Abstract
Background
Malaria infection during pregnancy presents a substantial health threat, adversely impacting both the mother and fetus. Its pathogenesis and clinical consequences further complicate diagnosis, treatment, and prevention, particularly in endemic regions. The precise impact of malaria infection on hematological profiles needs to be clearly elucidated, and the occurrence of malaria in expectant mothers still needs to be explored. Consequently, this study aims to assess the prevalence of malaria infection among pregnant women as well as to investigate and correlate the effects of this infection on the hematological parameters of pregnant women in Yola, Nigeria.
Methods
A structured hybrid questionnaire was used to gather socio-demographic, clinical, and obstetric data from 100 pregnant women aged 15–45 years. Malaria parasitemia was determined and confirmed using a light microscope, blood smear-staining techniques, and rapid diagnostic tests (RDT). At the same time, the packed cell volume (PCV) was measured using a microhematocrit reader. Also, the complete blood count was determined using Turk’s solution and Neubauer’s counting chamber (hemocytometer).
Results
Out of the 100 participants in the study, 76 tested positive for malaria, resulting in a prevalence rate of 76%. The age group between 30 and 34 years and multigravida recorded high values of malaria-infected women, accounting for 18 (23.7%) and 49%, respectively. Also, the study’s findings indicate that malaria-infected pregnant women had a significantly higher occurrence of anemia than those not infected (P = .045). In addition, eosinophil counts, total white blood cells (WBC), and neutrophil count were notably higher in pregnant women infected by malaria compared to those not infected (P < .05). Conversely, lymphocyte count, basophil count, and monocyte count were significantly lower in pregnant women infected by malaria compared to uninfected pregnant women.
Conclusion
Pregnant women participating in prenatal care at the Specialist Hospital in Yola, Nigeria, exhibited a relatively high occurrence of malaria parasite infection, and these infected pregnant women displayed a notable change in specific hematological parameters. The findings of this study offer valuable insights into the pathogenesis of malaria during pregnancy and contribute to improved diagnostic and management strategies for pregnant women at risk of malaria infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Background
Malaria continues to pose a significant global health challenge, particularly in regions with high transmission rates [1]. Due to elevated steroid levels during pregnancy and the development of a new organ called the placenta, pregnant women constitute the leading vulnerable group of adults in malaria-endemic regions, as their immune system is significantly weakened [1, 2]. The increased levels of human chorionic gonadotropin (HCG) and prolactin levels, which remain increased throughout pregnancy, further weaken pregnant women’s immune responses and, thus, increase their vulnerability to malaria infection [3]. Therefore, malaria remains a persistent challenge during pregnancy both in obstetrics and medicine, necessitating comprehensive and complex strategies. In 2009, the vulnerability index of malaria during pregnancy in sub-Saharan African countries was estimated to be 11.6 million [3], indicating a moderately high risk of malaria transmission (accounting for 35% of all pregnancies in the region) [3, 4]. As a result, 822,000 babies were born with low birth weight [3]. Africa experienced a significant incidence of low-weight babies, resulting in an uneven halving of the global estimation of low-weight babies caused by malaria. According to the World Health Organization, malaria is highly prevalent in regions characterized by extreme poverty and areas where disease identification, documentation, and reporting methods are lacking [5].
Plasmodium, a genus of parasitic protozoans, is humans' primary source of malaria [1]. Within the family of Plasmodiidae, there is only one genus: Plasmodium [1]. This genus belongs to the phylum Apicomplexa, class Aconoidasida, and order Haemosporida. It comprises over 200 species capable of causing malaria [6]. However, among these species, five are commonly found to infect humans. Plasmodium falciparum and Plasmodium vivax have the widest distribution, followed by Plasmodium malariae, Plasmodium ovale, and Plasmodium knowlesi [6, 7]. On the other hand, P. falciparum poses a grave danger to human health, resulting in yearly fatalities [7]. The capacity of plasmodium species to thrive in Africa may be attributed to the region's prevailing hot and humid environmental conditions [8]. Human transmission of Plasmodium species occurs when an individual is bitten by an infected female Anopheles mosquito [9]. The malaria parasite initially undergoes development and replication within liver cells, followed by proliferation within red blood cells [10]. Additionally, transmission can occur through different routes, including blood transfusions, organ transplants, sharing needles or syringes, and from a pregnant mother to her developing fetus [9]. The impact of malaria infection on the human body, in terms of both sickness and death, is known as its virulence. The diversity in parasite virulence plays a role in determining the clinical consequences observed in cases of malaria infections [11, 12]. The presence of asexual erythrocytic or blood-stage parasites in the blood cells is responsible for all the clinical symptoms related to malaria infection [10]. Consequently, malaria is considered a highly significant parasitic disease, leading to substantial health issues that have attracted worldwide attention [11].
Expectant mothers are more prone to mosquito bites and malaria infection compared to women who are not pregnant, as mosquitoes find them particularly appealing [3, 13]. The increased attractiveness may be attributed to at least two physiological factors. Firstly, mosquitoes are attracted to moisture and carbon dioxide, and pregnant women in the advanced stages of pregnancy exhale 21% more carbon dioxide [13] than non-pregnant women. Secondly, it has been observed that the abdomen of a pregnant woman is 0.7 Celsius hotter and warmer, releasing more volatile substances from their skin [3]. The physiological transformations during pregnancy and the pathological alterations caused by malaria infection mutually influence and exacerbate one another’s progression, creating challenging conditions for the mother, the fetus, and the treating physician [2, 9]. The presence of P. falciparum in pregnant women can result in significant consequences and further deteriorate the subsequent outcomes [14]. In pregnancy, the morbidity linked to malaria infection encompasses conditions such as anemia, fever, low blood sugar, cerebral malaria, pulmonary edema, postpartum infection, and the risk of severe malaria and excessive bleeding leading to death [9, 14].
On the other hand, newborns face various challenges, such as being born with a low weight, being premature, contracting malaria infection, and experiencing a high mortality risk [14, 15]. Pregnant women who have experienced multiple episodes of malaria infection before conceiving tend to develop partial resistance to severe malaria [2, 15]. However, due to alterations in their immune systems during pregnancy and the emergence of a new organ, the placenta, which becomes a target site for parasite attachment, pregnant women may experience a reduction in their immunity to malaria infection [2]. In this scenario, primigravidae who lack immunity are typically the most impacted [14, 15].
