Abstract
Curbing infectious diseases has been a significant challenge worldwide, with existing conventional surveillance systems presenting gaps in providing timely and spatial information, which undermines prevention and control. This has propelled the use of Wastewater-Based surveillance (WBS), a valuable tool for infectious disease surveillance able to detect early infectious diseases among asymptomatic, pre-symptomatic, symptomatic, and post-symptomatic individuals. Despite the global attention and the contribution of WBS in monitoring the COVID-19 pandemic, its use in the African continent is still stunted, which may hamper the early detection, monitoring, prevention, and response to outbreaks. Africa can benefit from WBS, deemed to be quick, cost-effective, providing timely data to ensure early report of the presence of a high-consequence infectious pathogen and devise timely protective measures at a population-level perspective. In addition, considering its inclusivity in providing an overall burden of infectious agents representing the population even in areas with limited resources, wastewater surveillance is important in tackling health disparities. Therefore, it is crucial to overcome challenges related to implementing surveillance in Africa. This can be achieved by providing adequate investments for surveillance efforts, establishing modern infrastructure to enhance wastewater drainage, enhancing the healthcare workforce through training, improving healthcare infrastructure and equipment, and utilising digital health solutions. Collaborative efforts on both local and global scales are crucial for developing effective health policies, and a robust research capacity within the continent is crucial.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Infectious diseases remain a significant global public health challenge that impacts communities and individuals. This challenge has been persistent throughout human history, causing approximately 15 million deaths annually, with a disproportionate burden among low- and middle-income countries [1]. In addition, the burden of infectious diseases weighs much more on vulnerable populations, people living in precarious conditions or stigmatised communities [2, 3], thus compounding health inequities.
Pathogens causing infectious diseases evolve and adapt to new environments, resulting in new strains and variations of infectious diseases. The evolution and emergence of infectious diseases are complex and adheres to dynamic processes [4]. These processes can be influenced by a range of factors, including changes in human behaviour, demographic shifts, urbanisation, globalisation, and environmental changes [5]. The dynamic nature of infectious diseases means that effective control and prevention strategies are also evolving. For example, the global response to the spread of the human immunodeficiency virus (HIV) has changed significantly over the past few decades, from the initial phase of confusion and denial to the current phase of increased knowledge, prevention strategies, and access to antiretroviral therapy (ART) and pre-exposure prophylaxis (PrEP) [6].
The global response to infectious diseases is also influenced by the political, economic, and social context in which they occur, making the response effective or ineffective as seen during the Ebola crisis in West Africa in 2014 and the 2003 severe acute respiratory syndrome (SARS) outbreak. Whereas the detection and response to the former were slow and inadequate [7], the response to the latter was deemed rapid and effective, partly due to strong healthcare systems and effective public health measures implemented by affected countries [8].
Effective control and prevention strategies require a dynamic and adaptive global response that can respond to the changing nature of infectious diseases. This features the importance of early and innovative approaches to infectious disease surveillance, such as wastewater-based surveillance (WBS). WBS leverages the vast amounts of data generated by wastewater treatment facilities, providing real-time, population-level data that document early warning signs of the spread and presence of infectious diseases within a community [9]. This indicates that the use of WBS as one of the infectious diseases surveillance methods is crucial and effective in response to outbreaks.
In Africa, the burden of infectious diseases is high, with many countries facing significant challenges in terms of disease control and prevention. This has been evidenced in the World Health Organization (WHO) Africa data indicating that infectious diseases were responsible for 36% of disability-adjusted life years (DALY) in 2015 [10]. Early detection of infectious diseases is, therefore, crucial to monitor and provide warnings that can prompt timely actions, underlying the need to strengthen early warning systems such as WBS [9]. Despite WBS’s capacity to minimise the impact of infectious disease outbreaks on the community, there is a significant gap in the utilisation of WBS and availability of its data in Africa [11], demonstrating a need for further research highlighting its importance on the continent. This article elucidates the infectious diseases surveillance system in Africa and the expanding roles of waste-water surveillance in optimising infectious diseases surveillance in the continent.
