Abstract
Objectives
Acute atrial fibrillation and flutter (AF/AFL) are common arrhythmias treated in the emergency department (ED). The 2021 CAEP Best Practices Checklist provides clear recommendations for management of patients with acute AF/AFL. This study aimed to evaluate physician compliance to Checklist recommendations for risk assessment and ED management of AF/AFL.
Methods
This health records review assessed the management of adult patients presenting to two tertiary care EDs for management of acute AF/AFL from January to August, 2022. All ECGs demonstrating AF/AFL with a heart rate greater than 100 were compiled to capture primary and secondary causes. All visits were assessed for rate and rhythm control management, adverse events, return to ED, and safety criteria. Study physicians classified safety criteria from the Checklist into high and moderate concerns. The primary outcome was the proportion of cases with safety concerns and adverse events occurring during management in the ED. Data were analyzed using simple descriptive statistics.
Results
We included 429 patients with a mean age of 67.7 years and 57.1% male. ED management included rate control (20.4%), electrical (40.1%), and pharmacological (20.1%) cardioversion. Adverse events occurred in 9.5% of cases: 12.5% in rate control, 13.4% in electrical cardioversion, and 6.9% in pharmacologic cardioversion. Overall, 7.9% of cases had management safety concerns. Moderate safety concerns occurred in 4.9% of cases including failure to attain recommended heart rate at time of discharge (3.9%). Severe concerns were identified in 3.0% of cases including failure to cardiovert unstable patients (1.2%). The 30-day return-to-ED rate was 16.5% secondary to AF/AFL.
Conclusion
ED management of AF/AFL was consistent with the CAEP Checklist and was safe overall. Opportunities for optimizing care include attaining recommended targets during rate control, avoidance of calcium channel and beta blockers in patients with systolic dysfunction, and earlier cardioversion for clinically unstable patients.
Abstrait
Objectifs
La fibrillation auriculaire aiguë et le flutter (FA/FAT) sont des arythmies courantes traitées aux urgences (SU). La liste de vérification des pratiques exemplaires 2021 du CAEP fournit des recommandations claires pour la prise en charge des patients atteints de FA/FAT aiguës. Cette étude visait à évaluer la conformité des médecins aux recommandations de la liste de contrôle pour l’évaluation des risques et la gestion de la FA/FAT.
Méthodes
Cet examen des dossiers de santé a évalué la prise en charge des patients adultes qui se sont présentés à deux urgences de soins tertiaires pour la prise en charge des FA/FAT aiguës de janvier à août 2022. Tous les ECG démontrant une FA/FAT avec une fréquence cardiaque supérieure à 100 ont été compilés pour capturer les causes primaires et secondaires. Toutes les visites ont été évaluées pour la gestion du contrôle des taux et du rythme, les événements indésirables, le retour à l’urgence et les critères de sécurité. Les médecins de l’étude ont classé les critères d’innocuité de la liste de contrôle en préoccupations élevées et modérées. Le résultat principal était la proportion de cas présentant des préoccupations en matière de sécurité et des événements indésirables survenant pendant la prise en charge à l’urgence. Les données ont été analysées à l’aide de statistiques descriptives simples.
Résultats
Nous avons inclus 429 patients avec un âge moyen de 67.7 ans et 57.1% d’hommes. La prise en charge de l’urgence comprenait une cardioversion contrôlée (20.4 %), électrique (40.1 %) et pharmacologique (20.1 %). Des événements indésirables se sont produits dans 9.5% des cas : 12.5% dans le contrôle du taux, 13.4% dans la cardioversion électrique et 6.9% dans la cardioversion pharmacologique. Dans l’ensemble, 7.9 % des cas concernaient la sécurité de la direction. Des problèmes de sécurité modérés sont survenus dans 4.9 % des cas, y compris l’incapacité d’atteindre la fréquence cardiaque recommandée au moment du congé (3.9 %). Des préoccupations graves ont été identifiées dans 3.0 % des cas, y compris l’échec à cardiovert patients instables (1.2 %). Le taux de retour aux urgences après 30 jours était de 16,5 % secondaire aux FA/FAT.
