Abstract
Background
Treatment for coronavirus disease 2019 (COVID-19) evolved between pandemic waves. Our objective was to compare treatments, acute care utilization, and outcomes of COVID-19 patients presenting to emergency departments (ED) across pandemic waves.
Methods
This observational study enrolled consecutive eligible COVID-19 patients presenting to 46 EDs participating in the Canadian COVID-19 ED Rapid Response Network (CCEDRRN) between March 1 and December 31, 2020. We collected data by retrospective chart review. Our primary outcome was in-hospital mortality. Secondary outcomes included treatments, hospital and ICU admissions, ED revisits and readmissions. Logistic regression modeling assessed the impact of pandemic wave on outcomes.
Results
We enrolled 9,967 patients in 8 provinces, 3,336 from the first and 6,631 from the second wave. Patients in the second wave were younger, fewer met criteria for severe COVID-19, and more were discharged from the ED. Adjusted for patient characteristics and disease severity, steroid use increased (odds ratio [OR] 7.4; 95% confidence interval [CI] 6.2–8.9), and invasive mechanical ventilation decreased (OR 0.5; 95% CI 0.4–0.7) in the second wave compared to the first. After adjusting for differences in patient characteristics and disease severity, the odds of hospitalization (OR 0.7; 95% CI 0.6–0.8) and critical care admission (OR 0.7; 95% CI 0.6–0.9) decreased, while mortality remained unchanged (OR 0.7; 95% CI 0.5–1.1).
Interpretation
In patients presenting to cute care facilities, we observed rapid uptake of evidence-based therapies and less use of experimental therapies in the second wave. We observed increased rates of ED discharges and lower hospital and critical care resource use over time. Substantial reductions in mechanical ventilation were not associated with increasing mortality. Advances in treatment strategies created health system efficiencies without compromising patient outcomes.
Trial registration
Clinicaltrials.gov, NCT04702945.
Résumé
Contexte
Le traitement de la maladie à coronavirus 2019 (COVID-19) a évolué entre les vagues pandémiques. Notre objectif était de comparer les traitements, l'utilisation des soins aigus et les résultats des patients atteints de la maladie COVID-19 se présentant aux urgences à travers les vagues de pandémie.
Méthodes
Cette étude observationnelle a recruté des patients COVID-19 éligibles consécutifs se présentant à 46 services d'urgence participant au Réseau canadien de réponse rapide aux services d'urgence COVID-19 (CCEDRRN) entre le 1er mars et le 31 décembre 2020. Nous avons recueilli des données au moyen d’un examen rétrospectif des dossiers. Notre principal résultat a été la mortalité à l’hôpital. Les résultats secondaires incluaient les traitements, les admissions à l'hôpital et aux soins intensifs, les revisites aux urgences et les réadmissions. La modélisation par régression logistique a évalué l'impact de la vague de pandémie sur les résultats.
Résultats
Nous avons recruté 9 967 patients dans 8 provinces, 3 336 de la première vague et 6 631 de la deuxième vague. Les patients de la deuxième vague étaient plus jeunes, moins nombreux à répondre aux critères de gravité de la COVID-19 et plus nombreux à quitter les urgences. Après ajustement en fonction des caractéristiques des patients et de la gravité de la maladie, le recours aux stéroïdes a augmenté (rapport de cotes [RC] 7.4 ; intervalle de confiance à 95 % [IC] 6.2–8.9) et la ventilation mécanique invasive a diminué (RC 0.5 ; IC à 95 % 0.4–0.7) lors de la deuxième vague par rapport à la première. Après ajustement pour tenir compte des différences dans les caractéristiques des patients et la gravité de la maladie, les probabilités d'hospitalisation (RC 0.7 ; IC à 95 % 0.6–0.8) et d'admission en soins intensifs (RC 0.7 ; IC à 95 % 0.6–0.9) ont diminué, tandis que la mortalité est restée inchangée (RC 0.7 ; IC à 95 % 0.5–1.1).