2 Infectious disease surveillance systems in Africa
Establishing a strong surveillance system is essential to mitigating infectious disease outbreaks. Effective infection prevention and control requires an infectious surveillance system that can timely detect and monitor infection outbreaks, thus providing an appropriate response via the implementation of protective policies. As Africa has recorded a significant number of infectious diseases, countries on the continent have implemented various infectious diseases surveillance systems to prevent further spread of the diseases. Some of the existing surveillance methods on the continent are described below:
2.1 Disease reporting and notification
African countries have adopted disease reporting and notification surveillance systems in order to curb infectious diseases [12]. Disease reporting and notification enables a swift response to infectious diseases, thereby preventing the disease’s transmission. Reporting is typically done by frontline healthcare professionals or laboratories upon identifying an infectious disease outbreak. This method of surveillance is a legal requirement in African countries. Taking the example of South Africa, there is legislation obliging healthcare workers to promptly report suspected or confirmed emerging and re-emerging communicable diseases to prevent and monitor the trends of the disease [12]. Thus, a successful disease reporting system will depend largely on healthcare providers who are knowledgeable in the process of identification and reporting of outbreaks.
2.2 Integrated disease surveillance and response (IDSR)
The Integrated Disease Surveillance and Response (IDSR) strategy aims to integrate comprehensive surveillance, laboratory diagnostics and response mechanisms to diseases at all health systems levels. In the WHO African Region, around 94% of countries had embraced the IDSR strategy by 2017. However, despite this progress, certain obstacles persist. These include issues like incomplete and inconsistent data reporting, which undermines the IDSR strategy’s capacity to effectively facilitate evidence-based decision-making [13, 14].
2.3 Sentinel surveillance
Sentinel surveillance system involves selecting a single or few health facilities that will be saddled with the responsibility of gathering and reporting data on daily cases. In Madagascar, this form of surveillance has been deployed in reporting incidence cases including malaria, dengue, and influenza diseases [15]. It also provides valuable epidemiological data on distributions based on different disease agents, risk factors and age distribution. Whereas sentinel surveillance systems help to bolster shortcomings of surveillance by regulating and controlling an area’s crisis more intentionally, global data highlights the inconsistency in the information provided by the system, which impedes effective control measures [16].
2.4 Syndromic surveillance
Syndromic surveillance is a prevalent practice in resource-limited settings, where it detects symptoms that serve as early warning signals. This proactive approach involves health authorities, backed by computer-generated data and statistical analysis. It enables the swift identification and control of disease indicators in a timely and predictive manner, facilitating the early discovery of disease outbreaks [17]. Syndromic surveillance systems provide a timely signal for health incidence by trailing symptoms before confirmation by clinical and laboratory diagnosis. This surveillance system was used in countries such as Rwanda, Liberia, Lesotho, Malawi, Sierra Leone, Haiti, and Mexico for COVID-19 surveillance monitoring [17]. Rwanda demonstrated favourable results in the response to COVID-19 through the utilization of Syndromic Surveillance. This approach enabled Rwanda to achieve the herd immunity threshold as defined by the WHO [18]. While this system can detect a big health issue in a population, it has limited capacity to detect new emerging infectious diseases, thus missing new pathogens [19].
2.5 Laboratory capacity and innovative technologies
The capacity and infrastructure of laboratories must be improved for accurate and prompt detection of infectious diseases. This entails setting up properly equipped laboratories, educating laboratory staff, and ensuring that diagnostic equipment and reagents are available as stipulated in the 2008 Maputo Declaration on strengthening laboratory services [20]. Leveraging innovative technologies such as genomics and the use of digital health can enable robust laboratory capacity while improving and strengthening health systems ability to tackle infectious diseases via better prevention and control. Testing problems are not only limited to a paucity of equipment but are also linked to ethical challenges such as ethical approval by competent institutions and consent from participants [19].
2.6 Community capacity building and engagement
A better health system ensures that local people are at the centre of response preparedness and strategies for diseases [21]. Engaging and equipping the community with necessary skills regarding outbreaks and providing information useful for response has played an important role in community protection as was reported during the Ebola outbreak [21]. As such, community members are key players in raising awareness among their community. Thus, empowering them to report any unusual health event and promote health intervention is essential.
2.7 One health approach
The interconnection between human health, veterinary, and the environmental sector is a critical component of infectious disease surveillance in Africa. Combined efforts that consider dimensions such as human health, animal health, and the environment can improve surveillance and response to infection. This is critical because many risk factors of infection are connected not only to humans but also to animals and the environment. Notably, recent studies indicate that 60–75% of human infectious diseases are transmitted from wild animals to humans, a transmission called “zoonotic spillover” [22], highlighting the need for one health approach in tackling infectious diseases as advised by CDC Africa. The strengths and limitations of above-mentioned approaches are described in Table 1. Therefore, exploring the environment can be paramount in providing an early warning that can predict the disease before its occurrence in communities such as Wastewater-Based Surveillance. The next section explores the utmost importance of Wastewater-Based Surveillance in Africa.