Conclusion
La gestion de l’AF/AFL par le DG était conforme à la liste de vérification du CAEP et était sécuritaire dans l’ensemble. Les possibilités d’optimisation des soins comprennent l’atteinte des cibles recommandées lors du contrôle des taux, l’évitement du canal calcique et des bêtabloquants chez les patients présentant une dysfonction systolique et une cardioversion antérieure pour les patients cliniquement instables.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
What is known about this topic? |
The CAEP 2021 Best Practice Checklist provides recommendations for management of acute atrial fibrillation / flutter in the ED. |
What did this study ask? |
Are ED physicians compliant with the CAEP 2021 Checklist recommendations in acute atrial fibrillation / flutter and are there any safety concerns? |
What did this study find? |
This study found good compliance to the CAEP recommendations and elements where patient care can be improved in AF/AFL management. |
Why does this study matter to clinicians? |
Patient care can be optimized by heart rate targeting at disposition, avoidance of calcium channel and beta blockers in systolic dysfunction and cardioversion for unstable patients. |
Introduction
Atrial fibrillation and flutter (AF/AFL) are common emergency department (ED) presentations with a documented increase in hospitalizations in the last 2 decades [1]. However, studies suggest that most patients with recent onset AF/AFL may be discharged home directly from the ED after adequate rate and rhythm control [2, 3]. Historically, there was significant variation to physician management of AF/AFL in the ED [4]. The 2021 CAEP Acute Atrial Fibrillation/Flutter Best Practices Checklist was adapted from the Canadian Cardiovascular Society guidelines and offers clear recommendations for safe management of patients presenting with acute AF/AFL [5, 6]. The CAEP Checklist provides guidance on risk stratification, ED management, stroke prevention, disposition, and follow-up [5].
Given the prevalence of these tachyarrhythmias, appropriate management in the ED is integral for patient care and may mitigate rises in hospitalizations [1, 2]. Notably, practice variation is inherent in the ED and has been well documented in the management of AF/AFL [7]. The CAEP Checklist can, therefore, bridge the gap by providing unifying recommendations for ED management of AF/AFL. There are no studies which assess the 2021 CAEP Checklist in clinical practice.
The purpose of this study was to evaluate physician compliance to the 2021 CAEP Checklist with regards to risk assessment and ED management. In particular, we wished to assess safety concerns and adverse events in the management of adult patients presenting to the ED with symptomatic AF/AFL. Secondary outcomes included patient disposition, return to ED for management, and adverse events 30 days post-discharge. A complementary paper evaluates alignment with the second two parts of the checklist: stroke prevention and disposition [8].
Methods
Study design and time period
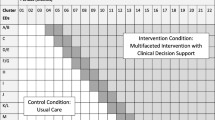
This health records review compiled all ED visits from January 1, 2022 to August 31, 2022 for patients presenting with acute AF/AFL. This study protocol was approved by our institutional research ethics board.
Study setting
This study was conducted at The Ottawa Hospital (TOH) Civic and General campus EDs, which see 180,000 patients annually. The 2 EDs are staffed by 95 attending physicians, certified in emergency medicine, along with 55 EM residents and fellows.
Population
All adult patients (≥ 18 years of age) presenting to TOH EDs with tachyarrhythmias deemed to have the diagnosis of AF/AFL as a result of primary or secondary causes were included in this study. Patients were excluded if their tachyarrhythmia was not the reason for their presentation or their heart rate was less than 100 bpm.
Data collection procedures
All ED patient visits were obtained from the EPIC health records system based on inclusion criteria to capture primary and secondary causes of AF/AFL. All ECGs were compiled if the diagnosis was “atrial fibrillation” or “atrial flutter” in the machine-generated diagnosis or following staff cardiologist review. These charts were independently reviewed and entered into an encrypted database.
Outcome measures
Safety criteria were identified from the CAEP 2021 recommendations based on consensus from a group of senior ED physicians. These criteria were then categorized into moderate or severe safety concerns. Severe safety criteria included: no electrical cardioversion if the patient was unstable; cardioversion of secondary AF/AFL; calcium channel or beta blocker use in systolic dysfunction; and attempted cardioversion if deemed unsafe based on Checklist criteria. Moderate safety concerns included: cardioversion in permanent AF/AFL; failure to attain a target heart rate by discharge; or inadequate staffing for cardioversion procedures.
Additional outcome measures collected include adverse events during ED management of the arrhythmia including hypotension (systolic blood pressure < 90), bradycardia (heart rate < 60 bpm), hypoxia (SpO2 < 90%), pulmonary edema, cardiogenic shock or cardiac arrest. Finally, we assessed patient disposition, return to ED for management, and adverse events 30 days post-discharge.
Data analysis and sample size
We chose a pragmatic sample size of 300 patients as this was thought to be large enough to be representative of care for patients in the ED and to identify safety concerns. Any discrepancies in safety assessment criteria for patient management on initial screening were reviewed by all members of the study team and resolved by consensus. Data were analyzed through descriptive statistics as appropriate for the data.