Interprétation
Chez les patients se présentant dans les établissements de soins de santé, nous avons observé une adoption rapide des thérapies fondées sur des données probantes et un moindre recours aux thérapies expérimentales lors de la deuxième vague. Nous avons observé une augmentation des taux de sortie des services d'urgence et une diminution de l'utilisation des ressources hospitalières et des soins intensifs au fil du temps. Les réductions substantielles de la ventilation mécanique n'étaient pas associées à une augmentation de la mortalité. Les progrès réalisés dans les stratégies de traitement ont permis d'améliorer l'efficacité des systèmes de santé sans compromettre les résultats pour les patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
What is known about the topic? |
The patient population affected by and treatments for coronavirus disease 2019 (COVID-19) changed over the course of the pandemic. |
What did this study ask? |
How did treatments, hospital utilization and patient outcomes compare between the first two pandemic waves? |
What did this study find? |
We observed more steroid use, and less mechanical ventilation and critical care utilization with stable mortality during the second wave. |
Why does this study matter to clinicians? |
This study provides real-world evidence that practice changes in the second wave were safe and associated with lower resource utilization. |
Introduction
COVID-19 continues to place a strain on acute care hospitals. Early reports from the first wave of the pandemic were critical in allowing clinicians to gain an understanding of a new disease entity [1,2,3,4,5,6], but reflected convenience samples of patients with more severe disease and typical presentations due to limited testing capacity [7]. Most studies omitted emergency department (ED) utilization [1,2,3,4,5,6], even though EDs are the first point of contact in the acute care system.
Early in the pandemic many patients were treated with experimental therapies including antivirals such as ritonavir/lopinavir, antimalarials such as hydroxychloroquine and antihelmintics such as ivermectin based on anecdotal evidence or inconclusive studies, some of which have been disproven [8,9,10]. While high-quality randomized rials identified effective therapies and clear indications for their use [11,12,13], others remain unsupported by high quality evidence [14,15,16]. Evaluating treatments and resource utilization over time is important to understanding the uptake of evidence-based therapies and their associated patient outcomes.
The Canadian COVID-19 ED Rapid Response Network (CCEDRRN, pronounced “sedrin”) is a national collaboration that harmonized data collection on consecutive COVID-19 cases in EDs across 8 provinces [17, 18]. CCEDRRN’s goal is to generate real-world high-quality observational studies to inform the pandemic response [19, 20]. Our main objective was to describe and compare treatments, acute care utilization, and outcomes of ED patients with COVID-19 across two pandemic waves.
Methods
Design and setting
This pan-Canadian observational study enrolled consecutive eligible COVID-19 patients who presented to the EDs of 46 participating acute care hospitals between March 1 and December 31, 2020 [17]. The research ethics boards of participating institutions reviewed and approved the study protocol with a waiver of informed consent for patient enrollment. Patient partners from different areas across the country were engaged from study inception to completion. Study sponsors were not-for profit organizations, and had no role in study design, data collection, analysis, interpretation, or writing of this manuscript. All authors had access to study data and vouch for this manuscript.
Study population
Research assistants screened institutional or provincial medical microbiology testing lists for nucleic acid amplification tests (NAATs) for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and lists of presenting complaints or discharge diagnoses for consecutive eligible patients [17]. We excluded data from two sites that were unable to initiate data entry in 2020, and two sites that were unable to demonstrate ≥ 99% compliance with patient enrollment to ensure an unbiased sample.
We included COVID-19 patients presenting to the EDs of participating sites who were seen by an emergency physician, and whose medical record review was complete before the data cut (ESM Appendix Fig. 1). We excluded patients tested in the context of an elective admission, those seen directly by a consultant, and those who acquired COVID-19 in-hospital.
Definitions
We defined confirmed COVID-19 as presenting with COVID-19 symptoms and a positive SARS-CoV-2 NAAT obtained 14 days prior to, or after ED arrival. This allowed us to capture patients diagnosed in the community, and those with early false negative tests. We included patients presenting with COVID-19 symptoms and diagnosed with “confirmed COVID-19" to capture patients who were transferred into CCEDRRN hospitals whose NAAT at the sending site could not be confirmed, and patients who were presumed by treating clinicians to have COVID-19 despite negative NAATs.
We defined repeat COVID infections as cases in whom SARS-CoV-2 was isolated on two ED visits at least 90 days apart based on the longest duration of viral shedding [20,21,22].
We defined a wave as a period of sustained acceleration followed by a period of sustained deceleration in cases using the World Health Organization (WHO) dashboard for Canada. We allocated patients to the first wave if they presented between March 1 and June 30, 2020, and to the second wave if they presented between July 1 and December 31, 2020.