3 The need for adoption and the strengths of wastewater-based surveillance systems in Africa
The recent COVID-19 pandemic emphasized the importance of an early surveillance system for halting the spread of the pandemic and mitigating its effects. It did, however, reveal a slew of significant flaws in the conventional surveillance system (Table 1), primarily based on clinical and laboratory testing, including high costs, missing asymptomatic cases, late detection of infection after it has dispersed throughout the community, reporting delays due to stigma and limited access to healthcare, and, ultimately, widespread infection before health authorities are informed, as well as an underestimation of infection prevalence [19]. Furthermore, conventional surveillance is constrained due to its inability to effectively capture zoonotic transmission and detect emerging pathogens [19]. These pose challenges in healthcare settings with limited resources such as African countries, among others. The limit of conventional or traditional surveillance illustrates the need for surveillance systems, such as WBS, that have the potential to address the aforementioned limitations and has the opportunity to be a feasible and effective surveillance system for current and forthcoming communicable diseases [11]. The strengths of WBS are summarised in Table 1.
Wastewater testing was first introduced in the nineteenth century when cholera epidemics caused staggering deaths in London. In order to better understand the cause of the outbreaks, Dr. John Snow examined water and sewage systems in 1854 and reported that the contaminated water was the cause of cholera epidemics in England [23]. The term “wastewater” is generally used to describe the end product of all types of water usage, including stormwater, sewage from homes, industrial, commercial, and agricultural activities [19]. By analyzing wastewater, public health authorities can identify outbreak hotspots in real time and space, monitor for emergencies and the spread of variants, forecast surges and trends in a municipality, province, or region, and then implement public health response measures [24]. COVID-19 demonstrated that wastewater surveillance can detect a new pathogen outbreak. Having found that COVID-19 sheds RNA fragments in faeces, wastewater surveillance programs targeting the virus and its known variants have gained attention worldwide, thus increasing the use of wastewater data for population-level screening as an additional and effective monitoring technique [25]. When implemented in Africa, WBS has provided both early and cost-effective data to enhance clinical surveillance systems [11].
Wastewater analysis has the potential to uncover a range of diseases and other pollutants, including pharmaceuticals, hormones, and illegal drugs, which can give an understanding of the health status of communities [24]. Several pathogens, which due to their potential to cause sudden and significant harm necessitates rigorous and thorough preparedness measures [26]. Wastewater testing can thus efficiently evaluate the multiple health markers of these pathogens, thereby making it a leading indicator in detecting pathogens prior to reporting infection cases, which is essential for early intervention strategies [26].
Moreover, monitoring wastewater is an essential environmental and public health surveillance component. Due to growing concerns about water-borne infections and environmental destruction, the use of WBS has increased in Africa in recent years. In Africa, wastewater surveillance was first put into place in Nigeria in 2011 for poliovirus tracing. Since then, other African nations have used this system as an additional tool in the fight to eradicate polio [27]. In addition, wastewater tests contributed to assessing the presence of Aichi virus (AiV) and human bocavirus (HBoV) and showed possible virus implications in diarrheal diseases in Egypt [28]. The equally important use of WBS was unveiled in its capacity to screen Noroviruses (NoVs), particularly in characterising 16 NoV genotypes in Free State and Gauteng, in South Africa [29]. Documenting the prevalence and diversity of these virological pathogens has been critical in informing health policy to enact intervention strategies and make data-driven decisions, which is essential in curbing infectious diseases in Africa.
African countries have made significant strides in comprehending the diversity of viruses in wastewater. A study conducted in Uganda to understand the viral density in surface and wastewater identified a prevalence of hepatitis, adenovirus, rotavirus, and enterovirus [30]. This emphasises the critical importance of monitoring viral concentrations in wastewater to provide accurate data on the prevalence and trends of waterborne viruses at a population level. In addition, through the analysis of wastewater in Nigeria, it became possible to identify specific characteristics and intra-genotype diversity within rotaviruses. This knowledge is essential for improving the prevention and control strategies for these diseases [31]. Furthermore, comparing the detection of enteroviruses (EV) in sewage has shown differences in the direct detection of EV strains, with samples from Pakistan and Senegal presenting a significant number of strains than the United Kingdom [32]. This surveillance strategy has also been successfully deployed in Tunisia by detecting and genotyping group A rotaviruses, emphasizing the need to monitor wastewater to add to existing surveillance systems for this infection [33]. Other studies have demonstrated the feasibility of using wastewater samples to routinely monitor noroviruses (NoVs) within the African continent, indicating that monitoring sewage can be beneficial in detecting the presence of different NoV strains in the wider community [29, 33, 34].
