Abstract
Helicobacter pylori gastric infections are among the most diffused worldwide, suffering from a rising rate of antibiotic resistance. In this context, some of the authors have previously designed an ingestible device in the form of a luminous capsule to perform antibacterial photodynamic inactivation in the stomach. In this study, the light-emitting capsules were tested to verify the safety of use prior to perform clinical efficacy studies. First, laboratory tests measured the capsule temperature while in function and verified its chemical resistance in conditions mimicking the gastric and gut environments. Second, safety tests in a healthy minipig model were designed and completed, to verify both the capsule integrity and the absence of side effects, associated with its illumination and transit throughout the gastrointestinal tract. To this aim, a capsule administration protocol was defined considering a total of 6 animals with n = 2 treated with 8 capsules, n = 2 treated with 16 capsules and n = 2 controls with no capsule administration. Endoscopies were performed in sedated conditions before–after every capsule administration. Biopsies were taken from the corpus and antrum regions, while the gastric cavity temperature was monitored during illumination. The bench tests confirmed a very good chemical resistance and a moderate (about 3 °C) heating of the capsules. The animal trials showed no significant effects on the gastric wall tissues, both visually and histologically, accompanied with overall good animal tolerance to the treatment. The integrity of the administered capsules was verified as well. These encouraging results pose the basis for the definition of successive trials at the clinical level.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Helicobacter pylori (H. pylori), a Gram-negative bacterium that colonises the human stomach and duodenum, is a group 2 pathogen and a Group 1 carcinogenic agent, as defined by the International Agency for Research on Cancer [1]. Its infection is spread worldwide with a prevalence of more than 50% (up to 90% in developing countries) [2, 3] causing severe gastric pathologies among which atrophic gastritis, gastric and duodenal ulcers, MALT lymphoma and adenocarcinoma [4, 5].
Nowadays, the pharmacological treatment of H. pylori infection consists in a proton pump inhibitor (PPI) and two or three antibiotics (triple/quadruple therapy) either bismuth-based or bismuth-free (sequential and concomitant) [6]. Unfortunately, antibiotic resistance limits the effectiveness of these pharmacological therapies [7,8,9], which are also affected by non-negligible side effects.
In the research of new therapeutic modalities against bacterial infections, a promising approach is represented by photodynamic treatments, in which the absorption of light at specific wavelengths by molecules called photosensitizers (PS) in presence of oxygen leads to the formation of Reactive Oxygen Species (ROS) that can damage the biological molecules inducing cell death [10, 11]. Antibacterial photodynamic therapy (aPDT) and photodynamic inactivation (aPDI) are much considered both in in vitro and in vivo studies, with important clinical applications since few decades [12,13,14,15,16,17] as a valid antibacterial strategy, also because they are not known to determine the development of resistance [18, 19]. Helicobacter pylori produces and accumulates photosensitizers, specifically a mixture of porphyrins (protoporphyrin IX—PPIX—and coproporphyrins) [20,21,22], paving the way for a light-only-based therapeutic scheme.
Several studies about aPDI and aPDT efficacy against H. pylori have been conducted in vitro [2, 20, 23, 24] and research about the possible side effects on gastric mucosa has highlighted no cellular damage in in vitro models sensitised with PPIX [25]. In that case, the following conditions were considered: 4.8 mW/cm2 irradiance, 2 to 45 min irradiation for a light dose of 0.6–13 J/cm2. A considerable reduction of the bacterial load was also demonstrated by aPDI in patients using endoscopic light sources [26,27,28]. Nevertheless, this treatment did not lead to complete eradication, being also invasive and associated with poor patient compliance.
Therefore, alternative solutions for this kind of therapy have been studied, consisting in prototypes of endoscopic therapeutic capsules [29, 30], among which an innovative medical device consisting in a swallowable luminous capsule [31,32,33] to perform aPDI in the stomach in a minimally invasive way. Following the development of a first prototype [31], an improved capsule was designed and produced, to be tested first in laboratory, then in an animal model to prove the safety of an in vivo use and the correctness of the associated administration protocol.
In this paper, the capsule prototype is described and characterised, together with the evaluation of its resistance to chemical agents (gastric juice and bile, pH variations) and device heating during operation. Moreover, an in vivo study in a minipig animal model is shown and discussed. This study was performed on healthy animals to assess: (i) the possible harmful effects of both the gastric mucosa illumination and the capsule transit through the gastrointestinal (GI) tract; (ii) the capsule resistance during its transit in the GI tract.
2 Materials and methods
2.1 The capsule prototypes
Figure 1 shows the assembled capsule prototype considered for this study, containing the following components: (1) an external casing in polycarbonate, a biocompatible and durable material; major axis dimension is 27 mm, the radius of the central cylindrical section is 12 mm; (2) the batteries (3 × 1.55 V, SR936W, Renata SA, Switzerland); (3) a programmable electronic board, driving LED emission; (4) the LED sources (3 red and 3 blue LEDs, VLMU, Vishay Intertechnology, USA). Red LED emission is centred at λ = 646 nm, while the blue one is centred at λ = 408 nm; emission of LEDs of the same colour is synchronised; (5) a magnetic switch mounted on the board. Due to storage, transportation and animal administration needs, the default capsule mode is off until the magnet is released, which is accompanied by a time delay preceding the start of light emission (30 s in this study). This delay accounts for the mean time needed to set the device in place inside the animal stomach cavity once the switch is released and can be programmed offline. To optimise capsule transportation, a specific capsule holder was designed and built (not shown).
