategy. One review study found abrupt quitting to give higher quit rates than gradual reduction [31], while another review study found no differences between gradual and abrupt strategies in long-term success rates [32]. Finally, earlier quit attempts have been shown to increase the likelihood of making a subsequent attempt [33]. In terms of individual characteristics, quit rates might vary in age and gender groups [34], self-efficacy has been shown to increase success rates [35], and individual smoking habits (cigarettes per day, nicotine addiction) also tend to influence the probability of quitting [33].
We aimed to (1) investigate cessation activities and outcomes of cessation attempts in individuals that are, or have been, smoking and (2) explore associations between different cessation aids, the number of previous attempts, and attempt-planning and successful quitting.
2 Methods
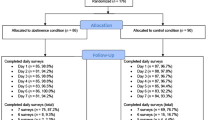
The data stems from a national web panel administered by the commercial pollster Norstat and collected in a web survey by Mindshare Norway, in connection with a 28 day long quit smoking campaign (Stoptober) organized by the Norwegian Directorate for Health in October 2020. Panellists, randomly drawn within age, gender and regional quotas, received an invitation to participate by email, and data collection continued until each quota reached a pre-set number of participants. Only people who smoked or had smoked before were eligible for participation, and participants were rewarded points to save up and eventually exchange for goods.
The data handler Norstat complies with the general data protection requirement (GDPR) and legal guidelines of ESOMAR (European Society for Opinion and Marketing Research). All participants have given their consent to participate and can withdraw this consent and demand their personal information to be deleted at any point in time. For this study, we received only anonymous and non-sensitive/non-health-related data, and the survey was therefore exempt from further ethical approval.
Half the data set was collected prior to, and the other half after, the quit smoking campaign. Individuals who participated in the “before” collection were not invited to participate in the “after” collection. For the purpose of this study, which did not involve any evaluation of the intervention itself, both data collections were merged giving an analytic sample of 1424 individuals who were either currently smoking (N = 1011) or had been smoking before (N = 413).
3 Variables
3.1 Smoking status
Answers to the question “do you smoke cigarettes”, with answer categories “yes daily”, “yes occasionally” and “no I have quit” were transformed to the dummy variable current smoking vs. former smoking. Frequency of smoking was not used in analyses because the data did not contain information on smoking frequency for the former smoking group.
3.2 Cessation aids
All participants were asked to identify the cessation aids they used on their last quit attempt. Fifteen different types of cessation aids were listed, including the option “I did not use a cessation aid”. However, some of the specific aids were used by very few people or even by nobody. For simplicity, these low-prevalent aids, which included the use of health personnel at community health centres or elsewhere, smoking cessation courses, digital resources, chat robots, quit-lines, alternative methods (hypnosis etc.), self-help books, and other unspecified aids, were merged under the label “other aids”. Table 1 gives an overview of cessation aids and their prevalence of use.
3.3 Life-time quit attempts
The participants were themselves free to define their own quit attempts. People who reported to be smoking at the time of the survey were asked, “Have you tried to quit smoking?” People who reported to have quit smoking were asked, “How many times did you try to quit before you managed to quit smoking. In both cases, the response alternatives were “one time”, “2–3 times”, “4–5 times”, “6 times or more”, and “don’t know/don’t want to answer”. Additionally, individuals who were smoking were offered a “no times” alternative.
3.4 Planning to quit
All participants were asked to indicate the amount of planning they did before their last quit attempt using pre-set categories. The categories were operationalized such that “I did not plan the quit attempt, I just quit” was coded as no planning, while all other categories (i.e., “I planned the quit one day/ a couple of days/ a couple of weeks/ a couple of months before”) were coded as any planning. The categories “I don’t know” and “none of the above” were coded as missing.
In addition, the data included information on the participants’ age and gender.
4 Analyses
Bivariate descriptive analyses were used to study the prevalence and distribution of cessation aids and cessation attempts. Multivariate logistic regression was used to investigate associations between cessation aids and cessation attempt outcome, presenting crude odds ratio (OR) and adjusted odds ratio (AOR).
5 Results
As shown in Fig. 1, the majority (56.7%) of the former smoking group needed one attempt to quit smoking, while 35.6% of them needed two or more attempts, and 7.7% did not know. In the smoking group, 23.9% had never tried to quit smoking, 16.2% had made one quit attempt, 52.8% had tried to quit two or more times, while 7.0% did not know.