The crucial importance of WBS is beyond disease detection. It has been applied to document antibiotic resistance in some African countries. Antibiotic resistance is a health issue that is difficult to manage, resulting in mortality, long hospitalisation, and high costs that can lead people into significant poverty [35]. To mitigate inadequate antimicrobial surveillance in Africa, WBS is a critical component for the early detection of drug resistance. For instance, a study conducted in South Africa to determine drug-resistant tuberculosis (DR-TB) in treated and untreated wastewater showed that resistance to primary and alternative TB treatment drugs was more prevalent in untreated wastewater [36]. In Kenya, the practice of analysing wastewater has been employed to determine the presence of antibiotics within communities, with results indicating elevated levels of antibiotics in sewage sludge. This suggests that adsorption may play a significant role in removing these compounds from wastewater treatment plants [37]. This raises concerns about using sewage sludge and treated wastewater in agriculture, as antibiotics could enter the food chain through plant uptake. It is, therefore, imperative to enhance wastewater treatment methods to reduce the discharge of antibiotics into surface waters, sewage sludge, and soil [37].
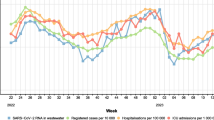
In another context WBS served as a viable early warning system for outbreaks and the emergence of clinical infections. For instance, SARS-CoV-2 viral RNA was found in USA wastewater before the onset of symptoms and clinical diagnosis, with its titers being positively correlated with the number of subsequent clinical cases reported [38]. WBS was also conducted in South Africa to detect and monitor COVID-19. Wastewater testing revealed variations in viral load between two distinct time periods [39]. This study has highlighted the importance of WBS in providing real data in real-time and space. It anticipated new infection flare-ups during holidays and social gatherings [39], allowing health authorities to allocate the necessary resources and the public to take the necessary precautions.
WBS provides a cost-effective surveillance system for low-income countries in Africa. Employing WBS in a single wastewater treatment unit in the same country could provide coverage for approximately 15,000 people at a much lower cost [40]. Additionally, WBS could also be utilized in tracking disease spread and determining whether it is contained, as well as the effectiveness of public health measures such as contact tracing and lockdown. In New Zealand, the negative wastewater analysis results ruled out the spread of the infection in the community, indicating the containing of the COVID-19 pandemic as a result of effective protective measures and contact tracing, leading the country to lift the lockdown [41]. This demonstrates that WBS is important in forming decision-makers not only to implement but also to lift protective measures when appropriate.
WBS systems can be beneficial and complementary to conventional infectious disease surveillance. Therefore, it is crucial for African health systems to prioritise the widespread adoption of this approach and to tackle the challenges linked to its implementation.
4 Addressing limitations, challenges and a way forward for WBS in Africa
Despite its apparent advantages, several factors have presented significant challenges to the successful implementation of Wastewater-Based Surveillance (WBS) in Africa. Chief among these is the constraint of limited resources, leading to notable gaps in its widespread adoption [11]. Addressing this issue necessitates strategic allocation and investment in workforce training, equipment procurement, and infrastructure development. These crucial steps are essential for establishing and maintaining effective wastewater analysis systems, particularly in the context of numerous African countries whose wastewater treatment facilities remain outdated and inadequately equipped, resulting in suboptimal wastewater treatment [42].
Technological challenges linked to ineffectual treatment processes such as dilution effects, unmeasured flows, modelling issues of wastewater systems compounded by a lack of technical capacity further complicates the challenge of integrating WBS comprehensively throughout the continent, underscoring the critical necessity of reinforcing health systems in Africa, profoundly impacted by the repercussions of the COVID-19 pandemic [43]. Thus, the imperative to fortify the workforce and enhance WBS becomes evident, as it underscores the importance of employing accurate wastewater analysis techniques capable of yielding evidence that guides targeted public health interventions. A proactive approach entails devising robust programs within African health systems, supported by resilient infrastructure, and promoting the utilization of wastewater surveillance as a preemptive tool to monitor the prevalence of infectious diseases both prior to and during outbreaks. This ambitious goal mandates collaborative efforts between governments, as well as local, regional, and global partners, collectively investing in bolstering health systems.