Diverse clinical manifestations of various diseases, including endemic conditions like malaria, can potentially influence hematological parameters, indicating their impact on human health [16, 17]. The changes in hematological parameters are prevalent complications of malaria infection and hold substantial significance in the development of the disease. These modifications involve vital constituents of the blood cells, like erythrocytes, leukocytes, and thrombocytes [17]. Two crucial factors cause the primary impact of malaria during pregnancy: firstly, the weakened immune system during pregnancy, and secondly, the trapping of infected red blood cells in the placenta [3]. In contrast, when adults contract malaria, the infected red blood cells are trapped in the spleen, resulting in a shortage of folic acid and the development of microcytic anemia. Nevertheless, pregnant women encounter a unique circumstance where the placenta serves as an additional site for the sequestration of infected red blood cells [14]. Consequently, pregnant women experience a significantly higher degree of anemia; as a result, malaria in pregnancy is recognized as a contributing factor to increased occurrences of miscarriage, intrauterine death, preterm birth, underweight newborns, perinatal health problems, and mortality [7].
The occurrence of malaria in pregnant women, specifically within the placenta, spans a wide range, starting from 1% and extending up to 50%, based on the degree of malaria transmission in a given area. Interestingly, many infected pregnant women may remain unaware of the degree of malaria infection in their bodies [18]. This is due to the protective effect of previous exposure to the disease, which grants the pregnant woman acquired immunity against clinical malaria [18]. As a result, the manifestation and complexities of malaria in pregnant women vary depending on the malaria transmission intensity in a specific region and the immune response acquired by the pregnant women [2, 3]. Malaria incidence is believed to be greater during the initial and subsequent pregnancies, but it tends to decrease as the number of pregnancies increases [19]. This decrease is linked to the progressive rise in immune defenses with each additional pregnancy [19].
A significant advancement in the research on malaria during pregnancy is the recognition that sulfadoxine–pyrimethamine, which has progressively replaced chloroquine (CQ) as the primary treatment, is now showing an increasing rate of ineffectiveness [2, 8]. Hence, it is crucial to establish plans and frameworks to determine the best drug or drug combination to prevent malaria during pregnancy, along with a well-organized approach to preventing malaria infection. The World Health Organization (WHO) has recommended three strategic approaches for controlling malaria in pregnant women, particularly in Africa. These methods consist of intermittent preventive treatment (IPT), efficient case management (diagnosis and treatment of illness), and the utilization of insecticide-treated nets. (ITNs) [7, 8].
Although previous studies have investigated the prevalence of malaria parasite infection among pregnant women attending antenatal care, particularly in Northeastern Nigeria, there is a limited understanding of its impact on hematological parameters. Existing research has mainly focused on the association between malaria infection and adverse pregnancy outcomes, such as low birth weight and maternal anemia [15, 19, 20]. Consequently, a detailed examination of specific hematological parameters and their alterations due to malaria parasite infection must be included. Similarly, while the implication of malaria infection is evident, there needs to carry out a more thorough investigation into the extent of significant changes resulting from the pathogenesis of malaria parasite infection. Specifically, certain hematological parameters have not been identified as biomarkers for evaluating the severity of malaria infection, particularly in pregnant women who transfer their immune system to their developing fetus. Therefore, this study aims to address the existing research discrepancy by investigating the effect of malaria parasite infection on the hematological parameters of pregnant women participating in prenatal care at a specialist Hospital, Yola. This would involve assessing the pack cell volume (hemoglobin level), total white blood cell counts, etc., in relation to the presence and severity of malaria infection. By investigating these parameters, we can gain a more comprehensive understanding of how malaria impacts the hematological profile of pregnant women and potentially identify biomarkers for early detection and monitoring of malaria infection during pregnancy. Additionally, this study will consider the influence of other factors, such as gestation and age, on the relationship between malaria infection and hematological parameters. This will help account for potential confounding factors and provide a more accurate assessment of the impact of malaria on pregnant women’s hematological profiles.
By addressing this research gap, we can ultimately enhance our understanding of the hematological consequences of malaria parasite infection during pregnancy. This may improve diagnostics and management strategies for pregnant women at risk of malaria infection.
2 Methods
2.1 Study area
The research was conducted at Specialist Hospital Yola, Adamawa State, Nigeria. Specialist Hospital, Yola is a government-owned general hospital, which serves as a secondary healthcare facility in Yola, offering various medical services. Several comprehensive health centers in the state operate under this hospital, making it a significant reference study area for our research. The hospital is located in Yola, the capital city of Adamawa State, at geographical coordinates of 9° 17′ 0″ North and 12° 28′ 0″ East. Yola has a tropical climate characterized by alternating dry and rainy seasons. The rainy season begins in April and continues until mid-to-late October. The dry season, on the other hand, starts in November and lasts until March. In April, the temperatures in Yola can reach up to 40 °C, while during December and early January marks the harmattan period due to northeasterly trade winds, minimum temperatures can drop as low as 18.3 °C [21].
2.2 Sample design and population
A structured hybrid questionnaire was used to gather socio-demographic, clinical, and obstetric data from 100 pregnant women during antennal care sessions at Specialist Hospital, Yola, from April to June. Samples were collected every Wednesday biweekly. Prior to sample collection, informed consent was obtained from all study subjects who participated in this study.
2.3 Inclusion criteria
All gravidae women (aged 15+) who registered for antenatal care with signs of malaria infection within the past 48 h, particularly having an axillary temperature of 37.5 °C or higher, also, they were permanent residents of the study area who had consented to participate.
2.4 Exclusion criteria
All gravidae women who had taken antimalaria drugs in the last four weeks before the study period were excluded from this study. Also, pregnant women with pre-existing medical conditions that may affect hematological parameters (such as hematological disorders and chronic illnesses) were excluded from this study.
2.5 Sample size
Sample size was determined using the formula n = P (1 − P) Z2 /d2 [22] where n = sample size, P is the estimated prevalence value, d is the error margin at 0.05 (5%), which is the level of significance or precision, and Z is the confidence level of the results (1.96).