2.2 Laboratory tests
The following tests were performed to verify the capsule performance and safety prior to its use in the minipig model:
(a) Power consumption and light emission efficiency.
To verify that the battery power drainage allows a sufficiently long permanence in the “on” light-emitting state, the battery voltage was measured directly on the assembled electronic + LED boards, powered by the capsule batteries. Measurements were performed with a 0.7 s time resolution during a time T ~ 18 min, compatible with the expected mean residence time of the capsule inside the stomach cavity in humans [34]. Along with battery voltage, the start of light emission by both LED types was also verified by visual inspection to discard the possible presence of faulty capsules, being completed by further spectral measurements detailed in the following. LED emission was programmed to be periodic and intermittent, i.e. composed of cycles characterised by a duty ratio D defined as the percentage of the emission time over the total cycle duration. The best value for D was defined as the one associated with the maximum emitted radiant energy E during T, in laboratory conditions and relative to different a priori conditions for the capsule emission. In fact, the emitted energy per capsule will in turn drive the mean released dose in vivo, therefore, the therapeutic efficacy. E was obtained by time integration of the emitted radiant power P(t) during T, which was measured by an integrating sphere setup (UPB-150-ARTA, Gigahertz-Optik, Germany, Fig. 2). The capsule LEDs and circuitry, powered by fully charged batteries, were inserted into the sphere. Different experiments (5 for each D value) were performed with D = 0.5, 0.6, 0.75, 0.9 respectively, and a fixed total cycle duration of about 2 s; D was varied after programming the capsule electronic board.
For each chosen D value, the following procedure was defined: (i) the emitted spectral radiant power dPi/dλ = dP (ti)/dλ in the range 380–700 nm was measured at a mean rate of 1 measurement/5 s (ti = start of measurement time) during LED emission with a 4 ms integration time, thanks to a fibre-coupled spectrometer (AVASPEC2048XL, Avantes, The Netherlands). Previous calibration of the sphere-spectrometer system was used to obtain absolute units (mW/nm) for dP/dλ; (ii) for each measurement time ti, the radiant power Pi = P(ti) was obtained by integrating each dPi/dλ over the acquired spectral range; (iii) the different D value cases were studied by comparing E(D), the numerical integrals of Pi(t) over T; the final value of the duty ratio was chosen as the one associated with the maximum value of E(D).
(b) Temperature
The capsule inner temperature was monitored by a thermistor (NTC B57861S502F40, TDK, Milan, Italy) during light emission in the following controlled conditions: air temperature = 40 °C; relative air humidity = 34%. During measurements, performed with a 0.7 s time resolution, the temperature sensor was placed in proximity of the capsule batteries. Besides, a thermal camera (TiS10, Fluke Corporation, USA) was used to monitor the capsule surface temperature before and during light emission in air laboratory conditions, considering the emissivity of the plastic material for the casing by choosing the correct pre-set value in the device software. Images were taken with a mean frequency of 1 image every 10 s.
(c) Chemical resistance and pH tests.
The capsule resistance to chemical agents and pH variation were tested simulating the passage of the device through the digestive apparatus (stomach and intestine), both in the “on” (light emission) and “off” states. First, the capsule was immersed for 2 h in a pH2 HCl solution and then for 48–72 h in a pH 8 NaHCO3 solution, mimicking the stomach acidic and intestine basic environments. In both cases, the temperature was maintained at 40 °C by use of a water bath. Additional tests were also implemented by immersing the capsule for 2 h into solutions simulating the gastric juice and bile, prepared as reported in [35].
2.3 Animal tests
The study was conducted in a minipig animal model (Sus scrofa domesticus), being approved by the Italian Ministry of Health (Authorization 176/2018, 27-Feb-2018) in accordance with the Italian legislative decree 26/2014. The study was carried out at the Toscana Gabriele Monasterio Foundation, Centre for Experimental Biomedicine (CBS), Pisa, Italy. Six adult and sexually intact males minipigs were used (weight 40 kg), coming from the Experimental Surgery Unit at San Piero a Grado, Pisa. The animals were housed in single cages, in visual and olfactory contact with other animals of the same species. The environmental parameters were checked daily. The diet consisted of feed for pigs in pellets (800 g/day) free of foods containing photosensitizing substances (Pig 1020 and Stalla Fibra Progeo in the proportion 2:1) with ad libitum water. Animals presenting symptoms such as vomiting, diarrhoea or a decrease in food intake were excluded.
Two groups were defined: treated (receiving light irradiation by the capsules) and control animals (no capsule administration). Before each endoscopy the animals fasted for 24 h; they were then anaesthetised with Zoletil® (10 mg/kg), Stresnil® (2 ml) and atropine (0.05 mg/kg) intramuscular and subsequently propofol (1 mg/kg) endovenous. Anaesthesia was maintained with 1% isoflurane by orotracheal intubation.
2.4 Study protocol
The study protocol was structured as follows.
Treated group (four animals).
In the treated group, 2 animals were administered 8 capsules during a time span of 16 days and 2 animals were administered 16 capsules during a time span of 32 days. For each animal belonging to the treated group, the protocol was the following, defining the time origin at day 1 when the first capsule is administered:
-
1)
Pre-treatment endoscopy: day-7, 1 week before the start of the capsule treatment: one endoscopy under anaesthesia, including gastric mucosal biopsies, to evaluate the stomach conditions before the capsule treatment.