Furthermore, the design of Polymerase Chain Reaction (PCR) assays for detecting viruses in wastewater must take into account the potential for cross-reactivity with live virus-based vaccines used in mass vaccination initiatives. Additionally, the selection of an appropriate biomarker for a given infectious disease presents a multifaceted challenge. A biomarker must exhibit specificity to human metabolism to exclude non-human sources. Furthermore, it should demonstrate stability throughout the wastewater handling, extraction, storage, and analysis processes [44]. Prioritising the early identification of a biomarker that aligns with these criteria is paramount for effectively harnessing Wastewater-Based Epidemiology (WBE) as an early warning system for the containment of emerging infections.
An additional pressing concern pertains to the dearth of wastewater treatment facilities in rural regions across many African nations. Open defecation remains prevalent, due to the absence of basic sanitation amenities in over 30% of sub-Saharan African countries [45]. The practice of disposing wastewater in open drains or spaces poses a challenge to representative sample collection, as it skews results due to the absence of residents in the sampling pool. Addressing this issue underscores the urgency of modernising urban infrastructure in African cities to incorporate advanced wastewater drainage systems capable of accommodating larger population samples. In the interim, leveraging wastewater from public spaces such as schools, markets, and places of worship can serve as a valuable alternative.
Applying WBS within community contexts necessitates acknowledging ethical considerations surrounding privacy, data sharing, and potential stigmatisation [46]. Consequently, community engagement becomes pivotal, ensuring that surveillance efforts are culturally sensitive. Employing privacy-enhancing technologies like beacons, access control measures, differential privacy techniques, cryptography, and blockchain can effectively safeguard confidentiality while facilitating the responsible implementation of Wastewater-Based Surveillance.
5 Conclusion
In summary, this article underscores the crucial role of wastewater-based surveillance (WBS) as a complementary tool to conventional infectious disease surveillance systems, with a specific emphasis on its significance for Africa. Wastewater-based surveillance offers a novel approach to detecting infectious diseases by analysing samples from wastewater sources. This method proves invaluable in identifying diseases and providing early warnings for infections or outbreaks within communities, even among those who might be asymptomatic or pre-symptomatic.
The adoption of wastewater-based surveillance allows for a comprehensive global and population-level perspective on infectious diseases. The data collected through this approach holds substantial value for health policymakers, aiding in the development of effective public health interventions on a global scale. Notably, wastewater-based surveillance facilitates the detection of infections among individuals who might lack access to conventional healthcare facilities, thereby promoting a more equitable distribution of disease testing and healthcare resources.
Furthermore, wastewater-based surveillance enables the real-time monitoring of pathogen concentration trends and the swift identification of emerging hotspots. This function plays a pivotal role in evaluating the efficacy of disease control measures and supports the targeted deployment of interventions.
However, despite the promising benefits, the implementation of wastewater surveillance systems in Africa faces formidable challenges. Weak healthcare systems, inadequate funding, and a lack of modern infrastructure, including proper wastewater drainage systems, pose significant barriers to the successful integration of this surveillance method in many sub-Saharan African regions.
To fully harness the potential advantages of wastewater-based surveillance, Africa must prioritise the strengthening of its healthcare systems and investment in the requisite infrastructure. Improving infrastructure, specifically by creating effective wastewater drainage systems, will play a vital role in supporting the successful planning and implementation of wastewater surveillance efforts, leading to overall better living conditions.
Evidently, a collaborative and concerted global effort is imperative to support the seamless implementation, vigilant monitoring, and ethical application of wastewater-based surveillance systems. By collectively addressing these challenges, the international community can effectively leverage this innovative approach to bolster infectious disease surveillance and response capabilities, ultimately leading to enhanced public health outcomes.
Data availability
Not applicable.
References
WHO. Infectious diseases. World Health Organization. 2019. https://www.who.int/health-topics/infectious-diseases#tab=tab_1. Accessed 25 July 2023.
Manirambona E, Wilkins L, Lucero-Prisno DE III. COVID-19 and its threat to refugees in Africa. Health Promot Perspect. 2021;11(3):263–6. https://doi.org/10.34172/hpp.2021.33.
Manirambona E, Shomuyiwa DO, Musa SS, Lucero-Prisno DE III. Monkeypox among men who have sex with men in Africa: the need for testing and vaccination beyond stigma. J Med Virol. 2023;95(1): e28121. https://doi.org/10.1002/jmv.28121.
Molloy S. Disentangling syntrophy. Nat Rev Microbiol. 2014;12(1):7–7.
Ragonnet-Cronin M, Nagle A, Dominguez AL, Bibi Y, Ochola R. Emergence and evolution of infectious diseases: the role of human activities and societal changes. EcoHealth. 2018;15(1):5–16.