2.6 Sample collection
About 2 ml of venous blood was promptly transferred into a well-labeled bottle containing ethylene diamine tetra acetic acid (EDTA) by a trained laboratory scientist using a 5 ml syringe. Only one blood sample per patient was collected.
2.7 Malaria diagnosis
Three blood droplets were placed on a microscope slide that was completely free of grease to make thick and thin films. These drops were spread in a circle with a diameter of approximately 1 cm at one end of the slide to make a thick film. Additionally, about 1 cm away from the thick film, one drop of blood was placed and spread thinly to form a thin film. The smears were then left to air-dry for an hour. Subsequently, the smeared slides were stained in a 3% Giemsa solution for 45 min. After rinsing and drying the slides, they were observed under a 100× objective lens with an oil immersion [23]. The parasite intensity was assessed using the plus system, which involved assigning the values as follows: 0 indicated the absence of parasites, + indicated mild parasitemia with 10–90 parasites per 100 high power field, ++ indicated moderate parasitemia with 100–1000 parasites per 100 high power field, and +++ marked severe parasitemia with 1000–10,000 parasites per high power field.
The blood samples were also evaluated for the presence of malaria parasite antigens using malaria rapid diagnostic tests (RDTs) to confirm the infection of malaria parasites. The RDT test was performed according to the manufacturer's instructions. Also, the RDTs used in this study were SD BIOLINE, Standard Diagnostic, Inc., USA. The RDT kits worked on the P. falciparum HRP-2 monoclonal antibody binding principle.
2.8 Hematological analysis
The white blood cell count was measured using Turk’s solution and Neubauer’s counting chamber (hemocytometer). An anticoagulated blood sample was drawn precisely at the 0.5 mark on the white blood cell (WBC) pipette. Turk’s solution was then added to the 11th mark on the white blood cell (WBC) pipette. The content in the pipette was mixed, and after 5 min, a few drops of the mixture were discarded. The counting chamber was filled with the remaining mixture and allowed to settle for approximately 2–3 min. The objective was set to low power (10×), focusing on one of the corners marked with a “W” on the counting machine. The cells were examined using an oil immersion microscope. Finally, the cells in all four “W” marked corner squares were counted [24].
Packed cell volume (PCV) was also measured using a microhematocrit reader, centrifuge, and capillary tube. An anticoagulated blood sample was collected in a capillary tube and was sealed at one end. The tube was spun at 10,000–12,000 rpm for approximately 5 min in a centrifuge. The resulting packed cell volume (PCV) percentage was evaluated by reading the measurement using a microhematocrit reader [25].
2.9 Data analysis
The data was evaluated and processed using IBM SPSS statistics for Windows, version 20 [26], and the findings were displayed as the mean value ± SD (standard deviation). To evaluate the statistical significance of qualitative variables, the Chi-square test (χ2) was employed. The determination of statistical significance relied on evaluating P-values below the threshold of 0.05.
3 Results
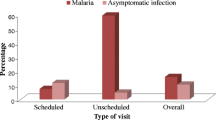
3.1 Malaria prevalence among the sample subjects
The study findings reveal a substantial occurrence of malaria infection among the study population. Out of the 100 blood samples analyzed under a microscope, 76 were identified as being infected with the malaria parasite, resulting in a 76% rate of infection. The statistical analysis of the data indicates that the observed malaria infection rate is statistically significant (χ2 = 3.84, P-value = 0.03). Also, from the study, all instances of parasitemia among the study subjects were attributed to P. falciparum.
3.2 Demographic report of the sample population
Table 1 shows the distribution of malaria parasites among pregnant women participating in prenatal care at the Specialist Hospital. The age group of 30–34 years had the highest occurrence of malaria infection, with 18 infected women, as detailed in Table 1. Also, within this age group, women with moderate parasitemia (++) accounted for the highest rate of infections, with exactly 9 (39.1%) infected women. Moreover, among the age group studied, the lowest malaria prevalence was spotted in women aged 35–39 years, with 5 infected pregnant women. Conversely, the age group with the mean average number of infected red blood cells (RBC) was observed among pregnant women aged 15–19 years, with 12 infected women. Nevertheless, the statistical analysis did not demonstrate a significant correlation between the rate of malaria infection and the age groups within the sampled population (P-value = 0.072, mean value = 12.67).
Table 2 illustrates the distribution of malaria infection among pregnant women based on their number of pregnancies (gestation). The highest occurrence of malaria infection was observed in women with multiple pregnancies (multigravida); this study recorded 49 malaria-infected women in this age group. Furthermore, within the group of women who had multiple pregnancies (multigravida), those who had moderate (++) and mild (+) parasitemia had the highest prevalence rate, accounting for 22 (71.0%) and 22 (59.5%), respectively. At the same time, the occurrence of malaria infections was lowest among primigravidae women, with a total of 27 malaria-infected women. However, no statistically significant difference was observed while analyzing the connection between the rate of malaria infection and the number of pregnancies (P-value = 0.362).
3.3 Packed cell volume (PCV)
Table 3 provide information on how the malaria parasite impacts the sampled population's packed cell volume (PCV). This study identified anemic pregnant women as having a packed cell volume (PCV) of less than 30. The highest occurrence of infection was observed among malaria-infected pregnant women who had their packed cell volume to be less than 30 (PCV < 30), accounting for 63 (82.9%) out of 76 (100%) infected pregnant women. In comparison, those with a mean packed cell volume (PCV) recorded 13 (17.1%) out of 76 (100%) cases. Table 4 offers additional insights. The statistical analysis revealed a significant association between the rate of malaria infection and packed cell volume (PCV) (P-value = 0.045).