Results
Visits from 2,244 patient charts were reviewed and 429 patients met all inclusion criteria (see online supplement). Table 1 outlines the demographics and outcome measures for the included patients. The mean age was 67.7 years with 57.1% being male. Primary and secondary arrhythmias were identified in 86.9% and 13.1% of cases, respectively.
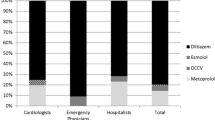
Adverse events occurred in 41 (9.5%) cases. Specifically, there were adverse events in 13.4% of patients who received electrical cardioversion, 6.9% in those who received pharmacological cardioversion, and 12.5% in those who received rate control (see Supplemental Table 1). Bradycardia occurred more often in electrical cardioversion (5.8%) when compared to pharmacologic cardioversion (1.0%) and rate control (1.1%). The incidence of hypotension was greater in pharmacological cardioversion (5.9%) and rate control (5.6%) when compared to electrical cardioversion (1.8%). Other documented adverse events following rate control included pulmonary edema (2.3%), cardiogenic shock (1.1%), and cardiac arrest (1.1%). Notably, the cardiac arrest occurred following beta blocker administration which was deemed appropriate based on CAEP recommendations. Overall, 83.4% of patients were discharged home, 15.9% were admitted to hospital, and 0.7% were deceased. The 30-day return-to-ED rate was 16.5% secondary to AF/AFL. Adverse events occurred in 2.3% of cases within 30 days of ED discharge (see online supplement).
Overall, there were 34 (7.9%) cases with management safety concerns; conversely, 92.1% had no concerns. Moderate safety concerns were identified in 4.9% of cases including failure to achieve a target heart rate at time of discharge (3.9%); inadequate staffing present for cardioversion (0.7%); and attempted cardioversion of permanent AF/AFL (0.2%). Severe safety concerns were identified in 3.0% of cases including failure to electrically cardiovert a clinically unstable patient (1.2%); the use of calcium channel or beta blocker in systolic dysfunction (0.9%); cardioversion in secondary AF/AFL (0.5%); and attempted cardioversion when deemed unsafe based on Checklist recommendations (0.5%).
Discussion
Interpretation of findings
This study highlights that most patients with AF/AFL are effectively managed in the ED with safe disposition home. An aging population and rising incidence of AF/AFL in ED patients with recurrent ED visits highlights the need for standardization of care which the CAEP recommendations provide [1]. We demonstrate that there is generally good physician compliance to the CAEP recommendations. We further emphasize where patient care can be optimized including: attaining a goal heart rate in rate control; appropriate use of AV node blockade agents; and prompt electrical cardioversion when indicated. The adverse events occurring during ED management with rate and rhythm control were generally transient with resolution prior to discharge. Finally, the incidence of adverse events occurring within 30 days of ED management was low with unclear relation to safety of the recommendations.
Comparison to previous studies
This study is the first to evaluate compliance to the 2021 CAEP Checklist for management of AF/AFL. There has been documentation of practice variation for ED management of acute AF/AFL preceding the 2021 CAEP recommendations [7]. The CAEP Checklist provides unifying recommendations which facilitates standardization of care in the ED, thereby optimizing patient care. Furthermore, there is evidence that treatment protocols for AF/AFL can reduce hospital admissions, thereby reducing overall cost to the health care system [9, 10].
Prior assessments of adverse events demonstrated that hypoxia during electrical cardioversion is likely attributed to sedation medications while all other adverse events were transient during ED management [10]. Our study highlights similar findings whereby hypotension, bradycardia, and hypoxia resolved in the ED with high rates of patients being discharged home. A complementary paper from our institution evaluated alignment with recommendations for stroke prevention and disposition, however, did not assess rate and rhythm control [8].
Strengths and limitations
A strength of this study is that it consists of a robust sample size performed at two large tertiary EDs. This facilitates the assessment of a large number of ED physicians which captures potential practice variation. A secondary strength is that this is the first study to compare the CAEP Checklist for acute AF/AFL management in the ED to current clinical practice.
A limitation of this study is that while most physicians practiced in accordance with the CAEP Checklist recommendations, given the study design, it is unclear if clinicians were referring to the Checklist or simply following their own practice. A second limitation is that this study does not account for shared decision-making that physicians have with patients during ED intervention. This includes patient preference for management options whereby patients would elect for pharmacological over electrical cardioversion when the latter would be the mainstay of treatment. We did not involve a non-academic hospital in our study and physician behavior may have been different. Further, we may have missed return-to-ED visits to other hospitals.
