Abstract
Purpose
The acquisition and interpretation of clinical results during resuscitations is common; however, this can delay critical clinical tasks, resulting in increased morbidity and mortality. This study aims to determine the impact of clinical result acquisition and interpretation by the team leader on critical task completion during simulated pediatric cardiac arrest before and after team training.
Methods
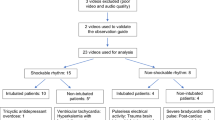
This is a secondary data analysis of video-recorded simulated resuscitation scenarios conducted during Teams4Kids (T4K) study (June 2011–January 2015); scenarios included cardiac arrest before and after team training. The scenario included either a scripted paper or a phone call delivery of results concurrently with a clinical transition to pulseless ventricular tachycardia. Descriptive statistics and non-parametric tests were used to compare team performance before and after training.
Results
Performance from 40 teams was analyzed. Although the time taken to initiate CPR and defibrillation varied depending on the type of interruption and whether the scenario was before or after team training, these findings were not significantly associated with the leader's behaviour [Kruskal–Wallis test (p > 0.05)]. An exact McNemar’s test determined no statistically significant difference in the proportion of leaders involved or not in interpreting results between and after the training (exact p value = 0.096).
Conclusions
Team training was successful in reducing time to perform key clinical tasks. Although team training modified the way leaders behaved toward the results, this behaviour change did not impact the time taken to start CPR or defibrillate. Further understanding the elements that influence time to critical clinical tasks provides guidance in designing future simulated educational activities, subsequently improving clinical team performance and patient outcomes.
Résumé
But
L’acquisition et l’interprétation des résultats cliniques pendant les réanimations sont courantes; toutefois, cela peut retarder les tâches cliniques critiques, ce qui entraîne une augmentation de la morbidité et de la mortalité. Cette étude vise à déterminer l'impact de l'acquisition et de l'interprétation des résultats cliniques par le chef d'équipe sur la réalisation des tâches critiques lors d'un arrêt cardiaque pédiatrique simulé, avant et après la formation de l'équipe.
Méthodes
Il s'agit d'une analyse de données secondaires de scénarios de réanimation simulés enregistrés sur vidéo, réalisés au cours de l'étude Teams4Kids (T4K) (juin 2011-janvier 2015); les scénarios comprenaient un arrêt cardiaque avant et après la formation de l'équipe. Le scénario comprenait un document écrit ou un appel téléphonique donnant les résultats en même temps qu’une transition clinique vers la tachycardie ventriculaire sans pouls. Des statistiques descriptives et des tests non paramétriques ont été utilisés pour comparer le rendement de l’équipe avant et après la formation.
Résultats
Les performances de 40 équipes ont été analysées. Bien que le temps nécessaire au déclenchement de la RCP et de la défibrillation ait varié selon le type d'interruption et selon que le scénario se déroulait avant ou après la formation de l'équipe, ces résultats n'étaient pas significativement associés au comportement du leader [test de Kruskal-Wallis (p > 0,05)]. Un test exact de McNemar n'a déterminé aucune différence statistiquement significative dans la proportion de dirigeants impliqués ou non dans l'interprétation des résultats entre et après la formation (valeur p exacte = 0,096).
Conclusions
La formation en équipe a permis de réduire le temps nécessaire pour effectuer les tâches cliniques clés. Bien que la formation de l'équipe ait modifié le comportement des dirigeants vis-à-vis des résultats, ce changement de comportement n'a pas eu d’incidence sur le temps nécessaire pour commencer la RCP ou la défibrillation. Une meilleure compréhension des éléments qui influencent le temps consacré aux tâches cliniques critiques fournit une orientation pour la conception des futures activités éducatives simulées, améliorant par la suite le rendement des équipes cliniques et les résultats pour les patients.