3.4 Blood cell count
Table 4 depicts the pairwise statistical comparisons of the impact of malaria parasite infection on various hematological parameters. These parameters include total white blood count (WBC), basophil count, monocyte count, lymphocyte count, and eosinophil count. These hematological parameters were evaluated in the study to assess the effects of the malaria parasite. Based on the data presented in Table 4, it can be observed that malaria-infected pregnant women had a significantly higher mean packed cell volume (PCV < 30) compared to those without parasitemia. The mean packed cell volume (PCV) values were 35.4 ± 1.67 SD (standard deviation) for the infected group, whereas the non-infected group had 14.1 ± 0.67 SD (P-value = 0.045). This difference in mean packed cell volume (PCV) values was statistically significant, indicating a notable variation between the two groups (infected and un-infected groups). The pregnant women who were infected had a higher total white blood cell (WBC) count of 11.3 ± 0.73 compared to non-parasitized pregnant women, whose white blood cell (WBC) count was 4.21 ± 0.27 (P-value = 0.021). The basophil counts in women infected with P. falciparum were significantly lower than those without parasitemia, with values of 7.07 ± 0.35 vs. 14.1 ± 0.69, respectively (P-value = 0.265). The neutrophil count in parasitized pregnant women, with a value of 24.1 ± 1.21, was relatively higher than that of the uninfected pregnant women, which was 6.4 ± 0.04 (P-value = 0.033). The monocyte levels in infected pregnant women, with a value of 1.41 ± 0.06, were considerably lower compared to uninfected women, with a value of 22.6 ± 0.94. However, the observed difference did not show statistical significance (P-value = 0.111). Additionally, Table 4 demonstrates that infected pregnant women had a decreased lymphocyte count, with standard deviation (SD) values of 2.7 ± 0.07. In contrast, uninfected women had a standard deviation (SD) value of 14.1 ± 1.0 for lymphocytes (P-value = 0.227). A statistically significant correlation was observed between the eosinophil levels of malaria-infected pregnant women and non-parasitized pregnant women, with eosinophil levels being lower in non-parasitized pregnant women (4.24 ± 0.72) compared to infected pregnant women (11.3 ± 0.73) (P-value = 0.049). This indicates a notable difference in average eosinophil values.
4 Discussion
4.1 Prevalence of malaria
The examination of the collected samples revealed that 76 out of the 100 pregnant women tested positive for Plasmodium, indicating a 76% infection rate. Conversely, 24 pregnant women were not infected with Plasmodium. This finding demonstrates that pregnant women in the study area were exposed to malaria parasites. The high prevalence examined in this study is probably connected to the abundance of female Anopheles mosquitoes, the vectors of malaria parasites in the region. Furthermore, the increased occurrence of malaria infection among the participants in the study could be attributed to the pregnant women’s failure to follow the recently approved intervention strategies for malaria control and prevention during pregnancy, as outlined by the World Health Organization (WHO). The findings of this study align with the research conducted in Osogbo (Osun), Lugbe and Gosa (Abuja), Imo, and Gombe in Nigeria by Bolaji et al. [27] Ohalete et al. [1], Onyemaechi & Malann [3], and Yusuf et al. [28] reported a relatively higher prevalence rate of 53.9%, 80.9%, 70.5%, and 74%, respectively. However, it differs from the study conducted in Kastina, Yola (Adamawa), Ikole (Ekiti), and Anyigba (Kogi), Nigeria, by Lawal et al. [29], Kwala et al. [8], Simon-Oke et al. [30], and Okolo et al. [31], who reported a relatively lower prevalence rate of 24.25%, 36.74%, 40.2%, and 40%, respectively. The variations in the reported findings could be due to differences in malaria epidemiology among various study populations, and in climatic conditions or seasons where the data were collected from different regions. However, this study was conducted during a period known to be the peak of rainfall in the study area. The warm and humid environmental conditions favor the breeding of the parasites' vector (Anopheles mosquito), hence the high prevalence recorded in this study [8]. On the other hand, another possible cause for the difference in findings is the laboratory personnel's skill and proficiency in handling, staining, and analyzing the microscopic results of the blood films [32]. This study strictly followed protocols, methods, and safety measures during the preparation and staining of slides, guaranteeing that the stained slides were unambiguous and easily interpretable, thus minimizing the chances of erroneous conclusions.
4.2 Age index of malaria prevalence
The study’s findings, as demonstrated in Table 1, indicated that pregnant women aged 30–34 had the highest occurrence of malaria parasite infection, accounting for 18 (23.7%) malaria-infected women. The age group 25–29 followed closely behind with 17 (22.4%) malaria-infected women, whereas the lowest prevalence was observed among women aged 35–39, with 5 (6.6%) malaria-infected women. Nevertheless, the observed difference in the rate of malaria infection in relation to age was not statistically significant. This study concurred with the findings of Ohalete et al. [1], Umar et al. [33], Bolaji et al. [27], and Okoroiwu [32], who concluded that the occurrence of malaria is not influenced by age. This study demonstrates a slight contrast to the research conducted by Mangusho et al. [34] and Yusuf et al. [28]. They discovered that pregnant teenagers and young adult women had a higher vulnerability to malaria infection than older expectant mothers. It is further explained that older women acquire immunity to malaria over time due to frequent infections, leading to lower levels of malaria parasites in adult women [34]. Oladimeji et al. [35] further revealed from their study that one potential reason for the lower prevalence of malaria infection among multigravida was the improved use of malaria intervention strategies by older pregnant women [35]. There are two possible explanations for the increased occurrence of malaria infection in the 30–34 age bracket: first, a smaller proportion of pregnant women examined in comparison to other age groups, and second, the direct impact of previous pregnancies, as a considerable proportion of the study subjects may be old and experienced mothers rather than younger, first-time mothers [34].
4.3 Gravidity implication of malaria infection
Analyzing the result of this research, it can be observed in Table 2 that pregnant women who have been pregnant multiple times (multigravida) had a higher infection rate compared to women who were pregnant for the first time (primigravidae). This finding contradicts the findings of Yimam et al. [36], Mlugu et al. [37], and Olukosi et al. [38], who reported that primigravidae were more prone to contracting malaria infection during pregnancy than multigravida. This is because primigravidae lack immunity to fight against malaria infection during pregnancy, while multigravida have acquired immunity against malaria during pregnancy [32]. Nevertheless, the outcome of this study was consistent with the research conducted by Suliman et al. [39] and Kiemde et al. [40], indicating that women with multiple pregnancies are the most vulnerable group and that the number of previous pregnancies does not influence protective immunity during pregnancy. The variations in the reports could be attributed to the insufficient nourishment of the multigravida in our sample population, potentially resulting in inadequate development of immunity against the malaria parasite [32, 41]. Furthermore, the variations in findings might be explained by the fact that women do not typically encounter regions with a high prevalence of the disease during their first pregnancy but are more common during subsequent pregnancies [33].