We defined severe COVID-19 according to WHO criteria [23]. For adults, criteria included an oxygen saturation of < 90% on room air, a respiratory rate > 30 breaths per minute, or signs of severe respiratory distress were documented in the ED.
Data collection
Trained research assistants abstracted demographic, clinical, treatment, diagnostic and outcome variables from clinical records using standardized forms. We previously evaluated the inter-rater agreement between retrospective chart review and prospectively collected data [17]. We implemented data verification and quality checks to ensure high data quality [17]. Research assistants were unaware of this research protocol at the time of chart abstraction.
We calculated the seven-day moving average incident COVID-19 cases per 100,000 population for every health region [24]. We mapped every patient to the seven-day moving average incident COVID-19 case count of their health region using their postal code of residence and index visit date. We imputed values by modeling reported COVID-19 over time using linear interpolation for the first five weeks of the pandemic, as incident COVID-19 case data were not available for this period (0.1% of values) [24].
Outcomes
Our primary outcome was in-hospital mortality. Secondary outcomes included treatments administered in hospital, hospital and ICU admissions, ED revisits and readmissions at seven and 30 days.
Statistical analysis
We summarized patient characteristics, treatments, and outcomes for each wave using descriptive statistics. We assessed wave differences with t-tests or analysis of variance (ANOVA) for continuous variables and chi-square tests for categorical variables. Separate logistic regressions with a random effect for study sites and patients modeled the associations between pandemic wave and outcomes. We considered different adjustments to provide an understanding of the incremental association between factors and pandemic waves: (1) patient (age, sex, comorbidity, tobacco and illicit substance use) and presentation characteristics (arrival mode, arrival from, and disease severity at presentation), and (2) the variables in (1) as well as the seven-day moving average incident COVID-19 cases in the patient’s health region to account for the hospital’s burden of COVID-19 [25]. We fitted continuous variables, such as age and the seven-day moving average incident COVID-19 cases, with restricted cubic splines with three knots into our logistic regression models. We conducted subgroup analyses on patients with severe COVID at presentation, pregnant patients, those reporting unstable housing, and those requiring invasive mechanical ventilation. We provided estimates with 95% confidence intervals (CIs). A cell size restriction policy prohibited us from reporting counts of less than five. A p value less than 0.05 was considered statistically significant. We conducted analyses using Stata (Version 16.1, StataCorp, College Station, Texas).
Results
Main results
We enrolled 9,967 COVID-19 patients, of whom 3,336 (33.5%) presented in the first and 6,631 (66.5%) in the second wave (Fig. 1). Of these, 3,319 were enrolled in Quebec (33.3%), 2,868 in Alberta (28.8%) and 2,458 in British Columbia (25.6%). In all but 80 (0.8%) patients, a NAAT confirmed the COVID-19 diagnosis. Follow-up time was 30 days for discharged patients and between 30 and 229 days for admitted patients.
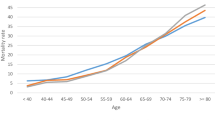
Pandemic waves
Patients presenting to hospitals differed between waves (Table 1 and ESM Appendix Table 1). During the second wave, patients were younger (mean age 53.2 versus 59.4 years old) and with fewer comorbidities compared to the first wave. In the second wave, patients were less likely to arrive from long-term care (5.6% versus 18.3%), report an occupational exposure (2.3% versus 8.7%), travel-related infection (1.9% versus 6.8%) or an institutional exposure (7.5% versus 18.6%). Fewer patients met criteria for severe disease in the second wave (27.7% versus 31.7%).
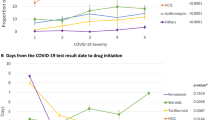
Steroids were used more frequently (28.0% versus 9.5%, p < 0.0001), and antimalarials (0.3% versus 9.0%, p < 0.0001) and antivirals (1.5% versus 6.7%, p < 0.0001) less frequently in the second wave (Table 2 and ESM Appendix Table 2). Among admitted patients, steroid use increased to 83.5% in the second wave compared to 16.9% in the first (p < 0.001), while antibiotic use remained unchanged (84.3 versus 85.3%, p = 0.6). Differences persisted after adjustment for baseline patient characteristics and disease severity (Tables 3, 4). Fewer patients were mechanically ventilated (3.7% versus 7.0%, p < 0.0001) in the second wave, which also persisted after adjustment (OR 0.56; 95% CI 0.44–0.71). Patients were intubated at the same time after the onset of symptoms (6.5 versus 6.3 days, p = 0.81), but later in their hospital course (3.2 versus 2.0 days, p < 0.0001) in the second versus the first wave, and for a shorter duration of time (12.8 versus 16.4 days, p = 0.018; ESM Appendix Table 3).