Similar content being viewed by others
What is known about the topic? |
Dealing with delivery of results in a pediatric resuscitation scenario is important as they are common and necessary to patient care. |
What did this study ask? |
What is the impact of results delivery on resuscitation performance, and meeting AHA guidelines for key clinical tasks? |
What did this study find? |
Leader involvement in delivery of results and type of results did not impact time to critical clinical tasks. |
Why does study matter to clinicians? |
Understanding how team training impacts time to performing critical clinical tasks can allow for better tailored educational activities. |
Introduction
The acquisition and interpretation of clinical results is a common and necessary occurrence in pediatric resuscitation settings. To continue effective care for patients, these interruptions (e.g., clinical results delivery via phone call or paper copy) should have minimal impact on factors that determine time to initiate critical clinical tasks such as defibrillation and cardiopulmonary resuscitation (CPR) [1, 2]. Delaying these tasks is much more likely to lead to adverse outcomes, such as increased morbidity and mortality; however, enhancing team/leader performance may mitigate any negative impact delivery of results may have [3]. Thus, understanding how teams deal with these interruptions during simulated cardiac arrest and their effect on completing key clinical tasks (team performance) will provide us with valuable educational strategies.
This study builds upon a previous article that explored the impact of a 1-day team training course on teamwork—it reported time to starting CPR and defibrillation significantly improved after training [4]. However, we do not know whether the leader’s behaviour toward the interruptions impacted the improvement in team performance. This study aims to determine the impact of clinical result acquisition and interpretation by the team leader on critical task completion during simulated pediatric cardiac arrest before and after team training.
Methods
Study design, setting, and participants
This is a secondary data analysis of video-recorded simulated resuscitation scenarios conducted during Teams4Kids (T4K) study (June 2011–January 2015) [4].
Scenario
See supplemental data for standardized scenario script (online resource 1). A transition point was scripted to include a planned interruption, which came as a phone call to provide interpretation of the patient's chest XR (CXR)/to report critical labs, or as a paper copy of a CXR/laboratory results to inform the physician of metabolic acidosis, hyperkalemia, hypoglycemia, or hypernatremia. The choice of a phone call or paper results was not random; it was based on the most likely scenario to ensure fidelity and certainty that the interruption would be reasonable based on what, when, and how it was presented (ex. a CXR was delivered if there had not been a CXR already ordered during the scenario and if the team had not looked at a CXR done in the ER). The delivery of results (interruptions) were meant to act as an interfering stimuli to the clinicians’ attention and thought process. Proper interpretation of the results would not lead to a change in immediate patient management; this would have been realized by the teams retrospectively. Results were timed to be introduced seconds before the cardiac arrest, so that the team would be tasked with analyzing the results during the event.
Variables and outcomes
Median and interquartile range (IQR) were used for quantitative time variables. Categorical variables were represented using frequencies and percentages.
This study's aim is to determine time to completion of critical clinical tasks (initiating defibrillation and CPR) based on type of results (phone call vs paper results) before and after training and leader involvement in results’ interpretation.
Video review
Video recordings were analyzed for: (a) time to initiating CPR and defibrillation, (b) time taken to analyze results concerning type of results, and (c) behaviour (involved or not involved) of leader concerning type of results. One primary video reviewer analyzed all of videos included in this analysis blinded to the performing team’s institution. Primary reviewer was trained to analyze timed outcomes by a critical care attending who led primary T4K study.
Data analysis
We summarized participant characteristics and outcomes using descriptive statistics. Non-parametric tests were used, since the variables were not normally distributed. We used median (interquartile range, IQR) for continuous variables and percentage for categorical variables. Changes before and after training were analyzed using Wilcoxon signed-rank test, Kruskal–Wallis, and McNemar test. We used SPSS Statistics for Mac (Version 27.0. Armonk, NY).
Results
Participant characteristics
A total of 40 pediatric resuscitation teams participated in 80 video-recorded simulated resuscitation events. Participants’ professional roles, clinical experience, and education are described in supplemental data (Table 1).
Time taken to analyze results and initiate CPR and defibrillation based on type of results delivered.
Results were delivered as paper results in 45/80 scenarios, and phone calls were used in 35/80 scenarios. Table 1 summarizes the time taken to analyze results and time to start CPR and shock based on delivery type (paper or phone).