4.4 Impact of malaria infection on the Packed Cell Volume (PCV) level
Anemia is a common complication that often occurs in cases of malaria infection, especially among pregnant women living in areas of high transmission. Although the precise pathogenesis of malaria infection during pregnancy is not fully understood, it is generally attributed to the parasite’s target being the red blood cells (RBC), resulting in their destruction [42], the increased removal of both infected and uninfected cells [43], compromised bone marrow function, and the level of parasitemia [44]. Analysis of the result from this study indicates that the packed cell volume of most malaria-infected pregnant women was relatively low (PCV < 30) compared to uninfected pregnant women, as shown in Table 3. This finding aligned with the reports of Ndamukong-Nyanga et al. [45], Yusuf et al. [28], and Binuyo et al. [46]. Furthermore, the finding of this study agrees with a separate investigation carried out in Sokoto, Nigeria, by Erhabor et al. [47], who documented that the reduced packed cell volume (PCV) levels reflect anemia resulting primarily from the mechanical destruction of partitioned red blood cells, the nutritional status of pregnant women with infections, and the spleen’s removal of segregated and defected cells.
5 Effects of malaria on other blood parameters
5.1 Total white blood cells (WBC)
The white blood cells (WBCs) are considered vital components of the immune system’s defense against diseases. Consequently, the number of white blood cells in the body can fluctuate, either decreasing or increasing, based on the specific condition or reaction within the body [48]. The findings of this study indicate that infected pregnant women had a higher total white blood cell (WBC) count than uninfected women (P = 0.021). This finding concurs with the research carried out by [49, 50], which concluded that there is a correlation between increasing parasite density and an increase in white blood cells (WBC). However, the findings of this study contrast with the findings of Obebe et al. [51], Pinedo-Cancino et al. [52], and Ndamukong-Nyanga et al. [45]. The rise in overall white blood cells observed in this study may be linked to the intensified invasion and replication of the malaria parasite within the red blood cells of these pregnant women. During different stages of malaria infection, it is common for the white blood cells to change. Moreover, the findings of this study further agree with the study carried out by Abbas et al. [42], who documented that the elevated white blood cell count could be due to an increased immune response against parasitic infections. However, Abbas et al. [42] further stated that it was necessary to note that the increased white blood cell (WBC) levels may not be exhibited in all cases, as some pregnant women, particularly those with complicated malaria or non-immune adults to malaria, may present with leucopenia (a reduced white blood cell (WBC) count). Furthermore, following prior research by Dockree et al. [53] and Yusuf et al. [28], during the early stages of pregnancy, the total white blood cell count experiences an elevation and continues to increase throughout pregnancy due to neutrophil leukocytosis.
5.2 Neutrophil
The findings of this study also revealed that pregnant women who were infected with malaria parasites had a higher concentration of neutrophils than those who were not infected with the parasite (P = 0.03). The findings of this study disagreed with the work carried out by Adamu & Jigam [54] and Pinedo-Cancino et al. [52], who reported a decreased segmented neutrophil level among malaria-infected pregnant women. Nevertheless, the finding of this study agreed with the findings of Binuyo et al. [46], Ogbodo et al. [49], and Foghi et al. [16]. They reported that the rise in neutrophil levels may be linked to the notable immune regulatory functions of neutrophils, as they are among the primary stimulators during inflammation and exhibit significant immune regulatory activities. The observed increase in neutrophil levels may be linked to the presence of pathogens in the body [55]. Moreover, in the initial stages of pregnancy, the fetus is occasionally perceived as a foreign body, resulting in an increased count of neutrophils that actively engage with antigens [56]. The rise in neutrophil levels aims to counteract foreign elements such as pathogens and even the developing fetus [56].
5.3 Eosinophil
The findings of this study indicate that the level of eosinophils in pregnant women infected with malaria parasites was higher in comparison to pregnant women without malaria infection (P = 0.05). This finding corroborates the result of Foghi et al. [16]. Two factors could explain the rise in eosinophil levels observed in this study. Firstly, eosinophils play a crucial role in identifying and combating parasites as well as certain infections within the human body [57]. Secondly, it indicates the possibility of eosinophil release following bone marrow suppression [58]. Moreover, another potential factor that can enhance the generation of eosinophils is the increased inoculation of the infective stage of Plasmodium [59].
5.4 Monocyte
The decline in monocyte levels among the pregnant women infected with malaria parasites in this study was in contrast with previous findings of Yusuf et al. [28], which indicate that during malaria infection, Plasmodium activates mononuclear cells that generate inflammatory molecules (cytokines) like tumor necrosis factor (TNF), interleukin-1 (IL1), and interleukin-6 (IL6). These molecules (cytokines) stimulate the liver to produce acute-phase inflammatory proteins [60], including C-reactive protein (CRP), which rises in response to malaria infection [60]. Nevertheless, the result concurred with the findings of Ogbodo et al. [49] and Garba et al. [61]. The decrease in monocyte levels observed in this study can be attributed to the activation of an innate response caused by Plasmodium infection, which alters monocyte metabolism, chromatin, and expressed receptors. These alterations could decrease tolerance or enhance the host's resistance to reinfection [62].
5.5 Lymphocyte
The results from the study also indicated a reduction in the lymphocyte level for malaria-infected pregnant women. The findings of this study align with the discoveries made by Binuyo et al. [46] and Ejike et al. [63]. They found that patients with acute malaria infection caused by P. falciparum commonly experience decreased peripheral blood lymphocytes, possibly due to lymph node sequestration and apoptosis-induced cell death. However, the finding differs from that of Foghi et al. [16], Okamgba et al. [64], and Adamu & Jigam [54]. The decreased lymphocytic level found in this study could be attributed to the redistribution of lymphocytes from being trapped in the spleen, resulting in either a decrease or increase in lymphocytes associated with malaria infection [65].