Piot P. The global response to HIV/AIDS: 30 years of lessons learned. Lancet. 2010;376(9738):801–9.
WHO Ebola Response Team, Agua-Agum J, Ariyarajah A, Aylward B, Blake IM, Brennan R, Cori A, et al. West African Ebola epidemic after one year–slowing but not yet under control. N Engl J Med. 2015;372(6):584–7. https://doi.org/10.1056/NEJMc1414992.
Leung NH, Au KW, Ho PL, Chan KF, Cheng VC, Tsang DN, Peiris JS. Clinical features, diagnosis and management of severe acute respiratory syndrome. Lancet. 2003;361(9368):1701–7.
National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Division on Earth and Life Studies; Board on Population Health and Public Health Practice; Water Science and Technology Board; Committee on Community Wastewater-based Infectious Disease Surveillance. Wastewater-based Disease Surveillance for Public Health Action. Washington (DC): National Academies Press; 2023. 1, Introduction. https://www.ncbi.nlm.nih.gov/books/NBK591714/.
A heavy burden: the productivity cost of illness in Africa. Brazzaville: WHO Regional Office for Africa; 2019. Licence: CC BY-NC-SA 3.0 IGO.
Dzinamarira T, Murewanhema G, Iradukunda PG, Madziva R, Herrera H, Cuadros DF, Tungwarara N, Chitungo I, Musuka G. Utilization of SARS-CoV-2 wastewater surveillance in Africa—a rapid review. Int J Environ Res Public Health. 2022;19(2):969. https://doi.org/10.3390/ijerph19020969.
Benson FG, Levin J, Rispel LC. Health care providers’ compliance with the notifiable diseases surveillance system in South Africa. PLoS ONE. 2018;13(4): e0195194. https://doi.org/10.1371/journal.pone.0195194.
Fall IS, Rajatonirina S, Yahaya AA, et al. Integrated disease surveillance and response (IDSR) strategy: current status, challenges and perspectives for the future in Africa. BMJ Glob Health. 2019;4: e001427.
Mremi IR, George J, Rumisha SF, Sindato C, Kimera SI, Mboera LEG. Twenty years of integrated disease surveillance and response in sub-Saharan Africa: challenges and opportunities for effective management of infectious disease epidemics. One Health Outlook. 2021;3(1):22. https://doi.org/10.1186/s42522-021-00052-9.
Randrianasolo L, Raoelina Y, Ratsitorahina M, Ravolomanana L, Andriamandimby S, Heraud JM, et al. Sentinel surveillance system for early outbreak detection in Madagascar. BMC Public Health. 2010;10:31. https://doi.org/10.1186/1471-2458-10-31.
Arita I, Nakane M, Kojima K, Yoshihara N, Nakano T, El-Gohary A. Role of a sentinel surveillance system in the context of global surveillance of infectious diseases. Lancet Infect Dis. 2004;4(3):171–7. https://doi.org/10.1016/S1473-3099(04)00942-9. (Erratum in: Lancet Infect Dis. 2004;4(8):533).
Fulcher IR, Boley EJ, Gopaluni A, Varney PF, Barnhart DA, Kulikowski N, Cross-site COVID-19 Syndromic Surveillance Working Group, et al. Syndromic surveillance using monthly aggregate health systems information data: methods with application to COVID-19 in Liberia. Int J Epidemiol. 2021;50(4):1091–102. https://doi.org/10.1093/ije/dyab094.
Uwizeyimana T, Manirambona E, Saidu Musa S, Uwiringiyimana E, Bazimya D, Mathewos K. Achieving COVID-19 herd immunity in Rwanda, Africa. Public Health Chall. 2023;2:e75. https://doi.org/10.1002/puh2.75.
Sims N, Kasprzyk-Hordern B. Future perspectives of wastewater-based epidemiology: monitoring infectious disease spread and resistance to the community level. Environ Int. 2020;139: 105689. https://doi.org/10.1016/j.envint.2020.105689.
The WHO Africa. The Maputo declaration on strengthening of laboratory systems. 2008. https://www.who.int/publications/m/item/the-maputo-declaration-on-strengthening-of-laboratory-systems. Accessed 25 July 2023.
Dickmann P, Kitua A, Apfel F, Lightfoot N. Kampala manifesto: building community-based one health approaches to disease surveillance and response-the Ebola legacy-lessons from a peer-led capacity-building initiative. PLoS Negl Trop Dis. 2018;12(4): e0006292. https://doi.org/10.1371/journal.pntd.0006292.