-
2)
Treatment period: day 1 to 16 (2 animals) and day 1 to 32 (2 animals). In either case, at day 1 and every 2 days after day 1, the following procedures were performed: a macroscopic examination of the gastric wall by endoscopy. In case that evident damage signs are noticed (such as erosions or large erythema), no capsule is administered. The endoscope is passed through a lubricated silicon tube, previously positioned into the oesophagus. If no damage signs are noticed, the endoscope is retracted, and one light-emitting capsule is administered under anaesthesia by passing it into the silicon tube with the aid of 50 ml of water. Capsules are introduced in the off state, turning on automatically after 30 s (see Materials and Methods). Afterwards, the endoscope is inserted again to verify the capsule positioning and be ready for successive inspection and endoscopies. The gastric wall temperature was measured before and after capsule administration using a temperature probe (Hewlett-Packard model 66S, HP GmbH, Germany) positioned as close as possible to the capsule and connected with the endoscope monitor.
-
3)
Follow-up chronic analysis, 1 week after the end of the treatment: day 16 + 7 (2 animals) and day 32 + 7 (2 animals): one final endoscopy under anaesthesia + stomach mucosal biopsies.
Control group (2 animals).
-
1)
First endoscopy: day-7. One endoscopy under anaesthesia, including gastric mucosal biopsies.
-
2)
Day 1 to 32. At day 1 and every 2 days after day 1: macroscopic examination of the gastric wall by endoscopy. The gastric wall temperature was measured as described for the treated group of animals.
-
3)
Follow-up analysis at both day 16 + 7 and day 32 + 7. One endoscopy under anaesthesia + stomach mucosal biopsies.
The animals of the control group followed the same three steps as described above, except for point (2) where the capsules were not administered. In fact, the proposed treatment corresponds to the presence of light-emitting capsules. Being light emission necessarily associated with capsule administration, the “no treatment” (control) case corresponded to no given capsules.
2.5 Endoscopies and biopsies
All endoscopies were performed using the processor Tele Pack Vet X Led, Karl Storz Germany, and a 3 m long scope (10.4 mm diameter), 60130PKS, Karl Storz, Germany, under anaesthesia and according to the literature [36, 37]. The endoscope was introduced through the mouth across the cranial oesophageal sphincter and pushed along the oesophagus to the stomach. Once there, all parts of the organ were evaluated (antrum, corpus, and fundus) to identify lesions of the mucosa, such as hyperaemia, erosions, and ulcerations (Fig. 3). Gastric biopsy samples (4 for each time point) were collected with a forceps delivered through the working channel of the endoscope in two different sites of the stomach (antrum and corpus). Biopsies were taken superficially (epithelium, glands and muscularis mucosae) and avoiding sites where signs of previous biopsies (e.g. scars) should be visible. Due to the presence of capsule-gastric wall relative movements, biopsies were not restricted to the vicinity of the capsule position at a definite time. In any case, endoscopic examination was considered as the most informative technique to analyse possible damage to the gastric wall, being biopsy samples an additional source of information. The number of endoscopies and biopsies was kept to a minimum, in accordance with the guidelines for animal wellbeing and compatible with the necessity to obtain scientifically sound data. In this regard, emerging methodologies such as non-invasive monitoring techniques by infrared spectroscopy [38] were not considered as they apply to infected cases and not to safety-only studies with non-infected animals.
Before each capsule administration, at the endoscopic examination, a macroscopic evaluation of gastric mucosa was performed to assess the presence/absence of erythema, bleeding, erosions, necrosis, scars from previous biopsies undergoing re-epithelialization. Before, during and after the treatment a stool sample for evaluation of the presence of occult blood in the faeces was collected. Capsule recovery and integrity were accomplished following the control of the faeces.
The biopsy samples were fixed by formalin (37% formalin; Sigma Aldrich, St. Louis, MO, USA) and included in paraffin (Shandon; Thermo Fisher Scientific, Waltham, MA, USA). Then, the tissue specimens were cut into 4 μm sections at various depths and put on positive charged glass slides (Bio-Optica, Milan, Italy), dewaxed in xylene and rehydrated with graded alcohols. The sections were stained with haematoxylin–eosin (Bio-Optica, Milan, Italy), dehydrated by graded alcohols and mounted using a synthetic mounting medium (Bio-mount, Bio-Optica, Milan, Italy). The histological samples were observed and examined with a binocular microscope (Leitz Laborlux, Leica Microsystems GmbH, Germany) with 10×, 20× and 40× objectives. Images of the samples were acquired with a Canon CCD camera (Canon Power shot S40, 2272 × 1074, ~ 23 × 20 μm pixels, Canon Inc. Japan). The presence of microscopic damage was evaluated through examination of the gastric biopsies, assigning a score (0: absent, 1: scant, 2: abundant) to each of the following parameters: epithelial desquamation, micro-erosion, presence of inflammatory cells, vascular congestion or hyperaemia, lamina propria oedema. For each animal of both the control and the two treated groups (8 and 16 capsules), a total damage score was obtained for both the pre- and post-treatment conditions, where biopsies were obtained. Statistical analysis was performed by the Mann Whitney U test to compare: (i) post-treatment samples for the different treated animals (separately for 8-capsule and 16-capsule cases); (ii) post-treatment samples for the control animals; (iii) pre- and post-treatment samples of the different treated animals; (iv) post-treatment samples between treated and control cases.
2.6 Animal wellbeing
Analysis of animal wellbeing was based upon the observation of general and specific parameters, each being associated to a score according to Table 1. Scores were assigned daily at each parameter and animal, during the whole study protocol. For the management of possible emergency situations, a specific action protocol was defined, including immediate action to be taken with pharmacologic treatments.