A greater proportion of patients were discharged from EDs in the second wave (61.3% versus 47.2%, p < 0.0001; Table 5 and ESM Appendix Table 4a). In the second wave a higher proportion of patients revisited the ED within seven days (6.9% versus 5.8%, p = 0.025) and were more likely to be admitted to a ward (8.2% versus 6.1%, p = 0.008; Table 6 and ESM Appendix Table 4b), but not critical care (ESM Appendix Table 5a). In both waves few patients died in the ED (0.5% versus 0.2%, p = 0.016).
In the second wave, hospital admissions were shorter (mean 11.7 versus 15.6 days, p < 0.0001), yet readmissions after hospital discharge were rare and similar across waves (Table 6 and ESM Appendix Tables 4b and 5b). In the second wave, fewer patients were admitted to critical care (7.7% versus 12.6%, p < 0.0001; Table 2, ESM Appendix Table 2) for a shorter duration of time (10.5 versus 15.6 days, p < 0.0001; Table 6, ESM Appendix Table 4b). These differences persisted after adjustment for patient characteristics, disease severity, and the seven-day moving average incident COVID-19 cases (Table 7). Crude mortality was lower in the second wave [6.1% versus 8.5%; odds ratio (OR) 0.69, 95% CI 0.59–0.82]. After adjusting for patient characteristics, disease severity, and the seven-day moving average incident COVID-19 cases we observed a trend towards reduced mortality which was not statistically significant (OR 0.7; 95% CI 0.52–1.05).
Subgroups
During the study period, fewer than five of 9,967 patients (< 0.05%, 95% CI 0.0002–0.0012%) re-visited a participating ED with a NAAT-confirmed re-infection. Among 119 pregnant patients, 28 (23.5%, 95% CI 16.7–32.0%) required admission, fewer than five (< 3.4%, 95% CI 1.2–8.7%) required mechanical ventilation, and none died. Among 176 patients reporting unstable housing (homeless, shelter, or single room occupancy), 50.6% (95% CI 43.2–57.9%) were admitted, and fewer than five (< 5%, 95% CI 0.84–5.93%) died.
Discussion
Interpretation of findings
We compared treatments, acute care utilization, and outcomes of COVID-19 patients presenting to EDs between pandemic waves and found differences in patient characteristics that we believe reflected public health measures to protect seniors and reduce travel [26]. We observed rapid uptake of evidence-based therapies and less use of experimental therapies in the second wave. The dramatic increase in steroid use among admitted patients with severe COVID-19 is consistent with its proven indications. We observed substantial decreases in invasive mechanical ventilation and less hospital and critical care utilization over time with no adverse effect on mortality.
Comparison to previous studies
Administrative database studies observed decreasing mortality during the Spring of 2020, before evidence-based treatments had been identified [6, 27]. While some hypothesized that these observations were the result of improved clinical care as clinicians gained experience treating COVID-19, it is possible that these findings were the result of ascertainment bias and confounding [7]. Testing restrictions during the first wave resulted in only the sickest COVID-19 patients being diagnosed, introducing systematic error in mortality estimates due to decreasing severity of diagnosed cases over time [28]. Administrative database studies were unable to capture respiratory parameters required to adjust for disease severity at presentation [29], resulting in mortality estimates that may be confounded [6]. Finally, during the early pandemic, residents of long-term care were tested more liberally than healthier populations. Oversampling of long-term care residents may have increased the early observed mortality risk due to competing risks [27]. In contrast, our study enrolled consecutive eligible patients through to the end of the first wave reducing ascertainment bias and selection bias, and used detailed clinical data to adjust for baseline differences in disease severity. These methodological differences may explain the observed differences in mortality across studies.
We observed changes to the frequency, initiation, and duration of invasive mechanical ventilation consistent with other studies [30]. Early in the pandemic, non-evidence based recommendations for early endotracheal intubation had been disseminated to reduce disease transmission [31]. We observed less frequent, later and shorter duration of invasive mechanical ventilation in the second wave, consistent with updated airway management guidelines. These changes were associated with reduced hospital and critical care resource utilization and no adverse impacts on mortality. Our results provide real-world evidence that a treatment strategy including reduced use of invasive mechanical ventilation was not associated with harm and may be beneficial.