The time taken to start CPR and defibrillate were not significantly different between teams who received a phone call and teams who received paper results and were not significantly different by leader behaviour [Kruskal–Wallis test (p > 0.05)].
Leader involvement in analyzing results
During the pre-training and post-training scenarios, 32 and 24 leaders, respectively, received new relevant clinical results requiring immediate interpretation. An exact McNemar’s test determined that there was no statistically significant difference in the proportion of leaders involved or not in interpreting results before and after the training (exact p value = 0.096). See Table 2 in supplemental data.
The leader behaviour (involvement in interpreting results or not) was significantly related to the type of communication of results (paper or phone call) during the post-training scenarios (Chi-square p < 0.001) but not in PRE scenarios (p > 0.430). During the post scenarios, most of the leaders did not get involved if they received a phone call (13/17, 76.5%), but when they received paper results, most of them got involved (20/23, 87%).
Discussion
We found that the teams’ ability to provide timely critical clinical tasks was not related to either the leader's involvement in the acquisition and interpretation of relevant clinical results or the mode of result delivery (paper or phone). Previous work has shown the impact of interruptions on surgical management of patients; however, no studies describe their impact on critical clinical tasks during pediatric resuscitation [1, 3, 5].
Limitations
As this was a simulation-based study, we could not replicate all unknown variables of a complex clinical environment present in real life. Delivery of results was scripted to happen simultaneously as clinical change, which may not be realistic. Furthermore, since leaders were residents, their leadership experience in resuscitation scenarios was limited. They may experience more stress, and as a result, their performance may suffer more than experienced physicians [1]. Expert attending physicians may be better at simultaneously managing interruptions and maintaining other team functions. As there was no control group without delivery of results, it is difficult to ascertain if they were the cause of delays to CPR/defibrillation provision. There are many other factors that we did not analyze which can impact team performance such as new team members joining the team and noises from other patient rooms (ex. patient alarms), which may also affect team functioning. Improvements pre- and post-training may not have been due to the training itself but may be due to increased comfort with the simulation.
Clinical implications
Leaders involved themselves more in analyzing paper results after team training. Leaders may have chosen to get involved with paper results as they take less time to analyze than phone, thus maintaining broad situational awareness of resuscitation efforts [4, 6, 7]. However, we did not find leader behaviour influenced whether teams met time to initiating key clinical tasks, and this was likely due to teams’ overall short time taking a phone call and analyzing a paper copy of results (supplemental table 2). The majority of teams took 30 s or less to accomplish these tasks, which would influence whether they met CPR initiation targets of 30 s but not necessarily defibrillation targets of 2 min. Nonetheless, it is well established that the non-technical skills of leadership such as stress management, decision-making, and situational awareness in CPR are crucial to improving team performance; training leaders in these aspects is accessible through simulation courses [6, 8,9,10].
Research implications
Future observational work with real-life resuscitation events could describe types of interruptions commonly occurring during resuscitation more accurately. In addition, including attending physicians will allow us to explore the difference prolonged training provides on effectively managing delivery of results and interruptions during resuscitation.
Conclusion
Team training was successful in reducing time to performing key clinical tasks. Although team training modified the way leaders behaved toward the delivery of results, this change in behaviour did not impact the time taken to start CPR or defibrillate. Further understanding the elements that influence time to critical clinical tasks provides guidance in designing future simulated educational activities which may subsequently improve clinical team performance and patient outcomes.
Code availability
Not applicable.
References
Sevdalis N, Undre S, McDermott J, Giddie J, Diner L, Smith G. Impact of intraoperative distractions on patient safety: a prospective descriptive study using validated instruments. World J Surg. 2014;38(4):751–8.
Nolan J. 2015 Resuscitation guidelines. Notfall + Rettungsmedizin. 2015;18(8):653–4. https://doi.org/10.1007/s10049-015-0102-0.
