Abstract
Objectives
Acute atrial fibrillation and flutter (AF/AFL) are common arrhythmias treated in the emergency department (ED). The 2021 CAEP Best Practices Checklist provides clear recommendations for management of patients with acute AF/AFL. This study aimed to evaluate physician compliance to Checklist recommendations for risk assessment and ED management of AF/AFL.
Methods
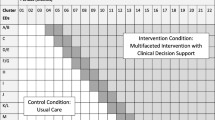
This health records review assessed the management of adult patients presenting to two tertiary care EDs for management of acute AF/AFL from January to August, 2022. All ECGs demonstrating AF/AFL with a heart rate greater than 100 were compiled to capture primary and secondary causes. All visits were assessed for rate and rhythm control management, adverse events, return to ED, and safety criteria. Study physicians classified safety criteria from the Checklist into high and moderate concerns. The primary outcome was the proportion of cases with safety concerns and adverse events occurring during management in the ED. Data were analyzed using simple descriptive statistics.
Results
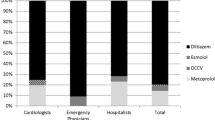
We included 429 patients with a mean age of 67.7 years and 57.1% male. ED management included rate control (20.4%), electrical (40.1%), and pharmacological (20.1%) cardioversion. Adverse events occurred in 9.5% of cases: 12.5% in rate control, 13.4% in electrical cardioversion, and 6.9% in pharmacologic cardioversion. Overall, 7.9% of cases had management safety concerns. Moderate safety concerns occurred in 4.9% of cases including failure to attain recommended heart rate at time of discharge (3.9%). Severe concerns were identified in 3.0% of cases including failure to cardiovert unstable patients (1.2%). The 30-day return-to-ED rate was 16.5% secondary to AF/AFL.
Conclusion
ED management of AF/AFL was consistent with the CAEP Checklist and was safe overall. Opportunities for optimizing care include attaining recommended targets during rate control, avoidance of calcium channel and beta blockers in patients with systolic dysfunction, and earlier cardioversion for clinically unstable patients.
Abstrait
Objectifs
La fibrillation auriculaire aiguë et le flutter (FA/FAT) sont des arythmies courantes traitées aux urgences (SU). La liste de vérification des pratiques exemplaires 2021 du CAEP fournit des recommandations claires pour la prise en charge des patients atteints de FA/FAT aiguës. Cette étude visait à évaluer la conformité des médecins aux recommandations de la liste de contrôle pour l’évaluation des risques et la gestion de la FA/FAT.
Méthodes
Cet examen des dossiers de santé a évalué la prise en charge des patients adultes qui se sont présentés à deux urgences de soins tertiaires pour la prise en charge des FA/FAT aiguës de janvier à août 2022. Tous les ECG démontrant une FA/FAT avec une fréquence cardiaque supérieure à 100 ont été compilés pour capturer les causes primaires et secondaires. Toutes les visites ont été évaluées pour la gestion du contrôle des taux et du rythme, les événements indésirables, le retour à l’urgence et les critères de sécurité. Les médecins de l’étude ont classé les critères d’innocuité de la liste de contrôle en préoccupations élevées et modérées. Le résultat principal était la proportion de cas présentant des préoccupations en matière de sécurité et des événements indésirables survenant pendant la prise en charge à l’urgence. Les données ont été analysées à l’aide de statistiques descriptives simples.
Résultats
Nous avons inclus 429 patients avec un âge moyen de 67.7 ans et 57.1% d’hommes. La prise en charge de l’urgence comprenait une cardioversion contrôlée (20.4 %), électrique (40.1 %) et pharmacologique (20.1 %). Des événements indésirables se sont produits dans 9.5% des cas : 12.5% dans le contrôle du taux, 13.4% dans la cardioversion électrique et 6.9% dans la cardioversion pharmacologique. Dans l’ensemble, 7.9 % des cas concernaient la sécurité de la direction. Des problèmes de sécurité modérés sont survenus dans 4.9 % des cas, y compris l’incapacité d’atteindre la fréquence cardiaque recommandée au moment du congé (3.9 %). Des préoccupations graves ont été identifiées dans 3.0 % des cas, y compris l’échec à cardiovert patients instables (1.2 %). Le taux de retour aux urgences après 30 jours était de 16,5 % secondaire aux FA/FAT.