5.6 Basophil
The study’s finding indicates a reduction in basophil levels, which may be linked to the tissue's recruitment and buildup of cells. This finding aligns with the research conducted by Stephane et al. [66]. Furthermore, another study revealed that this decrease could explain various reductions in peripheral blood [67]. However, this finding contradicts the findings of Adamu & Jigam [54] and Ifeanyi [68], who documented that basophil levels do not change significantly during malaria in pregnancy.
6 Limitations
While this study stands out for its distinctiveness and comprehensive exploration of blood profile biomarkers associated with malaria infection in pregnant women, along with evaluating its prevalence, it is essential to acknowledge its limitations. The study, however, has two-fold limitations: First, the samples were solely obtained from one hospital, disregarding broader regions within Yola. Secondly, the sample size was relatively small, which could have resulted in an inaccurate evaluation of malaria infection prevalence among pregnant women in this region. Consequently, there are still notable discrepancies; nonetheless, this research will be valuable in improving the understanding of contradictory findings from reports regarding malaria pathogenesis in pregnancy and its impact on hematological parameters.
7 Conclusions
In conclusion, this study evaluated the prevalence of malaria infection among pregnant women attending antenatal clinics at specialist hospital Yola. Overall, the rate of malaria parasite infection among pregnant women within the study population was relatively high, accounting for a 76% occurrence rate. Also, the study uncovered that four blood profiles were significantly altered among malaria-infected pregnant women. These include a low packed cell volume (PCV < 30), indicating anemia; a high white blood cell count (P = 0.021), indicating the severity of malaria parasite infestation within the immune system; an elevated neutrophil count (P = 0.03), demonstrating intense invasion and replication of malaria parasites within the red blood cells of the infected pregnant women; and a high level of eosinophils (P = 0.05), indicating increased inoculation of the infective stage of Plasmodium. Moreover, these parameters are critical indicators (biomarkers) of malaria infection. Consequently, malaria infection can affect the health and well-being of the pregnant woman and the developing fetus. These findings emphasized the importance of regularly monitoring hematological profiles in pregnant women infected with malaria and the need for prompt intervention to prevent complications.
Data availability
The datasets generated during and/or analyzed during the current study are available from corresponding author on reasonable request.
References
Ohalete C, Dozie I, Nwachukwu M, Obiukwu C (2020) A study of Socio-economic effect and epidemiology of malaria in pregnant women in Imo states, Nigeria. Int J Obstetr Gynecol 8(6):001–006
Bauseman M, Conroy A, North K, Patterson J, Bose C, Meshnick S (2019) An overview of malaria in pregnancy. Semin Perinatol 43(5):282–290
Onyemaechi N, Malann Y (2020) Malaria prevalence investigtion among pregnant women in Relation to their social well being: a case study of Lugbe and Gosa, Abuja, Nigeria. Int J Pathogen Res 4(2):7–15
Yaro J, Ouedraogo A, Diarra A, Sombie S, Ouedraogo Z, Nebie I et al (2021) Risk factors for Plasmodium falciparum infection in pregnant women in Burkina Faso: a community-based cross-sectional survey. Malar J 20:362
World Health Organization (2019) World Malaria Report 2019 at Glance. [Internet]. Geneva; Available from https://www.who.int/news-room/feature-stories/detail/_world-malaria-report-2019
World Health Organization (2020) World Malaria report (2020): 20 years of global progress and challenges. [Internet]. Geneva. Available from https://apps.whoo.int/iris/handle/10665/_337660
Sato S (2021) Plasmodium-a brief introduction to the parasites causing human malaria and their basic biology. J Physiol Anthropol 40(1):3
Kwale K, Asika A, Adiel T (2021) Prevalence of Malaria infection among pregnant women Attending specialist Hospital Yola, Adamawa State, Nigeria. South Asian J Parasitol 4(2):65–72
Balcha F, Menna T, Lombamo F (2023) Prevalence of asymptomatic malaria and associated factors among pregnant women at Boset District in East Shoa Zone, Oromia Region, Ethiopia: a cross-sectional study. Malar J 22:28
Venugopal K, Hentzschel F, Valkiunas G, Marti M (2020) Plasmodium asexual growth and sexual development in haematopoietic niche of the host. Nat Rev Microbiol 18:177–189
Galinski M (2022) Systems biology of malaria explored with non human primates. Malar J 21:177
Walker I, Rogerson S (2023) Pathogenicity and virulence of Malaria; sticky problems and triky solutions. Virulence 14(1):2150456
Ellwanger J, Cardoso JC, Chies J (2021) Variability in Human attractiveness to mosquitoes. Curr Res Parasitol Vector Borne Dis 1:100058
Chau C, Ming-khoo S, Ernest-Ong J, Ramireddi G, Yeo T, Teo A (2021) Malaria in pregnancy: from placental infection to its abnormal development and damage. Front Microbiol 12:777343
Chau C, Hasang W, Rogerson S, Andrew T (2021) Poor birth outcomes in malaria in pregnancy: recent insights into mechanisms and prevention approaches. Front Immunol 12:621382
Foghi B, Nduka F, Nzeako S (2021) Effect of Malaria on some hematological parameters among pregnant women in Delta State, Nigeria. Int J Trop Dis Health 42(16):21–29
Nlinwe N, Nange T (2020) Assessment of hematological parameters in malaria, among adults’ patients. Attending the Bamenda Regional Hospital. Anemia 2020:3814513
Obed A, Aminu M, Abdullahi U (2021) Malaria parasite infection and its Effect on Packed cell volume among pregnant women in Zaria, Nigeria. Int J Trop Dis. https://doi.org/10.23937/2643-461X/1710055
Oyerogba O, Adedapo A, Awokson T, Odukogbe A, Aderinto N (2023) Prevalence of malaria parasitaemia among pregnant women at booking in Nigeria. Health Sci Rep 6(6):e1337
Bakken L, Iversen P (2021) The impact of malaria during pregnancy on low birth weight in East-Africa; a tropical review. Malar J 20:348
Isa H, Bashir M, Adedeji B (2022) Malaria prevalence and anemia status of children attending a healthy facility in Yola. J Adv Microbiol 22(8):25–31
Charan J, Biswas T (2013) How to calculate sample size for different study designs in medical research. Indian J Psychol Med 35(2):121–126
Cheesbrough M (2010) District laboratory practice in tropical countries. In: Examination of malaria parasites, 2nd ed. Cambridge University Press, Cambridge, pp 195–216
Hoffbrand A, Higgs D, Keeling D, Mehta A (2011) Postgraduate haematology, 7th edn. John Wiley, London
vanAssendelft O, Bull B, Koepke J, Simson E (1993) Procedure for determination of packed cell volume by the microhematocrit method, 2nd ed. Vol. 13. NCCLS Document H7-A2
IBM Corp (2011) IBM SPSS Statistics for windows. Armonk, NY: IBM Corp.