Ellwanger JH, Chies JAB. Zoonotic spillover: understanding basic aspects for better prevention. Genet Mol Biol. 2021;44(1 Suppl 1): e20200355. https://doi.org/10.1590/1678-4685-GMB-2020-0355.
Tulchinsky TH. John Snow, cholera, the broad street pump; waterborne diseases then and now. Case Stud Public Health. 2018. https://doi.org/10.1016/B978-0-12-804571-8.00017-2.
Daughton CG. Wastewater surveillance for population-wide Covid-19: the present and future. Sci Total Environ. 2020;736: 139631. https://doi.org/10.1016/j.scitotenv.2020.139631.
Mohapatra S, Bhatia S, Senaratna KYK, Jong MC, Lim CMB, Gangesh GR, et al. Wastewater surveillance of SARS-CoV-2 and chemical markers in campus dormitories in an evolving COVID-19 pandemic. J Hazard Mater. 2023;446: 130690. https://doi.org/10.1016/j.jhazmat.2022.130690.
Sinclair RG, Choi CY, Riley MR, Gerba CP. Pathogen surveillance through monitoring of sewer systems. Adv Appl Microbiol. 2008;65:249–69. https://doi.org/10.1016/S0065-2164(08)00609-6.
Gumede N, Okeibunor J, Diop O, Baba M, Barnor J, Mbaye S, Ticha J, Weldegebriel G, Asghar H, Mkanda P. Progress on the implementation of environmental surveillance in the African region, 2011–2016. J Immunol Sci. 2018;4:24–30.
Shaheen MNF, Abd El-Daim SE, Ahmed NI, Elmahdy EM. Environmental monitoring of Aichi virus and human bocavirus in samples from wastewater treatment plant, drain, and River Nile in Egypt. J Water Health. 2020;18(1):30–7. https://doi.org/10.2166/wh.2019.075.
Mabasa VV, Meno KD, Taylor MB, Mans J. Environmental surveillance for noroviruses in selected South African wastewaters 2015–2016: emergence of the Novel GII.17. Food Environ Virol. 2018;10(1):16–28. https://doi.org/10.1007/s12560-017-9316-2.
O’Brien E, Nakyazze J, Wu H, Kiwanuka N, Cunningham W, Kaneene JB, Xagoraraki I. Viral diversity and abundance in polluted waters in Kampala, Uganda. Water Res. 2017;127:41–9. https://doi.org/10.1016/j.watres.2017.09.063.
Motayo BO, Adeniji JA, Faneye AO. Species A rotavirus (RVA) isolated from sewage in Nigeria, 2014: close genetic relatedness of partial G, P, and NSP4 gene sequences encoding G1 with cogent genes of other Asian and African rotaviruses. J Pathog. 2018;2018:8425621. https://doi.org/10.1155/2018/8425621.
Majumdar M, Sharif S, Klapsa D, Wilton T, Alam MM, Fernandez-Garcia MD, Rehman L, Mujtaba G, McAllister G, Harvala H, Templeton K, Mee ET, Asghar H, Ndiaye K, Minor PD, Martin J. Environmental surveillance reveals complex enterovirus circulation patterns in human populations. Open Forum Infect Dis. 2018;5(10): ofy250. https://doi.org/10.1093/ofid/ofy250.
Hassine-Zaafrane M, Kaplon J, Ben Salem I, Sdiri-Loulizi K, Sakly N, Pothier P, Aouni M, Ambert-Balay K. Detection and genotyping of group A rotaviruses isolated from sewage samples in Monastir, Tunisia between April 2007 and April 2010. J Appl Microbiol. 2015;119(5):1443–53. https://doi.org/10.1111/jam.12920.
Béji-Hamza A, Khélifi-Gharbi H, Hassine-Zaafrane M, Della Libera S, Iaconelli M, Muscillo M, Petricca S, Ciccaglione AR, Bruni R, Taffon S, Equestre M, Aouni M, La Rosa G. Qualitative and quantitative assessment of hepatitis A virus in wastewaters in Tunisia. Food Environ Virol. 2014;6(4):246–52. https://doi.org/10.1007/s12560-014-9163-3.
Shomuyiwa DO, Lucero-Prisno DE III, Manirambona E, Suleman MH, Rayan RA, Huang J, Zaw TN, Babatunde Y, Denkyira SA, Musa SS. Curbing antimicrobial resistance in post-COVID Africa: challenges, actions and recommendations. Health Sci Rep. 2022;5(5): e771. https://doi.org/10.1002/hsr2.771.