The average number of quit attempts was 1.57 (N = 381) in the former smoking group. Among those in the smoking group who had made at least 1 attempt, the average number of attempts was 2.24 (n = 698).
Approximately 47% of the sample reported that they did not use any cessation aid on their last quit attempt, and there was no significant difference between the smoking group and the former smoking group in this respect (Table 1). Snus was the most widely used cessation aid and had significantly more often been used in the quit smoking group than in the smoking group (25 vs 13%, p < 0.001). There were also significant differences between the groups in the use of NRTs (16 vs 11%, p < 0.05) and EC (14 vs 9%, p < 0.01), although these differences were in the opposite direction, with the higher prevalence of use among people who still smoked. Prescription drugs were used by 7%, the mobile app by 11%, and any other aids by 11% of the sample, with no significant differences related to current smoking status.
There were significant differences in the choice of cessation aids between men and women and in age groups (Table 2). Men significantly more often reported to have used snus in quitting and quit attempts, while women significantly more often had used the mobile app and other aids. Snus was more than three times, and the mobile app more than twice, as common among people in the 18–34 age group than among older people. In contrast, older people more often did not use any cessation aid and were twice as likely to use NRTs and three times as likely to use prescription drugs.
Plans regarding future quit attempts often involved using the same cessation aid as on previous cessation attempts (Fig. 2). Sixty-one per cent of those who did not use any aid during their last attempt to quit smoking reported this to be their plan also for future attempts. Correspondingly, 71% of those who previously used NRTs, 62% of previous EC users, and 59% of previous snus users planned to use the same aid in future quit attempts. Similar patterns were visible also for the less popular methods, with the proportions of people who wanted to retry the same aid as previously amounting to 40% for prescription drugs, 43% for the mobile app, and 38% for other methods.
The use of cessation aids varied considerably with quit attempt history and the amount of planning involved in the last attempt (Fig. 3). Among those who only had one quit attempt, 60% reported to have used no cessation aid. The corresponding proportion among people with several attempts was 38% (at the last attempt). Similarly, the majority of those who did not plan their last quit attempt (66%) did not use any cessation aid, while this was true for approximately one-third (32%) of those who had done any planning. Approximately 38% of the sample reported to have used one single cessation aid at the last quit attempt, with a higher prevalence among multiple attempters (41%) than single attempter (32%), and among planners (45%) than no-planners (28%). There was also a statistically significant association between planning and more quit-attempts, with 73% of planners reporting more than one attempt vs. 52% of the no-planners (results not reported in figure).
In unadjusted regressions (Table 3), women were less likely to have quit smoking (OR = 0.74, p < 0.05), while the participants age was not significantly associated with quit attempt outcome. Planning quit attempts (OR = 0.50, p < 0.001) and earlier quit attempts (OR = 0.43, p < 0.001) both reduced the odds of quitting. There were no significant associations between the use of prescription drugs, the mobile app or other cessation aids. Using NRTs (OR = 0.64, p < 0.05) and ECs (OR = 0.55, p < 0.01) reduced the likelihood of quitting, while using snus (OR = 2.33, p < 0.001) was associated with more quitting.
When adjusting for all variables simultaneously, snus was the only cessation aid significantly associated with a higher probability of quitting (AOR = 2.64, p < 0.001). Planning the quit attempt (AOR = 0.64, p < 0.01) and to have had earlier quit attempts (AOR = 0.43, p < 0.001) were significantly associated with a lower probability of quitting. Age and gender were not significantly associated with the outcome in the adjusted analysis, and applying alternative age specifications (i.e., groups) did not change these results.
6 Discussion
Approximately ¼ of participants who smoked had never tried to quit. Among all who had tried, almost 50% did not use a cessation aid in their last attempt. Snus was the most common cessation aid, and the only one associated with smoking cessation. People over 35 years were more likely not to have used any cessation aid, while those younger than 35 more often had used snus or the mobile app. Men were more likely to have used snus, and women more likely to have used the mobile app or other aids.
The large proportion of people who did not use a cessation aid in quit smoking attempts, and the predominance of snus, NRTs and ECs among the aids that were used, harmonize with results from a previous Norwegian study [7]. It has been suggested that reasons for not using cessation aids include limited access to smoking cessation support for lower SES individuals [36], or a general disbelief in the effectiveness of smoking cessation aids [37], e.g., due to the idea that the best foundation for successful smoking cessation is personal determination and willpower, and that replacement products like NRTs will not help overcome the psychological dependence [38].