Uptake of steroids among admitted hypoxic patients after publication of randomized trials and a prospective meta-analysis was rapid [32]. Previously, observed uptake of new evidence into clinical practice has been variable and much slower than what we observed [33]. While we did not collect data about knowledge translation strategies, regional COVID-19 treatment guidelines [34], podcasts with COVID-19 content [35] and other online learning tools [36] were widely shared during the first pandemic year, and may have contributed to rapid knowledge uptake.
Strengths
Unlike previous studies that were limited to single sites [37,38,39], we enrolled patients in urban and rural, and academic and non-academic sites across Canada. We captured all COVID-19 patients, including vulnerable patients who are typically unable to provide informed consent. We ascertained the outcomes of all enrolled patients, without censoring at 28 or 30 days, or at the time of analysis, as was commonly done in early studies leading to incomplete outcome ascertainment [14, 29]. For these reasons, we believe we were able to minimize ascertainment and selection bias and are confident of the internal validity of our study. We believe that our sample is representative of COVID-19 patients who presented to Canadian EDs during the study period.
Limitations
We captured data retrospectively and were limited to what was documented in the medical records. Despite research assistants not being able to support data collection in person in EDs during the first wave of the pandemic, we were able to validate our data collection methods by comparing retrospectively with prospectively collected data [17]. While we were unable to link with genomic data to identify variants of concern [40], circulation of variants was limited during the study period. Finally, we were unable to adjust for differences in patient-level goals of care across pandemic waves.
Clinical and research implications
Canadian acute care physicians rapidly implemented evolving treatment recommendations based on new evidence or expert advice in 2020. While the observational nature of our study does not allow for causal inferences, our data provide evidence that treatment changes were safe and associated with less acute care resource utilization. The observed reduction in the use of invasive mechanical ventilation was not associated with harm, and may be associated with benefit.
Our work highlights the feasibility of collaborating across Canada to enable timely evaluation of real-world practice changes during a pandemic. Attention to data quality, collection of clinical variables, and patient sampling can supplement and refine lessons learned from more rapidly conducted administrative database studies.
Conclusion
Our study documents rapid uptake of evidence during the COVID-19 pandemic, both for proven and disproven therapies. We saw increased rates of ED discharges and lower hospital and critical care resource use over time. We saw substantial reductions in mechanical ventilation without increasing mortality. Advances in treatment strategies created health system efficiencies without compromising patient outcomes.
Change history
22 April 2022
A Correction to this paper has been published: https://doi.org/10.1007/s43678-022-00314-z
References
Murthy S, Archambault PM, Atique A, et al. Characteristics and outcomes of patients with COVID-19 admitted to hospital and intensive care in the first phase of the pandemic in Canada: a national cohort study. CMAJ Open. 2021;9:E181–8.
Verma AA, Hora T, Jung HY, et al. Characteristics and outcomes of hospital admissions for COVID-19 and influenza in the Toronto area. CMAJ. 2021;193:E410–8.
Mitchell R, Choi KB, Pelude L. Patients in hospital with laboratory-confirmed COVID-19 in a network of Canadian acute care hospitals, Mar. 1 to Aug. 31, 2020: a descriptive analysis. CMAJ Open. 2019;2021(9):E149–56.
Docherty AB, Harrison EM, Green CA, et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO clinical characterisation protocol: prospective observational cohort study. BMJ. 2020;369:m1985.
Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA. 2020;323:2052.
Navaratnam AV, Gray WK, Day J, et al. Patient factors and temporal trends associated with COVID-19 in-hospital mortality in England: an observational study using administrative data. Lancet Respir Med. 2021;9:397–406.
Richterich P. Severe underestimation of COVID-19 case numbers: effect of epidemic growth rate and test restrictions. medRXiv. 2020. https://doi.org/10.1101/2020.04.13.20064220.
The RECOVERY Collaborative Group. Effect of hydroxychloroquine in hospitalized patients with Covid-19. N Engl J Med. 2020;383:2030–40.
RECOVERY Collaborative Group. Lopinavir-ritonavir in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet. 2020;396:1345–52.