Mtetwa HN, Amoah ID, Kumari S, Bux F, Reddy P. Wastewater-based surveillance of antibiotic resistance genes associated with tuberculosis treatment regimen in KwaZulu Natal, South Africa. Antibiotics (Basel). 2021;10(11):1362. https://doi.org/10.3390/antibiotics10111362.
Kimosop SJ, Getenga ZM, Orata F, Okello VA, Cheruiyot JK. Residue levels and discharge loads of antibiotics in wastewater treatment plants (WWTPs), hospital lagoons, and rivers within Lake Victoria Basin, Kenya. Environ Monit Assess. 2016;188(9):532. https://doi.org/10.1007/s10661-016-5534-6.
Wu F, Xiao A, Zhang J, Moniz K, Endo N, Armas F, et al. Wastewater surveillance of SARS-CoV-2 across 40 US states from February to June 2020. Water Res. 2021;202: 117400. https://doi.org/10.1016/j.watres.2021.117400.
Mahlangeni N, Street R, Horn S, Mathee A, Mangwana N, Dias S, et al. Using wastewater surveillance to compare COVID-19 outbreaks during the easter holidays over a 2-year period in Cape Town, South Africa. Viruses. 2023;15(1):162. https://doi.org/10.3390/v15010162.
Ali S, Gudina EK, Gize A, Aliy A, Adankie BT, Tsegaye W, et al. Community wastewater-based surveillance can be a cost-effective approach to track COVID-19 outbreak in low-resource settings: feasibility assessment for Ethiopia context. Int J Environ Res Public Health. 2022;19(14):8515. https://doi.org/10.3390/ijerph19148515.
National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Division on Earth and Life Studies; Board on Population Health and Public Health Practice; Water Science and Technology Board; Committee on Community Wastewater-based Infectious Disease Surveillance. Wastewater-based Disease Surveillance for Public Health Action. Washington (DC): National Academies Press; 2023. 2, Wastewater surveillance for COVID-19. https://www.ncbi.nlm.nih.gov/books/NBK591716/.
Wang H, Wang T, Zhang B, Li F, Toure B, Omosa IB, et al. Water and wastewater treatment in Africa—current practices and challenges. Clean: Soil, Air, Water. 2014;42(8):1029–35. https://doi.org/10.1002/clen.201300208.
Manirambona E, Musa SS, Irakoze S, Uwizeyimana T, Gyeltshen D, Bizoza D, Lucero-Prisno DE III. The impact of COVID-19 on international development aid and health systems strengthening in low-income countries. Ann Med Surg. 2022;82: 104772. https://doi.org/10.1016/j.amsu.2022.104772.
Mao K, Zhang K, Du W, Ali W, Feng X, Zhang H. The potential of wastewater-based epidemiology as surveillance and early warning of infectious disease outbreaks. Curr Opin Environ Sci Health. 2020;17:1–7. https://doi.org/10.1016/j.coesh.2020.04.006.
African Development Bank, United Nations Environment Programme, GRID-Arendal. Sanitation and wastewater management atlas of Africa. 2020. https://www.afdb.org/sites/default/files/documents/publications/sanitation_and_wastewater_atlas_of_africa_compressed.pdf. Accessed 25 June 2023.
National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Division on Earth and Life Studies; Board on Population Health and Public Health Practice; Water Science and Technology Board; Committee on Community Wastewater-based Infectious Disease Surveillance. Wastewater-based Disease Surveillance for Public Health Action. Washington (DC): National Academies Press (US); 2023. 4, Strategies for achieving the vision and increasing the public health impact of national wastewater surveillance. https://www.ncbi.nlm.nih.gov/books/NBK591711/.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
EM: conceptualization, project administration, and design, data collection and literature review, preparation of the original draft and visualization, supervision, reviewing, editing, and proofreading. DELP, DOS, JOO, UAH, SAD, HMS, SSM, DOS, MN, AME: data collection and literature review, preparation of the original draft and visualization, reviewing, editing, and proofreading. All authors have read and confirm that they meet ICMJE criteria for authorship.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Manirambona, E., Lucero-Prisno, D.E., Shomuyiwa, D.O. et al. Harnessing wastewater-based surveillance (WBS) in Africa: a historic turning point towards strengthening the pandemic control. Discov Water 4, 9 (2024). https://doi.org/10.1007/s43832-024-00066-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s43832-024-00066-0