The association found between using snus in quit attempts and successful smoking cessation is in line with earlier Norwegian results supporting an association between experience with snus use and having quit smoking [39, 40], and with previous studies of smoking cessation behaviour from Norway [7] and Sweden [13, 41], the only two countries where snus use is widespread in the population. The demographic segments that use snus for smoking cessation, i.e., men and younger individuals, are the same as the segments where the snus use prevalence is high in general. This might partly be due to different perceptions of the relative risk from snus use and cigarette smoking in these strata [42], and could also suggest that social contagion, comparable to what has been shown for smoking behaviours [43], is making snus more appealing as a cessation aid for individuals who live in an environment where snus is culturally accepted. It is also conceivable that some of the quit attempts are made by snus users who initially had no intention to quit smoking. As with EC users who accidentally quit smoking [44], this effect would likely be contingent on snus’s likeability and reduced harm profile. The effectiveness and high prevalence of snus makes it the cessation aid with the highest efficacy in Norway, i.e., the cessation aid with the highest potential for making a positive contribution to public health [45].
NRT is the nicotine product recommended as a cessation aid by health authorities. However, despite ample marketing and high accessibility, with sales from grocery stores and pharmacies, our study found no association with smoking cessation. Low doses of nicotine have been reported as one of NRTs limitations as a substitute for cigarettes, which becomes clear in real-life setting without any behavioural support [46].
Regarding ECs, a positive effect on smoking cessation has been supported in a Cochrane review [16], but we were not able to find a positive effect on smoking cessation in this study. A contributing factor to this disparity between Norwegian and international results might be that we were unable to separate EC users that use nicotine e-liquids from EC users that use liquids without nicotine. While nicotine liquids are relatively easy to buy from abroad in online shops, the lack of physical availability may represent a barrier that leads some of those who wish to try ECs for smoking cessation to use non-nicotine liquids instead, particularly individuals who erroneously believes that nicotine is the most harmful ingredient in tobacco cigarettes [47]. Such believes could also compel some quit attempters to cut down on the nicotine levels in e-liquids too quickly or too much. One could also speculate that some users struggle with the switching process from combustible to e-cigarettes, as the use of e-cigarettes is more technically demanding [48].
While most of the cessation aids included in this study have been on the market for many years, the mobile app that was made available quite recently. Internationally, smart-phone based smoking cessation interventions shows promise when used in combination with pharmacological treatment [49], and earlier Norwegian research have supported a higher likelihood of smoking cessation for people who use web or mobile solutions as cessation aids [7]. In contrast, no association was found between use of the mobile app and smoking cessation in the current study. Due to its novelty, one might submit that this type of aid has yet to reach its full potential in Norway. Specifically, the Norwegian mobile app is currently primarily used by younger people who, as a group, tend to use fewer pharmacological aids (Table 2).
The gender disparity, with men more often using snus as a smoking cessation aid, while women more often use the mobile app, and the variations found between older and younger individuals, correspond with results from a recent study of Norwegians seeking help to quit smoking [50]. Furthermore, the association between planning attempts and less smoking cessation is in accordance with Norwegian [7, 50] and international [51] studies. The negative association between earlier attempts and smoking cessation resembles results that have shown that quitting attempts increases likelihood of future attempts but not for quitting [52]. It has been argued that pre-quit and post-quit experiences have differential roles in the quitting process [53], and that while earlier quit attempts influence the tendency to try to quit, factors like personality traits, self-efficacy [35, 52], and low cigarette or nicotine dependence (33, 52) are more important for the outcome of the attempt.
Interestingly, quit attempters seem to be quite loyal to their own previous cessation aid choices, as unsuccessful quit attempters often planned to use the same aid (or lack of aid) as they had used earlier in their next quit attempt. A possible explanation for this could be that they initially had experienced some short-term success with the method, and that this encourages to use the same method in the next quit attempt. However, it is also possible that different aids appeal to different people. This would suggest that it is vital to give people who smoke a wide choice of cessation supports to ensure that everyone can find an aid that suits them.