López-Medina E, López P, Hurtado IC, et al. Effect of ivermectin on time to resolution of symptoms among adults with mild COVID-19: a randomized clinical trial. JAMA. 2021;325:1426.
Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the treatment of Covid-19—final report. N Engl J Med. 2020;383:1813–26.
Sterne JAC, Murthy S, WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group, et al. Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: a meta-analysis. JAMA. 2020;324:1330–41.
The RECOVERY Collaborative Group. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med. 2021;384:693–704.
Botta M, Tsonas AM, Pillay J, et al. Ventilation management and clinical outcomes in invasively ventilated patients with COVID-19 (PRoVENT-COVID): a national, multicentre, observational cohort study. Lancet Respir Med. 2021;9:139–48.
Marini JJ, Gattinoni L. Management of COVID-19 respiratory distress. JAMA. 2020;323:2329–30.
Tobin MJ, Laghi F, Jubran A. Caution about early intubation and mechanical ventilation in COVID-19. Ann Intensive Care. 2020;10:78.
Hohl CM, Rosychuk RJ, McRae AD, et al. Development of the Canadian COVID-19 Emergency Department Rapid Response Network population-based registry: a methodology study. CMAJ Open. 2021;9:E261–70.
Canadian COVID-19 Emergency Department Rapid Response Network (CCEDRRN). 2021. https://www.ccedrrn.com/. Accessed 6 Dec 2021.
McRae AD, Hohl CM, Rosychuk RJ, et al. Development and validation of a clinical risk score to predict SARS-CoV-2 infection in emergency department patients: The CCEDRRN COVID-19 Infection Score (CCIS). BMJ Open. 2021;11:e055832. https://doi.org/10.1101/2021.07.15.21260590.
Hohl CM, Rosychuk RJ, Archambault PM, et al. Derivation and validation of a clinical score to predict death among non-palliative COVID-19 patients presenting to emergency departments. The CCEDRRN COVID Mortality Score. medRXiv. 2021. https://doi.org/10.1101/2021.07.28.21261283.
Zhou B, She J, Wang Y, et al. The duration of viral shedding of discharged patients with severe COVID-19. Clin Infect Dis. 2020. https://doi.org/10.1093/cid/ciaa451.
Noh JY, Yoon JG, Seong H, et al. Asymptomatic infection and atypical manifestations of COVID-19: comparison of viral shedding duration. J Infect. 2020;81:816–46.
Interim guidance on duration of isolation and precautions for adults with COVID-19, 2021. https://www.cdc.gov/coronavirus/2019-ncov/hcp/duration-isolation.html. Accessed 8 July 2021.
World Health Organization. COVID-19 Clinical management: living guidance. 2021. https://apps.who.int/iris/bitstream/handle/10665/338882/WHO-2019-nCoV-clinical-2021.1-eng.pdf. Accessed 8 July 2021.
COVID-19 Canada. CaseDataTable. 2020. https://resources-covid19canada.hub.arcgis.com/datasets/3aa9f7b1428642998fa399c57dad8045/data?layer=1. Accessed 8 July 2021.
Asch DA, Sheils NE, Islam MN, et al. Variation in US hospital mortality rates for patients admitted with COVID-19 during the first 6 Months of the pandemic. JAMA Intern Med. 2020. https://doi.org/10.1001/jamainternmed.2020.8193.
Public Health Agency of Canada. Individual and community-based measures to mitigate the spread of COVID-19 in Canada. 2020. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/health-professionals/public-health-measures-mitigate-covid-19.html. Accessed 8 July 2021.
Strålin K, Wahlström E, Walther S, et al. Second wave mortality among patients hospitalised for COVID-19 in Sweden: a nationwide observational cohort study. meRrXiv. 2021. https://doi.org/10.1101/2021.03.29.21254557.
Boudourakis L, Uppal A. Decreased COVID-19 mortality—a cause for optimism. JAMA Intern Med. 2021;181:478–9.
Knight SR, Ho A, Pius R, et al. Risk stratification of patients admitted to hospital with covid-19 using the ISARIC WHO clinical characterisation protocol: development and validation of the 4C Mortality Score. BMJ. 2020. https://doi.org/10.1136/bmj.m3339.
Doidge JC, Gould DW, Ferrando-Vivas P, et al. Trends in intensive care for patients with COVID-19 in England, Wales, and Northern Ireland. Am J Respir Crit Care Med. 2021;203:565–74.