3 Results
3.1 Laboratory tests
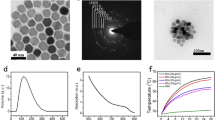
Battery voltage, measured during light emission, showed a mean decrease in time of about 0.5–1% per minute, according to the chosen duty ratio value and associated with battery consumption. This corresponds to an overall decrease of about 10–20% over the whole emission duration. During voltage measurements, the presence of LEDs emission was always visually verified. The emission spectra of both red and blue LEDs are shown in Fig. 4, together with the time trend of their emission when powered by the batteries. Table 2 resumes the results for the relative emitted energy corresponding to the various chosen values of D.
Temperature monitoring results are represented in Fig. 5. The maximum reproducibility error over all temperature values was estimated to be ± 0.5 °C.
The tests for the resistance evaluation to chemical agents (gastric juice, bile fluid and pH variation) highlighted that the capsule shell remained always intact and transparent, with no liquid contamination inside the capsule itself. Electronic board functionality was maintained.
3.2 Animal experimentation
All animals showed a very good tolerance for all undergone treatments. All animals fed regularly. No signs of suffering, fever or gastrointestinal disease were evidenced, with no need to prescribe analgesic or gastroprotective treatments. In reference to the animal wellbeing, none of the chosen parameters departed from the basal values, for all animals and evaluation times. All the administered capsules were expelled intact with no signs of digestive injury. The end-of-treatment video-endoscopies showed no differences in the gastric mucosa macroscopic and microscopic conditions compared with the start-of-treatment ones. In particular, the macroscopic evaluation of the mucosa did not show any abnormality during the study, such as signs of mechanical damage, oedema, or inflammatory processes (Fig. 6). Moreover, no significant difference was measured in the stomach wall temperature before and after each capsule administration: the recorded temperatures oscillate between 33 and 36 °C, reaching the value of 38 °C in one animal case only. Analysis and comparison of the biopsies collected in treated and control animals confirmed the gastroscopy observations. No evidence of histological mucosa alterations such as epithelial desquamation, micro-erosions, inflammatory cell infiltration, hyperaemia, or oedema of the lamina propria (Figs. 7 and 8) was observed in any of the treated and control animals.
Images of gastric biopsies of treated animals. All specimens were stained with haematoxylin and eosin. a Antrum at endoscopy a week before the beginning of capsule administration; b antrum at endoscopy a week after the end of the treatment; c corpus at endoscopy a week before the beginning of capsule administration; d corpus at the endoscopy a week after the end of the treatment
As far as histological mucosal alterations are concerned (Figs. 7 and 8), no significant difference was observed in any of the following cases: treated animals with each other, pre- and post-treatment cases with each other, treated and control cases.
4 Discussion
This study regards the assessment of the safety of use and administration of an innovative swallowable and luminous capsule, to perform aPDI in the stomach against H. pylori. Endoscopic capsules have long been used in the clinical practice for diagnostic purposes, being this one of the first attempts to use such a device for a therapeutic treatment, for the eradication of H. pylori gastric infection. In the broader context of ingestible medical devices, the two subsets of endoscopic (diagnostic) and therapeutic ones are unevenly distributed. On the one hand, we can affirm that the subset of capsule endoscopy belongs for many aspects to the state-of-the-art technology, even if new and more intelligent ways to collect and process information could lead to important innovations. On the other hand, the device presented in this study belongs to the much narrower context of therapeutic capsules. Here, major differences in the design, components and administration protocol can arise, mainly due to the need for maximising the energy stored in the device itself and the efficiency to exploit it for therapeutic purposes. This is true either in the case of devices to perform phototherapy, like ours, or when different therapeutic principles and protocols are considered. In fact, various solutions have been designed, mainly for drug delivery in the gastrointestinal tract or using ultrasound-based effects [30]. In one case [29], a capsule for intragastric phototherapy has been conceived, with blue-only emitted light and a pH-driven scheme for light emission inside the stomach cavity. Nevertheless, no safety studies have been disclosed till now for any of those devices. The development of the device described in this work is part of the research regarding the use of antimicrobial phototherapies as an alternative to the usual pharmacological treatments, whose efficacy is undermined by the spread of antibiotic resistance. In this context, the main strengths of the proposed approach are its minimal invasiveness and the absence of drug (photosensitizer) administration, these being also and ultimately the reasons for its weaknesses. Let us remember, however, that the exploitation of endogenous porphyrins only, enhances the selectivity of the proposed aPDI approach.
In a more comprehensive framework, the presented studies represent the initial part of a process whose final aim will be to demonstrate the clinical therapeutic efficacy of the ingestible capsule. To reach that goal, the following methodology was considered: (1) R&D activities, including theoretical and in vitro models, to design, produce and characterise a functioning prototype to be used in a therapeutic approach to Hp-associated infections; (2) safety tests (laboratory + animal models); (3) efficacy tests in humans. Regarding point (1) in particular, previous studies [25, 30, 39] have already defined the basis to claim the a priori feasibility of the capsule-based therapeutic approach. That claim must find a substantiation in points (2) and (3), as described above. In this approach, doubts about the therapeutic efficacy are certainly conceivable but not incompatible with the development of stage (1) and, above all, stage (2), being stage (3) the real verification point. Of course, this argument can also be applied to other therapeutic capsule prototypes with different working principles, which in our knowledge have not been accompanied by any safety neither efficacy results in a clinical setting till now.