7 Limitations
There is a shortage of socio-demographic information about participants. Notably, there is no information about participants’ educational attainment, employment status, or income, and this makes it more challenging to check the representativity of the sample. Concerning cessation activities, we lack information about the time of smoking cessation for successful quitters, and the time frame for earlier cessation attempts. In addition, social desirability bias might be an issue in self-reports, and the retrospective character of the information implies a risk of recall problems. We also lack information on the type of EC (eg., with or without nicotine) and NRT used (gums, patches, inhalers, etc.), and it is, therefore, possible that an association with quitting for some ECs and NRTs are attenuated by a lack of association for other ECs and NRTs. Finally, small group sizes made it impossible to study the combined use of cessation aids in any meaningful manner.
8 Conclusion
The use of cessation aids is relatively low in Norway and increasing the interest in using them could improve smoking quit rates. Among cessation aids, snus seems to be the most effective in the Norwegian setting. Better knowledge on the role of individual characteristics in smoking cessation might make us better equipped to optimize cessation aids for individuals.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- NRT:
-
Nicotine replacement therapy
- EC:
-
E-cigarettes
References
Stanaway JD, Afshin A, Gakidou E, Lim SS, Abate D, Abate KH, et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1923–94.
Vedøy TF. Utbredelse av sigarettrøyking i Norge [The prevalence of cigarette smoking in Norway] [web report]. Norwegian Institute of Public Health; 2023 Tobacco statistics. https://www.fhi.no/nettpub/tobakkinorge/bruk-av-tobakk/utbredelse-av-royking-i-norge/.
Borland R, Partos TR, Yong HH, Cummings KM, Hyland A. How much unsuccessful quitting activity is going on among adult smokers? Data from the International Tobacco Control Four Country cohort survey. Addiction. 2012;107(3):673–82.
Gravely S, Meng G, Hammond D, Hyland A, Cummings KM, Borland R, et al. Differences in cigarette smoking quit attempts and cessation between adults who did and did not take up nicotine vaping: findings from the ITC four country smoking and vaping surveys. Addict Behav. 2022;132: 107339.
McDermott MS, East KA, Brose LS, McNeill A, Hitchman SC, Partos TR. The effectiveness of using e-cigarettes for quitting smoking compared to other cessation methods among adults in the United Kingdom. Addiction. 2021;116(10):2825–36.
Addictovocab Addiction ontology vocabulary interface2023 https://addictovocab.org/ADDICTO:0000293.
Lund M, Lund I. Smoking cessation aids and strategies. A population-based survey of former and current smokers in Norway. BMC Public Health. 2022;22(1):1–9.
McNeill A, Brose L, Robson D, Calder R, Simonavicius E, East K, et al. 2022. Nicotine vaping in England: an evidence update including health risks and perceptions, 2022.
SCENIHR. Scientific opinion on the Health Effects of Smokeless Tobacco Products. SCENIHR (Scientific Committee on Emerging and Newly-Identified Health Risks). Belgium: Health & Consumer Protection DG, European Commission; 2008.
Vedøy TF. Utbredelse av snusbruk i Norge [prevalence of snus use in Norway] Oslo: National Institute of Public Health; 2022 https://www.fhi.no/nettpub/tobakkinorge/bruk-av-tobakk/utbredelse-av-snusbruk-i-norge/?term=&h=1
Ansteinsson V, Mdala I, Becher R, Grøtvedt L, Kopperud SE, Rukke VH. Factors associated with initiation and use of snus among adolescents. Scandinavian J Public Health. 2021. https://doi.org/10.1177/14034948211062311.
Lund I, Lund KE. How has the availability of snus influenced cigarette smoking in Norway? Int J Environ Res Public Health. 2014;11(11):11705–17.
Ramström L, Borland R, Wikmans T. Patterns of smoking and snus use in Sweden: implications for public health. Int J Environ Res Public Health. 2016;13(11):1110.
Vedøy TF, Tokle RI, Lund KE. Utbredelse av e-sigaretter og fordampere i Norge. Oslo: Folkehelseinstituttet; 2020.
Vedøy T, Lund KE. Self-reported sources for distribution of cigarettes, snus and e-cigarettes. Tidsskrift for den Norske laegeforening tidsskrift for praktisk medicin ny raekke. 2017. https://doi.org/10.4045/tidsskr.16.0994.
Hartmann-Boyce J, McRobbie H, Butler AR, Lindson N, Bullen C, Begh R, et al. Electronic cigarettes for smoking cessation. Cochrane Database Syst Rev. 2021. https://doi.org/10.1002/14651858.CD010216.pub5.
Kotz D, Fidler J, West R. Factors associated with the use of aids to cessation in English smokers. Addiction. 2009;104(8):1403–10.