Conclusion
La gestion de l’AF/AFL par le DG était conforme à la liste de vérification du CAEP et était sécuritaire dans l’ensemble. Les possibilités d’optimisation des soins comprennent l’atteinte des cibles recommandées lors du contrôle des taux, l’évitement du canal calcique et des bêtabloquants chez les patients présentant une dysfonction systolique et une cardioversion antérieure pour les patients cliniquement instables.
Similar content being viewed by others
Data availability
Data available within the article or its supplementary materials.
References
Humphries KH, Jackevicius C, Gong Y, Svensen L, Cox J, Tu JV, et al. Population rates of hospitalization for atrial fibrillation/flutter in Canada. Can J Cardiol. 2004;20(9):869–76.
Stiell IG, Macle L. Canadian cardiovascular society atrial fibrillation guidelines 2010: management of recent-onset atrial fibrillation and flutter in the emergency department. Can J Cardiol. 2011;27(1):38–46. https://doi.org/10.1016/j.cjca.2010.11.014.
Vandermolen JL, Sadaf MI, Gehi AK. Management and disposition of atrial fibrillation in the emergency department: A systematic review. J Atr Fibrillation. 2018. https://doi.org/10.4022/jafib.1810.
Stiell IG, Clement CM, Brison RJ, Rowe BH, Borgundvaag B, Langhan T, et al. Variation in management of recent-onset atrial fibrillation and flutter among academic hospital emergency departments. Ann Emerg Med. 2011;57(1):13–21. https://doi.org/10.1016/j.annemergmed.2010.07.005.
Stiell IG, de Wit K, Scheuermeyer FX, Vadeboncoeur A, Angaran P, Eagles D, et al. 2021 CAEP acute atrial fibrillation/flutter best practices checklist. Can J Emerg Med. 2021;23(5):604–10. https://doi.org/10.1007/s43678-021-00167-y.
Andrade JG, Aguilar M, Atzema C, Bell A, Cairns JA, Cheung CC, et al. The 2020 Canadian cardiovascular society/Canadian heart rhythm society comprehensive guidelines for the management of atrial fibrillation. Can J Cardiol. 2020;36(12):1847–948. https://doi.org/10.1016/j.cjca.2020.09.001.
Daniel RC, Atzema CL, Cho DD, Davis PJ, Costello LL. Which recommendations are you using? A survey of emergency physician management of paroxysmal atrial fibrillation. CJC Open. 2022;4(5):466–73. https://doi.org/10.1016/j.cjco.2022.01.005.
Adler S, Mattice A, Eagles D, Yadav K, Hui S, Azward A, Pandey N, Stiell I. How well do ED physician practices align with the CAEP acute atrial fibrillation checklist for stroke prevention and disposition? Can J Emerg Med. 2024. https://doi.org/10.1007/s43678-024-00676-6
Bode W, Ptaszek LM. Management of atrial fibrillation in the emergency department. Curr Cardiol Rep. 2021. https://doi.org/10.1007/s11886-021-01611-2.
Stiell IG, Sivilotti ML, Taljaard M, Birnie D, Vadeboncoeur A, Hohl CM, et al. Electrical versus pharmacological cardioversion for emergency department patients with acute atrial fibrillation (RAFF2): a partial factorial randomised trial. The Lancet. 2020;395(10221):339–49. https://doi.org/10.1016/s0140-6736(19)32994-0.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mattice, A.M.S., Adler, S., Eagles, D. et al. Assessment of physician compliance to the CAEP 2021 Atrial Fibrillation Best Practices Checklist for rate and rhythm control in the emergency department. Can J Emerg Med (2024). https://doi.org/10.1007/s43678-024-00669-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s43678-024-00669-5