Clinical implications
Our study highlights a few areas where patient care can be optimized. This includes targeting a heart rate < 110 bpm with ambulation and < 100 bpm when at rest. In addition, the use of bedside POCUS may assist in evaluating cardiac systolic dysfunction and mitigate adverse events associated with use of calcium channel or beta blockers in these situations. Furthermore, rapid identification of unstable patients for prompt electrical cardioversion is essential to prevent clinical deterioration. Finally, in select cases, alternative management was performed following documentation of patient discussions weighing the risks/benefits of intervention. This highlights the patient-centered care which is provided with physician guidance.
We encourage ED physicians to refer to the CAEP Checklist (open access: https://link.springer.com/article/https://doi.org/10.1007/s43678-021-00167-y) or the free smartphone application (CAEP Atrial Fibrillation Guide on iOS and Android) [5].
Research implications
Currently, there are no studies that assess the 2021 CAEP Checklist in AF/AFL management. Formal implementation studies could facilitate the identification of overall safety of the CAEP recommendations when used in clinical practice. We encourage other hospitals to conduct similar quality assurance reviews to evaluate the safety of local practice and opportunities for improvement.
Conclusion
We found that most ED patients were treated appropriately in accordance with the CAEP Checklist with a low number of safety concerns. Opportunities for improvement include attaining recommended targets during rate control, avoidance of calcium channel and beta blockers in patients with systolic dysfunction, and early consideration of cardioversion for clinically unstable patients.
Data availability
Data available within the article or its supplementary materials.
References
Humphries KH, Jackevicius C, Gong Y, Svensen L, Cox J, Tu JV, et al. Population rates of hospitalization for atrial fibrillation/flutter in Canada. Can J Cardiol. 2004;20(9):869–76.
Stiell IG, Macle L. Canadian cardiovascular society atrial fibrillation guidelines 2010: management of recent-onset atrial fibrillation and flutter in the emergency department. Can J Cardiol. 2011;27(1):38–46. https://doi.org/10.1016/j.cjca.2010.11.014.
Vandermolen JL, Sadaf MI, Gehi AK. Management and disposition of atrial fibrillation in the emergency department: A systematic review. J Atr Fibrillation. 2018. https://doi.org/10.4022/jafib.1810.
Stiell IG, Clement CM, Brison RJ, Rowe BH, Borgundvaag B, Langhan T, et al. Variation in management of recent-onset atrial fibrillation and flutter among academic hospital emergency departments. Ann Emerg Med. 2011;57(1):13–21. https://doi.org/10.1016/j.annemergmed.2010.07.005.
Stiell IG, de Wit K, Scheuermeyer FX, Vadeboncoeur A, Angaran P, Eagles D, et al. 2021 CAEP acute atrial fibrillation/flutter best practices checklist. Can J Emerg Med. 2021;23(5):604–10. https://doi.org/10.1007/s43678-021-00167-y.
Andrade JG, Aguilar M, Atzema C, Bell A, Cairns JA, Cheung CC, et al. The 2020 Canadian cardiovascular society/Canadian heart rhythm society comprehensive guidelines for the management of atrial fibrillation. Can J Cardiol. 2020;36(12):1847–948. https://doi.org/10.1016/j.cjca.2020.09.001.
Daniel RC, Atzema CL, Cho DD, Davis PJ, Costello LL. Which recommendations are you using? A survey of emergency physician management of paroxysmal atrial fibrillation. CJC Open. 2022;4(5):466–73. https://doi.org/10.1016/j.cjco.2022.01.005.
Adler S, Mattice A, Eagles D, Yadav K, Hui S, Azward A, Pandey N, Stiell I. How well do ED physician practices align with the CAEP acute atrial fibrillation checklist for stroke prevention and disposition? Can J Emerg Med. 2024. https://doi.org/10.1007/s43678-024-00676-6
Bode W, Ptaszek LM. Management of atrial fibrillation in the emergency department. Curr Cardiol Rep. 2021. https://doi.org/10.1007/s11886-021-01611-2.
Stiell IG, Sivilotti ML, Taljaard M, Birnie D, Vadeboncoeur A, Hohl CM, et al. Electrical versus pharmacological cardioversion for emergency department patients with acute atrial fibrillation (RAFF2): a partial factorial randomised trial. The Lancet. 2020;395(10221):339–49. https://doi.org/10.1016/s0140-6736(19)32994-0.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mattice, A.M.S., Adler, S., Eagles, D. et al. Assessment of physician compliance to the CAEP 2021 Atrial Fibrillation Best Practices Checklist for rate and rhythm control in the emergency department. Can J Emerg Med 26, 333–338 (2024). https://doi.org/10.1007/s43678-024-00669-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43678-024-00669-5