Jackson SE, Kotz D, West R, Brown J. Moderators of real-world effectiveness of smoking cessation aids: a population study. Addiction. 2019;114(9):1627–38.
Smith AL, Chapman S, Dunlop SM. What do we know about unassisted smoking cessation in Australia? A systematic review, 2005–2012. Tob Control. 2015;24(1):18–27.
Filippidis FT, Laverty AA, Mons U, Jimenez-Ruiz C, Vardavas CI. Changes in smoking cessation assistance in the European Union between 2012 and 2017: pharmacotherapy versus counselling versus e-cigarettes. Tob Control. 2019;28(1):95–100.
Soulakova JN, Crockett LJ. Unassisted quitting and smoking cessation methods used in the United States: analyses of 2010–2011 tobacco use supplement to the current population survey data. Nicotine Tob Res. 2017;20(1):30–9.
Papadakis S, Katsaounou P, Kyriakos CN, Balmford J, Tzavara C, Girvalaki C, et al. Quitting behaviours and cessation methods used in eight European Countries in 2018: findings from the EUREST-PLUS ITC Europe Surveys. European J Public Health. 2020;30(Supplement_3):iii26–33.
Zhu S-H, Melcer T, Sun J, Rosbrook B, Pierce JP. Smoking cessation with and without assistance: a population-based analysis. Am J Prev Med. 2000;18(4):305–11.
Hartmann-Boyce J, Chepkin SC, Ye W, Bullen C, Lancaster T. Nicotine replacement therapy versus control for smoking cessation. Cochrane Database Syst Rev. 2018. https://doi.org/10.1002/14651858.CD000146.pub5.
Stead LF, Koilpillai P, Fanshawe TR, Lancaster T. Combined pharmacotherapy and behavioural interventions for smoking cessation. Cochrane Database Syst Rev. 2016. https://doi.org/10.1002/14651858.CD008286.pub3.
Stanley T, Massey S. Evidence of nicotine replacement’s effectiveness dissolves when meta-regression accommodates multiple sources of bias. J Clin Epidemiol. 2016;79:41–5.
Zhu S-H, Lee M, Zhuang Y-L, Gamst A, Wolfson T. Interventions to increase smoking cessation at the population level: how much progress has been made in the last two decades? Tob Control. 2012;21(2):110–8.
Watkins SL, Thrul J, Max W, Ling PM. Real-world effectiveness of smoking cessation strategies for young and older adults: findings from a nationally representative cohort. Nicotine Tob Res. 2020;22(9):1560–8.
Larabie L. To what extent do smokers plan quit attempts? Tob Control. 2005;14(6):425–8.
Ferguson SG, Shiffman S, Gitchell JG, Sembower MA, West R. Unplanned quit attempts—results from a US sample of smokers and ex-smokers. Nicotine Tob Res. 2009;11(7):827–32.
Tan J, Zhao L, Chen H. A meta-analysis of the effectiveness of gradual versus abrupt smoking cessation. Tob Induc Dis. 2019. https://doi.org/10.18332/tid/100557.
Lindson N, Klemperer E, Hong B, Ordóñez-Mena JM, Aveyard P. Smoking reduction interventions for smoking cessation. Cochrane Database Syst Rev. 2019. https://doi.org/10.1002/14651858.CD013183.pub2.
Hyland A, Borland R, Li Q, Yong HH, McNeill A, Fong GT, et al. Individual-level predictors of cessation behaviours among participants in the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15(suppl 3):iii83–94.
Jarvis MJ, Cohen JE, Delnevo CD, Giovino GA. Dispelling myths about gender differences in smoking cessation: population data from the USA, Canada and Britain. Tob Control. 2013;22(5):356–60.
Smit ES, Hoving C, Schelleman-Offermans K, West R, de Vries H. Predictors of successful and unsuccessful quit attempts among smokers motivated to quit. Addict Behav. 2014;39(9):1318–24.
van Wijk EC, Landais LL, Harting J. Understanding the multitude of barriers that prevent smokers in lower socioeconomic groups from accessing smoking cessation support: a literature review. Prev Med. 2019;123:143–51.
Gross B, Brose L, Schumann A, Ulbricht S, Meyer C, Völzke H, et al. Reasons for not using smoking cessation aids. BMC Public Health. 2008;8(1):1–9.