Bolaji O, Adekunle O, Adeyemo A, Ojewuyi A, Ajayi A, Rufai A, et al (2023) Prevalence of Plasmodium falciparium among pregnant women attending antenatal clinics in Osogbo, Osun State Nigeria. Western Nigeria J Med Sci 6(1):23–28
Yusuf F, Sadau Y, Natasha P, Lai I (2023) Effects of Malaria Parasitemia on Hematological Parameters of Pregnant Women Attending Gombe Specialist Hospital. Bima J Sci Technol 7(1):397
Lawal S, Ahmed A, Lawal U (2023) Prevalence and risk factors associated with malaria among pregnant women attending selected public health facilities within Kastina metropolis, Kastina State Nigeria. UMYU J Microbiol Res 8(2):8–14
Simon-Oke I, Ogunseem M, Afolabi O, Awosolu O (2019) Prevalence of malaria parasites among pregnant women and children under five years in ekiti State, southwest Nigeria. J Biomed Transl Res 5(1):5–10
Okolo M, Adeshina K, Omotola C, Mudi I, Ugbane E (2023) Prevalence of Malaria and Typhoid Fever co-infection among pregnant women attending antenatal clinician Anyigba Kogi State, Nigeria. Microbes Infect Dis 4(2):671–680
Okoroiwu GA (2023) Prevalence of malaria and associated risk factors in pregnant women in mbaitoli local government area, South-east Nigeria. Afr J Biomed Res 26:167–172
Umar S, Erhabor O, Abdulrahaman Y, Zama I, Onuigwe F, Buhari H et al (2022) Alterations in some hematological parameters, ascorbic acid and pantothenic acid levels among pregnant women with plasmodium parasitaemia in Sokoto, Nigeria. Sokoto J Lab Sci 7(3):71–84
Mangusho C, Mwebesa E, Izudi J, Aleni M, Driclle R, Ayaiasi R et al (2023) High prevalence of malaria in pregnancy among women attending antenatal care at a large referral hospital in Northwestern Uganda: a cross-sectional study. PLoS ONE 18(4):e0283755
Oladimeji K, Tsoka-Gwegweni J, Anyiam F, Yaya S, Nutor J, Abiodun G et al (2023) Socio-economic predictors of uptake of malaria interventions among pregnant women and mothers of under 5 children in Oyo State, Nigeria: a cross-sectional study. Pan Afr Med J 44:65
Yimam Y, Nateghpour M, Mohebali M, Abbaszadeh-Afshar M (2020) Asystematic review and meta-analysis of asymptomatic malaria infection in pregnant women in sub-saharan Africa: A challenge for malaria elimination. PLoS ONE 16(4):e0248245
Mlugu E, Minzi O, Kamuhabwa A, Aklillu E (2020) Prevalence and correlates of asymptomatic malaria and anemia on first antenatal care visit among pregnant women in Southeast, Tanzania. Int J Environ Res Public Health 17(9):17093123
Olukosi A, Olakiigbe A, Ajibaye O, Orok B, Aina O, Akindele S et al (2020) Socio-economic behavioural indicators of falciparum malaria parasitaemia and moderate to severe anaemia among pregnant women attending antenatal clinics in Lagos, Southwestern Nigeria. Malaria J 19:393
Suliman M, Tamomh A, Younis O, Magboul A, Mohammed H, Hassan I et al (2021) Malaria infection and associated risk factors in pregnant women attending antenatal clinics in AI Jabalian locality, White Nile state Sudan. Ann Parasitol 67(3):499–504
Kiemde F, Sorgho H, Zango S, Some G, Rouamba T, Traore O et al (2023) Immunomodulatory effect of gestational age on blood cortisol and prolactin levels during pregnancy in malaria endemic area. Res Square 1:1–18
Angraini D (2023) Role of nutrient intake and social determinat in Anemia among pregnant women at Lampung Malaria Endemic Areas. Rev Primary Care Pract Educ 6(1):28–34
Abbas M, Jibril A, Nuhu A (2021) Assessment of some haematological parameters in pregnant women with malaria attending Murtala Muhammad Specialist Hospital. Kano Bayero J Sci 6(1):754–760
Saleh B, Lugaaajju A, Storry J, Persson K (2023) Autoantibodies against red blood cell antigens are blood cell antigens are common in malaria endemic area. Microbe Infect 25(3):105060
White N (2018) Anaemia and malaria. Malar J 17:371
Ndamukong-Nyanga L, Miangu-Wolloh G, Yunga N, Jacqueline N, Ndamukong N (2020) Malaria Parasitaemia and variations in Haematological parameters among pregnant women in Buea. Int J Pathogen Res 4(3):8–16
Binuyo O, Galadima M, Rowaiye A, Iseghohi F (2022) Effect of malaria infections on the Hematologic and Anthropometric indices of pregnant women in six villages in Northern Nigeria. Int J Dent Med Sci Res 4(4):106–116
Erhabor O, Abdullahi A, Tosan E (2019) Effects malaria parasitaemia on some Haematological parameters of pregnant women of African Descent in specialist Hospital Sokoto, Northwestern Nigeria. JOJ Nurse Health Care 10(4):555795
van-Wolfswinkel M, Langenberg M, Wammes L, Sauerwein R, Koelewijin R, Hermsen C, et al (2017) Changes in total and differential leukocyte counts during the clinically silent liver phase in a controlled human malaria infection in malaria-native Dutch volunteers. Malaria J 16:457
Ogbodo E, Ezeugwunne I, Eze B, Njoku C, Oguaka V, Amah A et al (2018) The effect of malaria infection on some hematological parameters of pregnant women in Nnewi Anambra state Nigeria. Int J Dev Res 8(10):23353–23358
WorldWide Antimalaria Resistance Network White Blood Cell Count in Malaria Study Group (2023) Variability in white blood cell count during uncoomplicated malaria and implications for parasite density estimation: a worldwide Antimalarial resistance network individual patient data met-analysis. Malaria J 22:174