In step (1), the main output consisted in producing prototypes whose characteristics (dimensions, emission, etc.) were as much close as possible to the desired ones, previously defined by theoretical and semi-theoretical models. Then, step (2) was performed, and its illustration and discussion represent the scope of this work. The safety tests were subdivided into: (i) laboratory tests and (ii) tests on animals.
Starting from the casing, biocompatibility, durability, and transparency (transmittance spectrum) were the main needed properties. Among the chosen materials for endoscopic capsules, polycarbonate and Poly(methyl methacrylate) are the most used and have similar transparency properties for the same thickness, which led to the choice of one of them (polycarbonate) for the casing. The LED sources were first chosen according to their emission peak wavelength, then dimensions and nominal emitted power were considered. Certainly, different choices could have led to different performances in terms of capsule emission geometry and power. A comprehensive study in this field is very complex and out of the scope of this work. In fact, numerous parameters are present with coupled influence on the final device performance, such as the total emitted radiant power, emission geometry and spectrum, pulsed/continuous emission, pulse duration and duty ratio, and heat production and its influence on LED emission. Rather, a definition of the “best” desired emission and performance is difficult as well, being the device in vivo efficacy the final proof, also considering the absence of active movements of the device that could drive the illumination geometry in vivo. In our case, priority was given to the need of maximising the emitted radiant energy in a definite time, corresponding to the mean expected residence time in the gastric cavity. For this, a programmed pulsed emission was first defined to facilitate heat dispersion. Then, four different duty ratios were defined in the reasonable range 0.5–0.9. The final chosen value for the duty ratio was 0.6. In fact, the energy emission values associated with D = 0.6 and 0.75 coincide within the error, the emission with D = 0.6 being more constant over time. The emission pulse duration (Tpulse = 2 s) was chosen to be much smaller than the whole expected stomach illumination time and at the same time much bigger respect to the LED switching time between the “on” and “off” states. Tpulse was kept constant for all D values, which were then characterised by different duration for the “on” and “off” states respectively.
In analysing Table 2, there are limitations linked to battery and LED performances and the way power is transferred between them. The prototype presented in this work corresponds to the best result obtainable in our knowledge and with our current capacities, even if a newer capsule design is under consideration with an expected improvement factor in the emitted energy of at least 2–3. In particular, of the unavoidable limiting factors is certainly the way batteries are designed and built, which in turn drives the energy coupling between them and the LEDs. Unfortunately, in our knowledge, the totality of commercial and miniaturised batteries is designed to last as much long as possible, which does not optimise their performance for our specific application. It must be considered that, for the moment, an ad hoc solution for the batteries was not feasible due to both technological and cost-related issues. No issues arose from the point of view of LED driving voltage, which proved to drive light emission for the whole 18-min time span.
The monitor of the device heating represents one important “check point”, corresponding the capsule to an “ingestible lamp” in a first instance. The temperature was first measured in proximity to the batteries. The chosen experimental conditions for air temperature and relative humidity correspond to those present in the capsule assembly room and, therefore, to the inner capsule atmosphere conditions, which are not expected to vary during all further experiments and trials due to the capsule sealed state. Then, a more general view of the device heating during operation was obtained by use of a thermal camera, allowing the discrimination between the various capsule point. The images show a more pronounced temperature increase of 5 °C respect to the mean temperature, corresponding to the central battery section surrounded by the electronic board, with a mean temperature increase of less than 3 °C respect to the environment. By analysing the maximum temperature behaviour in time in laboratory conditions, a temperature plateau for the mean device temperature is reached after about 5 min since the light emission start. Let us remember that, in normal physiological conditions, the gastric wall mean temperature is supposed to be at around 37 °C for an empty stomach. The choice to perform thermal measurements in air represents a worse scenario respect to in vivo conditions, where thermal relaxation can profit from the presence of gastric liquids and contact with the gastric wall, supposedly lowering both the device peak and mean temperature. Let us also consider that in vivo tissue heating associated to a possible light absorption is probably negligible respect to heat production due to LED and circuitry operation. This is reasonable, due to the power-light conversion efficiency being ≈ 20–25%. Further investigations, such as those related to convection, were out of the scope of this study: in-air thermal measurements were considered a sufficiently good indicator to proceed with in vivo temperature studies. In fact, a very acceptable performance in terms of working temperature was observed in a “worst case scenario” for in vivo conditions. The specific trials evidenced a good chemical resistance of the prototype both in the “on” and “off” states.
All these were comforting results to proceed with the successive in vivo safety evaluation in the minipig model to further study the device response to in vivo stresses and the possible undesired effects for the animal itself. In this context, healthy animals were preferred to those infected by H. pylori. In fact, on one hand it is true that the presence of the bacterium is in principle associated with a certain level of sensitisation for the gastric wall, due to the expected release of endogenous porphyrins. Nevertheless, previous studies [20, 25] indicate a negligible effect for the mucosa cells at the expected porphyrin concentrations.
For the safety studies, device prototypes were administered in vivo in healthy animals and in controlled conditions, following approval of a specific protocol by the local ethical committee and the Italian Ministry of Health. The effective capsule functioning inside the animal gastric cavity was verified, together with the absence of macroscopic and microscopic damage to the stomach wall tissue associated to possible local heating and/or mechanical forces. This was confirmed by analysis of gastric endoscopies and comparison of biopsy sample investigation before and after capsule illumination and transit in the GI tube. In particular, the onset of epithelial desquamation, micro-erosions, presence of inflammatory cells, hyperaemia, and oedema was excluded by statistical tests following examination of the histological samples. Besides, the overall animal wellbeing was also verified during and after the whole treatment by monitoring a series of pre-defined parameters associated to a score given by the veterinary (Table 1). In this context, a statistical evaluation of the results was not performed, mainly due to all the parameters remain unchanged. The capsule integrity after treatment and expulsion was confirmed. It must be noted that the relatively low measured temperature of the animal gastric wall (33–36 °C in 5 cases out of 6) is due to the anaesthesia, which is associated with a known and systemic hypothermic effect.