Morphett K, Partridge B, Gartner C, Carter A, Hall W. Why don’t smokers want help to quit? A qualitative study of smokers’ attitudes towards assisted vs. unassisted quitting. Int J Environ Res Public Health. 2015;12(6):6591–607.
Lund KE, Scheffels J, McNeill A. The association between use of snus and quit rates for smoking: results from seven Norwegian cross-sectional studies. Addiction. 2011;106(1):162–7.
Lund I, Christiansen SG. Association between snus use over time and smoking cessation in Norwegian smokers. Addiction. 2020;115(1):170–4.
Fagerstrom K, Rutqvist LE, Hughes JR. Snus as a smoking cessation aid: a randomized placebo-controlled trial. Nicotine Tob Res. 2012;14(3):306–12.
Lund KE. Association between willingness to use snus to quit smoking and perception of relative risk between snus and cigarettes. Nicotine Tob Res. 2012;14(10):1221–8.
Blok DJ, de Vlas SJ, van Empelen P, van Lenthe FJ. The role of smoking in social networks on smoking cessation and relapse among adults: a longitudinal study. Prev Med. 2017;99:105–10.
Kasza KA, Edwards KC, Kimmel HL, Anesetti-Rothermel A, Cummings KM, Niaura RS, et al. Association of e-cigarette use with discontinuation of cigarette smoking among adult smokers who were initially never planning to quit. JAMA Netw Open. 2021;4(12):e2140880-e.
Rosen LJ, Galili T, Kott J, Rees V. Beyond “Safe and Effective” The urgent need for high-impact smoking cessation medications. Prev Med. 2021;105:106567.
Mersha AG, Eftekhari P, Bovill M, Tollosa DN, Gould GS. Evaluating level of adherence to nicotine replacement therapy and its impact on smoking cessation: a systematic review and meta-analysis. Arch Public Health. 2021;79(1):1–14.
Yang B, Owusu D, Popova L. Effects of a nicotine fact sheet on perceived risk of nicotine and e-cigarettes and intentions to seek information about and use e-cigarettes. Int J Environ Res Public Health. 2020;17(1):131.
McKeganey N, Dickson T. Why don’t more smokers switch to using e-cigarettes: the views of confirmed smokers. Int J Environ Res Public Health. 2017;14(6):16.
Carrasco-Hernandez L, Jódar-Sánchez F, Núñez-Benjumea F, Conde JM, González MM, Civit-Balcells A, et al. A mobile health solution complementing psychopharmacology-supported smoking cessation: randomized controlled trial. JMIR Mhealth Uhealth. 2020;8(4): e17530.
Lund M, Kvaavik E. Methods used in smoking cessation and reduction attempts: findings from help-seeking smokers. J Smok Cessat. 2021;2021:6670628.
Garnett C, Shahab L, Raupach T, West R, Brown J. Understanding the association between spontaneous quit attempts and improved smoking cessation success rates: a population survey in England with 6-month follow-up. Nicotine Tob Res. 2020;22(9):1460–7.
Diemert LM, Bondy SJ, Brown KS, Manske S. Young adult smoking cessation: predictors of quit attempts and abstinence. Am J Public Health. 2013;103(3):449–53.
Borland R, Yong H-H, Balmford J, Cooper J, Cummings KM, O’Connor RJ, et al. Motivational factors predict quit attempts but not maintenance of smoking cessation: findings from the International Tobacco Control Four country project. Nicotine Tob Res. 2010;12(suppl_1):S4–11.
Acknowledgements
Data for this study was made available by the Norwegian Directorate for Health.
Funding
Open access funding provided by Norwegian Institute of Public Health (FHI). This study was funded by the Norwegian Institute of Public Health and the Norwegian Directorate for Health. The data was collected by the Norwegian Directorate for Health. The funding agencies had no influence on the design of the study, the data analyses, the interpretation of data or the writing of the manuscript.
Author information
Authors and Affiliations
Contributions
IL was responsible for the statistical analyses and the interpretation of results, and drafted the manuscript. ML contributed to statistical analyses and interpretations and read and commented manuscript drafts. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All participants have given their consent to participate and can withdraw this consent and demand their personal information to be deleted at any point in time. For this study, we received only anonymous and non-sensitive/non-health-related data, and the survey was therefore exempt from further ethical approval.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lund, I., Lund, M. Quit smoking: methods and outcomes for Norwegian adults. Discov Soc Sci Health 3, 12 (2023). https://doi.org/10.1007/s44155-023-00043-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44155-023-00043-3