Zuo M-Z, Huang Y-G, Ma W-H, et al. Expert recommendations for tracheal intubation in critically ill patients with novel coronavirus disease 2019. Chin Med Sci J. 2020. https://doi.org/10.24920/003724.
Sterne JAC, Murthy S, The WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group, et al. Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: a meta-analysis. JAMA. 2020;324:1330.
Morris ZS, Wooding S, Grant J. The answer is 17 years, what is the question: understanding time lags in translational research. J R Soc Med. 2011;104:510–20.
British Columbia COVID-19 Therapeutics Committee (CTC) and COVID-19 Therapeutics Review and Advisory Working Group (CTRAWG). Antimicrobial and immunomodulatory therapy in adult patients with COVID-19. 2021 http://www.bccdc.ca/Health-Professionals-Site/Documents/Antimicrobial-Immunomodulatory-Therapy-adults.pdf. Accessed 8 July 2021.
Mel Herbert. Emergency Medicine: reviews and perspectives. 2021. https://www.emrap.org/. Accessed 3 Dec 2021.
Canadian Association of Emergency Physicians. COVID-19 Townhall. 2021. https://caep.ca/covid-19-town-hall/. Accessed 3 Dec 2021.
Radovanovic D, Pini S, Franceschi E, et al. Characteristics and outcomes in hospitalized COVID-19 patients during the first 28 days of the spring and autumn pandemic waves in Milan: an observational prospective study. Respir Med. 2021;178:106323.
Iftimie S, López-Azcona AF, Vallverdú I, et al. First and second waves of coronavirus disease-19: a comparative study in hospitalized patients in Reus, Spain. PLoS ONE. 2021;16:e0248029.
Warner F, Hitchings MDT, Cummings DAT, et al. Longitudinal changes in COVID-19 associated in-hospital mortality. medRΧiv. 2021. https://doi.org/10.1101/2021.05.04.21255938.
Jassat W, Mudara C, Ozougwu L, et al. Increased mortality among individuals hospitalised with COVID-19 during the second wave in South Africa. medRXiv. 2021; 2021.03.09.21253184. https://doi.org/10.1101/2021.03.09.21253184
Acknowledgements
We gratefully acknowledge the assistance of Ms. Amber Cragg in the preparation of this manuscript. We thank the UBC clinical coordinating centre staff, the UBC legal, ethics, privacy and contract staff and the research staff at each of the participating institutions in the network outlined in the attached Supplement. The network would not exist today without the dedication of these professionals. Thank you to our patient partners who shared their lived experiences and perspectives to ensure that the knowledge we co-create addresses the concerns of patients and the public. Creating the largest network of collaboration across Canadian Emergency Departments would not have been feasible without the tireless efforts of Emergency Department Chiefs, and research coordinators and research assistants at participating sites. Finally, our most humble and sincere gratitude to all of our colleagues in medicine, nursing, and the allied health professions who have been on the front lines of this pandemic from day one staffing our ambulances, Emergency Departments, ICUs and hospitals bravely facing the risks of COVID-19 to look after our fellow citizens and after one another. We dedicate this network to you.
Funding
The Canadian Institutes of Health Research (447679), Ontario Ministry of Colleges and Universities (C-655-2129), Saskatchewan Health Research Foundation (5357), Genome BC (COV024) and Fondation du CHU de Québec (Octroi No. 4007) provided peer-reviewed funding. The BC Academic Health Science Network and BioTalent Canada provided non-peer reviewed funding. These organizations are not-for-profit, and had no role in study conduct, analysis, or manuscript preparation.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The study authors have no conflicts of interest to declare.
Additional information
The original online version of this article was revised: The name of the Canadian COVID-19 Rapid Response Network (CCEDRRN) investigators for the Network of Canadian Emergency Researchers, for the Canadian Critical Care Trials Group was incorrect in the author line.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hohl, C.M., Rosychuk, R.J., Hau, J.P. et al. Treatments, resource utilization, and outcomes of COVID-19 patients presenting to emergency departments across pandemic waves: an observational study by the Canadian COVID-19 Emergency Department Rapid Response Network (CCEDRRN). Can J Emerg Med 24, 397–407 (2022). https://doi.org/10.1007/s43678-022-00275-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43678-022-00275-3