Obebe O, Falohun O, Olajuyigbe O, Lawani M, Ajayi A (2018) Impact of asymptomatic Plasmodium falciparium on hematological parameters of pregnant women at first antenatal visit in South-western, Nigeria. Tanzan J Health Res 20(2):4
Pinedo-Cancino V, Arista K, Valle-Campos A, Saavedra-Langer R, Roca C, Ramos-Rincon J et al (2022) Hematological profile s of malaria infected patients in an endemic area of Peru. Rev Peruana Med Exp Salud Publ 39(3):11908
Dockree S, Shine B, Pavord S, Impey L, Vatish M (2021) White blood cells in pregnancy: reference intervals for before and after delivery. EBioMedicine 74:103715
Adamu J, Jigam A (2019) Effects of Malaria infection on some hematological and boichemical parameters in General population and pregnant malaria patients attending two District Hospitals in Niger State, Nigeria. Glob J Infect Dis Clin Res 5(1):001–005
Djimde M, Kayentao K, Arama C, Dicko A, Mens P, Henk-Schallig H (2023) Neutrophils and pregnancy associated malaria. Res Square 68:7–115
Bert S, Ward E, Nadkarni S (2021) Neutrophils in pregnancy: new insights into innate and adaptive immune regulation. Immunology 164(4):665–676
Jesenak M, Diamant Z, Simon D, Tufvesson E, Seys S, Mukherjee M, et al (2023) Eosinophils-from cradle to grave. Allergy. https://doi.org/10.1111/all.15884
Gigon L, Fettrelet T, Yousefi S, Simon D, Simon H (2023) Eosinophils from A to Z. Allergy 78(7):1810–1846
Scheunemann J, Reichwald J, Korir P, Kuehlwein J, Jenster L, Hammerschmidt-Kamper C et al (2021) Eosinophils Suppress the migration of T-cells into the brain plasmodium berghei-infected Ifnar1 mice and protect them from experimental cerebral malaria. Front Immunol. https://doi.org/10.3389/fimmu.2021.711876
Frimpong A, Amponsah J, Adjokatseh A, Agyemang D, Bentum-Ennin L, Ofori E et al (2020) Asympyomatic malaria infection is maintained by a balance pro-and anti-inflammatory response. Front Microbiol 11:559255
Garba I, Umar A, Tijjani M, Aliyu M, Muhammad H, Raji M et al (2023) Haematological changes in malaria infection among pregnant women in Sokoto Metropolis Nigeria. FUDMA J Sci 7(3):1870
Dobbs K, Crabtree J, Dent A (2021) Innate immunity to malaria, the role of monocytes. Immunol Rev 293(1):8–24
Ejike B, Ukpai O, Ihemanma C, Ajuga M, Eme G (2022) Impact of malaria infection on the haematological profile of pregnant women in south-eastern Nigeria. Nigeria J Parasitol 43(1):78–84
Okamgba O, Ifeanyichukwu M, Ilesanmi A, Chigbu L (2022) Variations in the leikocyte and cytokine profiles between placental and maternal circulation in pregnancy associated malaria. Res Rep Trop Med 9:1–8
Ourives S, Borges Q, Damazo A (2018) Analysis of the lymphocyte cell population during malaria caused by plasmodium vivax and its correlation with parasitaemia and thrombocytopaenia. Malar J 17:303
Stephane P, Diop S, Badiane M, Vitte J, Beguin P, Nato F et al (2012) enhanced basophil reactivities during severe malaria and their relationship with the Plasmodium falciparium histamine-releasing factor translationally controlled tumor protein. Infect Immun 80(8):2963–2970
Porcherie A, Peronet R, Schneider E, Claver J, Commere P, Kiefer-Biasizzo H et al (2011) Critical role of neutrophil-associated high affinity receptor for IgE in the pathogenesis of experimental cerebal. J Exp Med 208(11):2225–2236
Ifeanyi O (2019) An update on impact of malaria in pregnancy on Hematological parameters. Int J Med Sci Dent Res 2(1):37–39
Acknowledgements
The authors thank the management of the Specialist Hospital Yola, Nigeria, for granting the necessary approvals that enabled the success of this study. The enormous support of the trained medical personnel (nurses) who helped in the collection of samples is highly acknowledged. In addition, the participation of all the pregnant women that availed themselves in this study is gratefully appreciated.
Author information
Authors and Affiliations
Contributions
Blessing Nkechi Emmanuel: Conceptualization, Data collection, samples analysis, Methodology, Writing-original draft preparation, Writing-reviewing and editing. Godly Chessed: Conceptualization, Writing-reviewing and editing, Supervision. Jerry Chima Ekeuhie: Conceptualization, Data collection, Data collection, samples analysis. Frank Efe Erukainure: Writing original draft preparation, Writing-reviewing and editing. Vandi Philips: Conceptualization, Writing-reviewing and editing, Supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval
The study was conducted following the Declaration of Helsinki. All the experimental protocols used for this study were approved by the Institutional Reviews Board and the Ethical Committee of the Specialist Hospital, Yola, Adamawa State, Nigeria (Ref. ID: ADS/SHY/301/VOL.II), where the study was carried out. Furthermore, informed consent was obtained from all study subjects who participated in this study. Also, the voluntary participation of the study subject was respected.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Emmanuel, B.N., Chessed, G., Erukainure, F.E. et al. Prevalence of malaria parasite and its effects on some hematological parameters amongst pregnant women in Yola, Nigeria. J.Umm Al-Qura Univ. Appll. Sci. 10, 200–210 (2024). https://doi.org/10.1007/s43994-023-00092-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43994-023-00092-z