In a step-by-step approach to obtaining the best capsule performances in both safety and efficacy, these results encourage us in adding new features to the device, besides further improving the device performance in terms of battery-LED coupling with more custom solutions. The new features consist in a temperature and a pH sensor. The first one is related to a further safety improvement, to switch off illumination in the remote possibility that the device experiences an excessive heating. The second one is associated to both safety and efficacy improvements: it will turn off the capsule while entering the intestine, to avoid any possible damage associated with intestinal flora photosensitization. At the same time, the pH sensor will maintain the light emission while in the stomach cavity, overcoming the possible limitations related to a pre-defined time emission, like in the present study. Further improvements for the device will concern a further optimization of energy draining to maximise the released light dose, besides a possible reduction in size. As far as the animal model is concerned, further experiments could be performed with infected minipigs even if, in our opinion, the gap in the definition of good, infected models in this field has still to be closed.
As a final remark, we can confirm that this study was performed according to a general practise where safety studies in an animal model are accomplished before any further step is done in a clinical setting with safety and/or efficacy purposes. In principle, different choices could be considered, such as to also perform efficacy studies in an animal model before doing the same in humans. This could be a way to proceed, provided an appropriate animal infection model is considered.
5 Conclusions
Prototypes of an ingestible luminous capsule to perform aPDI in the stomach were produced and characterised. Their safety was confirmed by on the bench and animal test results, which is normally considered as a prerequisite to further proceed with safety and efficacy studies in a clinical setting, regardless of whether efficacy studies are performed on an animal model. Therefore, these outcomes are very encouraging for the progression of the study in humans, not only for testing the safety of the capsule, but above all, for evaluating its therapeutic efficacy, alone or in possible association with antibiotic therapy [40].
Availability of data and materials
The datasets generated during and/or analysed during the current study are not publicly available due to ongoing R&D activity linked to future industrial production by Probiomedica srl or associated partners, but are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
International Agency for Research on Cancer, World Health organization. (1994). Schistosomes, liver flukes and Helicobacter pylori. In: AIRC Monographs on Evaluation of Carcinogenesis Risks to Humans. IARC Press, Volume 60, p. 177.
Gerrits, M. M., van Vliet, A. H. M., Kuipers, E. J., & Kusters, J. G. (2006). Helicobacter pylori and antimicrobial resistance: Molecular mechanisms and clinical implications. Lancet Infection Disease, 6, 699–709.
Dunn, B. E., Cohen, H., & Blaser, J. (1997). Helicobacter pylori. Clinical Microbiology Reviews, 10, 720–741.
Sugano, K., Tack, J., Kuipers, E. J., Graham, D. Y., El-Omar, E. M., Miura, S., Haruma, K., Asaka, M., Uemura, N., Malfertheiner, P., & Faculty Members of Kyoto Global Consensus Conference. (2015). Kyoto global consensus report on Helicobacter pylori gastritis. Gut, 64, 1353–1367. https://doi.org/10.1136/gutjnl-2015-309252
Fasciana, T., Capra, G., Cala’, C., Zambuto, S., Mascarella, C., Colomba, C., Di Carlo, P., & Giammanco, A. (2017). Helicobacter pylori and Epstein–Barr co-infection in gastric disease. Pharmacology Online, 4, 73–82.
Fallone, C. A., Chiba, N., van Zanten, S. V., Fischbach, L., Gisbert, J. P., Hunt, R. H., Jones, N. L., Render, C., Leontiadis, G. I., Paul, M. P., & Marshall, J. K. (2016). The toronto consensus for the treatment of Helicobacter pylori infection in adults. Gastroenterology, 15, 51-69.e14. https://doi.org/10.1053/j.gastro.2016.04.006
Savoldi, A., Carrara, E., Graham, D. Y., Conti, M., & Tacconelli, E. (2018). Prevalence of antibiotic resistance in Helicobacter pylori: A systematic review and meta-analysis in World Health Organization regions. Gastroenterology, 155, 1372–1382. https://doi.org/10.1053/j.gastro.2018.07.007
Rosbach, A. (2012). The bacterial Challenge: time to react. ECDC/EMA joint technical report 2009; Committee on the Environment, Public Health and Food Safety, Report on the “Microbial Challenge-Rising threats from Antimicrobial Resistance”
Fasciana, T., Calà, C., Bonura, C., Di Carlo, E., Matranga, D., Scarpulla, G., Manganaro, M., Camilleri, S., & Giammanco, A. (2015). Resistance to clarithromycin and genotypes in Helicobacter pylori strains isolated in Sicily. Journal of Medical Microbiology, 64, 1408–1414. https://doi.org/10.1099/jmm.0.000163
Wilson, B. C., & Patterson, M. S. (2008). The physics, biophysics and technology of photodynamic therapy. Physics in Medicine and Biology, 53, R61.