Bircher NG, Chan PS, Xu Y, Investigators for the AHAGWTG. Delays in cardiopulmonary resuscitation, defibrillation, and epinephrine administration all decrease survival in in-hospital cardiac arrest. Anesthesiology. 2019;130(3):414–22. https://doi.org/10.1097/ALN.0000000000002563.
Gilfoyle E, Koot DA, Annear JC, Bhanji F, Cheng A, Duff JP, et al. Improved clinical performance and teamwork of pediatric interprofessional resuscitation teams with a simulation-based educational intervention. Pediatr Crit Care Med. 2017;18(2):e62–9.
Parker SE, Laviana AA, Wadhera RK, Wiegmann DA, Sundt TM 3rd. Development and evaluation of an observational tool for assessing surgical flow disruptions and their impact on surgical performance. World J Surg. 2010;34(2):353–61.
Yeung JHY, Ong GJ, Davies RP, Gao F, Perkins GD. Factors affecting team leadership skills and their relationship with quality of cardiopulmonary resuscitation. Crit Care Med. 2012;40(9):2617–21.
Fernandez Castelao E, Boos M, Ringer C, Eich C, Russo SG. Effect of CRM team leader training on team performance and leadership behavior in simulated cardiac arrest scenarios: a prospective, randomized, controlled study. BMC Med Educ. 2015;15:116.
Gabr AK. The importance of nontechnical skills in leading cardiopulmonary resuscitation teams. J R College Physicians Edinb. 2019;49(2):112–6.
Fernandez Castelao E, Boos M, Ringer C, Eich C, Russo SG. Effect of CRM team leader training on team performance and leadership behavior in simulated cardiac arrest scenarios: a prospective, randomized, controlled study. BMC Med Educ. 2015;15(1):116.
Hunziker S, Bühlmann C, Tschan F, Balestra G, Legeret C, Schumacher C, et al. Brief leadership instructions improve cardiopulmonary resuscitation in a high-fidelity simulation: a randomized controlled trial. Crit Care Med. 2010;38(4):1086–91.
Acknowledgements
We would like to thank all study team members: Calgary: Nicola Robertson, BA, Kathy Tobler, MD, FRCPC, Amy Cripps, RRT, Jennifer Davidson, RN, Dori-Ann Martin, RN, Helen Catena, RN, Lynette Wohlmeguth, RN, MN, CPNP (PC), Tom O’Neill, PhD, and Estée Grant, MD, FRCPC. Edmonton: RN, Kristin Balon, RN, Gonzalo Garcia Guerra, MD, MSc, and Allan de Caen, MD, FRCPC. Toronto: Kristin McBain, MSc, CCRP, PMP, Elaine Ng, MD, FRCPC, Hadi Mohseni-Bod, MD, FRCPC, Darlene Murray, BSN, MSc, and Jason MaCartney, RRT. McGill: Ilana Bank, MDCM, FRCPC and Jean-François Trudel, RRT. and participants in the study. We would like to thank Sarah E Henrickson Parker for kindly granting permission to use the Severity Rating Scale. Department/institution to which the work should be attributed to: Department of Pediatrics, Cumming School of Medicine, University of Calgary
Funding
Open Access funding provided by the IReL Consortium. Carol Rizkalla received grant funding for summer research from the Emergency Strategic Clinical Network, Alberta Health Services (grant no. 4500 CAD (1500/month)).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
Institutional Review Board approval was granted at each participating institution: Alberta Children’s Hospital, Calgary, AB, Canada; Sick Kids Hospital, Toronto, ON, Canada; Stollery Children’s Hospital, Edmonton, AB, Canada, and Montreal Children’s Hospital, Montreal, QC, Canada.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
All participants have consented to publication of the study.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rizkalla, C., Garcia-Jorda, D., Cheng, A. et al. The impact of clinical result acquisition and interpretation on task performance during a simulated pediatric cardiac arrest: a multicentre observational study. Can J Emerg Med 24, 529–534 (2022). https://doi.org/10.1007/s43678-022-00313-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43678-022-00313-0