Wang, Y., Wang, Y., Wang, Y., Murray, C. K., Hamblin, M. R., Hooper, D. C., & Dai, T. (2017). Antimicrobial blue light inactivation of pathogenic microbes: State of the art. Drug Resistance Update, 33–35, 1–22. https://doi.org/10.1016/j.drup.2017.10.002
Dougherty, T. J. (2002). An update on photodynamic therapy applications. Journal of Clinical Laser Medicine & Surgery, 20, 3–7. https://doi.org/10.1089/104454702753474931
Kharkwal, G. B., Sharma, S. K., Huang, Y. Y., Dai, T., & Hamblin, M. R. (2011). Photodynamic therapy for infections: Clinical applications. Lasers in Surgery and Medicine, 43, 755–767. https://doi.org/10.1002/lsm.21080
Van Straten, D., Mashayekhi, V., De Bruijn, H. S., Oliveira, S., & Robinson, D. J. (2017). Oncologic photodynamic therapy: Basic principles, current clinical status and future directions. Cancers, 9, 19. https://doi.org/10.3390/cancers9020019
Cieplik, F., Deng, D., Crielaard, W., Buchalla, W., Hellwig, E., Al-Ahmad, A., & Maisch, T. (2018). Antimicrobial photodynamic therapy—what we know and what we don’t. Critical Reviews in Microbiology, 44, 571–589. https://doi.org/10.1080/1040841X.2018.1467876
Ferreira Dos Santos, A., Raquel Queiroz De Almeida, D., Ferreira, T. L., Baptista, M., & Labriola, L. (2019). Photodynamic therapy in cancer treatment—an update review. Journal of Cancer Metastasis and Treatment, 5, 25. https://doi.org/10.20517/2394-4722.2018.83
Quilbe, A., Moralès, O., Baydoun, M., Kumar, A., Mustapha, R., Murakami, T., Leroux, B., de Schutter, C., Thecua, E., Ziane, L., Colombeau, L., Frochot, C., Mordon, S., & Delhem, N. (2020). An efficient photodynamic therapy treatment for human pancreatic adenocarcinoma. Journal of Clinical Medicine, 9, 192. https://doi.org/10.3390/jcm9010192
Al-Mutairi, R., Tovmasyan, A., Batinic-Haberle, I., & Benov, L. (2018). Sublethal photodynamic treatment does not lead to development of resistance. Frontiers in Microbiology, 9, 1699. https://doi.org/10.3389/fmicb.2018.01699
Ma, J., Hiratsuka, T., Etoh, T., Akada, J., Fujishima, H., Shiraishi, N., Yamaoka, Y., & Inomata, M. (2018). Anti-proliferation effect of blue light-emitting diodes against antibioticresistant Helicobacter pylori. Journal of Gastroenterology and Hepatology, 33, 1492–1499. https://doi.org/10.1111/jgh.14066
Hamblin, M. R., Viveiros, J., Yang, C., Ahmadi, A., Ganz, R. A., & Tolkoff, M. J. (2005). Helicobacter pylori accumulates photoactive porphyrins and is killed by visible light. Antimicrobial Agents and Chemotherapy, 49, 2822–2827. https://doi.org/10.1128/AAC.49.7.2822-2827.2005
Battisti, A., Morici, P., Ghetti, F., & Sgarbossa, A. (2017). Spectroscopic characterization and fluorescence imaging of Helicobacter pylori endogenous porphyrins. Biophysical Chemistry, 229, 19–24. https://doi.org/10.1016/j.bpc.2017.05.010
Battisti, A., Morici, P., Signore, G., Ghetti, F., & Sgarbossa, A. (2017). Compositional analysis of endogenous porphyrins from Helicobacter pylori. Biophysical Chemistry, 229, 25–30. https://doi.org/10.1016/j.bpc.2017.06.006
Choi, S., Lee, H., & Chae, H. (2012). Comparison of in vitro photodynamic antimicrobial activity of protoporphyrin IX between endoscopic white light and newly developed narrowband endoscopic light against Helicobacter pylori 26695. Journal of Photochemistry and Photobiology B: Biology, 117, 55–60. https://doi.org/10.1016/j.jphotobiol.2012.08.015
Morici, P., Battisti, A., Tortora, G., Menciassi, A., Checcucci, G., Ghetti, F., & Sgarbossa, A. (2020). The in vitro photoinactivation of Helicobacter pylori by a Novel LED-based device. Frontiers in Microbiology, 11(283), 2020. https://doi.org/10.3389/fmicb.2020.00283.eCollection
Faraoni, P., Gnerucci, A., Ranaldi, F., Orsini, B., Romano, G., & Fusi, F. (2018). Side effects of intra-gastric photodynamic therapy: An in vitro study. Journal of Photochemistry and Photobiology B: Biology, 186, 107–115. https://doi.org/10.1016/j.jphotobiol.2018.07.010
Wilder-Smith, C. H., Wilder-Smith, P., Grosjean, P., van den Bergh, H., Woodtli, A., Monnier, P., Dorta, G., Meister, F., & Wagneries, G. (2002). Photoeradication of Helicobacter pylori using 5-aminolevulinic acid: Preliminary human studies. Lasers in Surgery and Medicine, 31, 18–22. https://doi.org/10.1002/lsm.10066
Ganz, R. A., Viveiros, J., Ahmad, A., Ahmadi, A., Khalil, A., Tolkoff, M. J., Nishioka, N. S., & Hamblin, M. R. (2005). Helicobacter pylori in patients can be killed by visible light. Lasers in Surgery and Medicine, 36, 260–265. https://doi.org/10.1002/lsm.20161
Lembo, A. J., Ganz, R. A., Sheth, S., Cave, D., Kelly, C., Levin, P., Kazlas, P. T., Baldwin, P. C., Lindmark, W. R., McGrath, J. R., & Hamblin, M. R. (2009). Treatment of Helicobacter pylori infection with intra-gastric violet light phototherapy: A pilot clinical trial. Lasers in Surgery and Medicine, 41, 337–344. https://doi.org/10.1002/lsm.20770
Li, Z., Ren, B., Tan, H., Liu, S., Wang, W., Pang, Y., Lin, J., & Zeng, C. (2016). Capsule design for blue light therapy against Helicobacter pylori. PLoS ONE, 11(1), e0147531.
Vasilakakis, M. D., Koulaouzidis, A., Marlicz, W., & Iakovidis, D. K. (2020). The future of capsule endoscopy in clinical practice: From diagnostic to therapeutic experimental prototype capsules. Gastroenterology Review, 15(3), 179–193.
Tortora, G., Orsini, B., Pecile, P., Menciassi, A., Fusi, F., & Romano, G. (2016). An ingestible capsule for the photodynamic therapy of Helicobacter pylori infection. IEEE/ASME Transactions on Mechatronics, 21, 1935–1942. https://doi.org/10.1109/TMECH.2016.2536944
Romano, G., Tortora, G., Calusi, S., Orsini, B., Gnerucci, A., & Fusi, F. (2016). Minimally invasive ingestible device to perform anti-bacterial phototherapy in the stomach. Physica Medica, 32, 215.
Gnerucci, A., Faraoni, P., Calusi, S., Fusi, F., & Romano, G. (2020). Influence of stomach mucosa tissue on the efficacy of intragastric antibacterial PDT. Photochemistry Photobiology Sciences, 19, 34–39. https://doi.org/10.1039/c9pp00315k
O’Grady, J., Murphy, C. L., Barry, L., Shanahan, F., & Buckley, M. (2020). Defining gastrointestinal transit time using video capsule endoscopy: A study of healthy subjects. Endoscopy International Open, 8(3), E396–E400.
Lian, W. C., Hsiao, H. C., & Chou, C. C. (2003). Viability of microencapsulated bifidobacteria in simulated gastric juice and bile solution. International Journal of Food Microbiology, 86, 293–301. https://doi.org/10.1016/s0168-1605(02)00563-9
McCarthy, T. (2004). Veterinary Endoscopy for the Small Animal Practitioner. Elsevier Saunders.
Frandson, R. D., Lee, W. W., & Fails, A. D. (2009). Anatomy and Physiology of Farm Animals (7th ed.). Wiley-Blackwell.
Maiti, K. S., & Apolonski, A. (2021). Monitoring the reaction of the body state to antibiotic treatment against Helicobacter pylori via infrared spectroscopy: a case study. Molecules, 26, 3474. https://doi.org/10.3390/molecules26113474
Romano, G., Calusi S., Gnerucci A., Orsini B., Faraoni P., Tortora G., Menciassi A., Fusi F. (2016). Optical modelling of the gastric tissue to optimize the phototherapy against H. pylori infection, 18th Italian National Conference on Photonic Technologies (Fotonica 2016). doi: https://doi.org/10.1049/cp.2016.0946
Baccani, I., Faraoni, P., Marini, M., Gnerucci, A., Orsini, B., Pecile, P., Romano, G., Fusi, F., Rossolini, G. M., & Antonelli, A. (2019). Synergistic effect of photodynamic therapy at 400 nm and doxycycline against Helicobacter pylori. Future Microbiology, 14, 1199–1205. https://doi.org/10.2217/fmb-2019-0129
Acknowledgements
The authors would like to thank Eng. Paolo Grandi from Laboratori Victoria srl for help with the capsule programming, temperature and voltage monitoring, Mr. Gianni Paoli, Probiomedica srl, for help with prototype production and Eng. Giuseppe Tortora, Scuola Superiore Sant’Anna, Pisa for the thermal image of the capsule.
Funding
Open access funding provided by Università degli Studi di Firenze within the CRUI-CARE Agreement. This research was supported by the project “Capsulight” (PAR FAS 2007–2013, action line 1.1–1.1.2)—Tuscany Regional Board and by the project “Device endoscopico per foto-terapia antibatterica intragastrica”, Fondazione Cassa di Risparmio di Firenze.
Author information
Authors and Affiliations
Contributions
Conceptualization: SB, FF, BO, GR, FR, and SM; methodology: SB, FF, CT, AD, GR, FR, BO, and SM; formal analysis and investigation: SB, SB, PF, CT, AD, FF, GR, GM, BO, FR, FR, and PT; writing—original draft preparation: BO, PF, AG, GR, FR, and SB; writing—review and editing: BO, PF, AG, CT, AD, GR, and FF; funding acquisition: FF, GR, and BO; supervision: FF, GR, and BO.
Corresponding author
Ethics declarations
Conflict of interest
GR, FF and BO acknowledge being also Probiomedica srl.
Ethics approval
This study was approved by the local Ethical Committee (CNR—Centre for Experimental Biomedicine, Pisa, Italy).
Consent to participate
All the authors gave their consent to participate.
Consent for publication
All the authors gave their consent to publish.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Orsini, B., Busechian, S., Faraoni, P. et al. Ingestible light source for intragastric antibacterial phototherapy: a device safety study on a minipig model. Photochem Photobiol Sci 22, 535–547 (2023). https://doi.org/10.1007/s43630-022-00333-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43630-022-00333-w