Abstract
Objective
This study aimed to determine the short- and medium-term outcomes of hip dislocation in infants who failed Pavlik harness therapy and were subsequently treated with brace, closed reduction (CR) or open reduction (OR) before 6 months of age.
Methods
Fifty infants (66 hip dislocations) who failed Pavlik harness therapy between 2000 and 2018 and were treated with a rigid abduction brace or undergoing a CR or OR/cast were evaluated. All demographic data obtained from the medical system, developments and complications during the follow-up and treatment process were recorded and evaluated.
Results
Fifty infants (66 hips) with dislocated hips failed Pavlik harness therapy. Of these, 9 infants (12 hips) underwent rigid abduction splint therapy: 9 hips were successful, 2 hips had CR and 1 had OR. Thirty-eight infants (51 hips) had index CR, of which 3 (3 hips) failed and had OR. Radiographs of 49 hips (44 patients) were normal at the final evaluation. Pavlik harness therapy starting after 3 weeks (P = 0.028) and unilateral dislocations (P = 0.028) increased the risk of needing operating room. There was an association between OR and avascular necrosis (P = 0.025), but not between OR and other complications—dysplasia and re-dislocation/subluxation (P = 0.257 and P = 0.508, respectively).
Conclusion
Closed treatment of hip dislocation is possible in most babies who fail Pavlik treatment. Babies who are started on Pavlik therapy after 3 weeks of age may be at increased risk of needing an operating room.
Level of Evidence
IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The goal of treatment for developmental dysplasia of the hip (DDH) is to anatomically reduce the hip joint as soon as possible to maintain normal development of the acetabulum and proximal femur. This early concentric reduction helps reduce the risk of acetabular or femoral dysplasia and gives the patient the best chance of a functional hip joint for life [1,2,3]. The later the diagnosis is made, the higher the complexity of interventions and the higher the risk of complications and the lower the chance of success [2,3,4,5].
Avascular necrosis (AVN) after DDH treatment is the most problematic complication in the long term. This complication can cause proximal femoral growth impairment and degenerative joint disease. AVN is a treatment-related complication [3, 6, 7]. Higher rates of AVN rates are reported in the literature after unsuccessful Pavlik harness treatment, in those who applied Pavlik harness after 6 weeks, in fixed dislocations, and in bilateral cases [3,4,5,6,7].
Failure of the Pavlik harness typically requires intervention in the form of CR or open reduction (OR) to achieve concentric reduction of the hip [1]. If the hip cannot be reduced with closed treatment in DDH, surgical treatment is indicated [8, 9]. During the follow-up of patients, additional corrective surgeries may be required for complications such as re-dislocation and residual acetabular dysplasia [4, 5].
The literature highlights the incidence of failure of Pavlik harness therapy for DDH, the variability in diagnosis and treatment outcomes in these failed hips, the lack of standardized management protocols, and the need for stronger supporting evidence [8, 9]. Failure of Pavlik harness therapy is observed especially in dislocated hips at rest [10, 11]. Therefore, we included only dislocated hips confirmed by dynamic ultrasonography in this study.
The aim of this study was to evaluate consecutive cases of hip dislocation (confirmed by dynamic ultrasound) infants at our institution who failed Pavlik harness therapy between 2000 and 2018, and to determine the short- and medium-term outcomes after treatment with subsequent support, CR, or OR.
Methods
Our hospital's institutional review board approved this retrospective study (2019/1445214-Nemours Office of Human Subjects Protection). Informed consent forms were obtained from all patients participating in the study. A total of 124 (170 hips) consecutive infants with hip dislocations treated with Pavlik harnesses between January 2000 and December 2018 were evaluated. Demographic data were obtained from the patient medical records (Epic Systems, Verona, WI, USA). Patients diagnosed with hip dislocation by dynamic ultrasonography less than 6 months old, patients who underwent Pavlik harness therapy, and patients with adequate clinical and imaging follow-up for at least 2 years after the last intervention were included in this study. We excluded all syndromic dislocated hips that developed secondary to arthrogryposis, myelodysplasia, or other neuromuscular or syndromic abnormalities. Patients who were treated in other facilities before coming to our institution were also excluded from the study.
All Ortolani and Barlow examinations were performed by experienced pediatric orthopedic surgeons. Dynamic hip ultrasound was performed by pediatric radiologists using real-time sonographic equipment with 7.5-MHz linear array transducers using the technique described by Harcke and Grissom [12].
Pavlik harness treatment was started in the outpatient clinic immediately after the diagnosis of dislocation was made in all babies by clinical and ultrasonography. During the Pavlik harness treatment, the infants were followed both clinically and ultrasonographically. Pavlik harness therapy failure was defined as failure of progressive hip reduction exceeding 3 weeks after initiation of Pavlik therapy. The use of the Pavlik harness was discontinued and alternative rhino abduction braces or surgical interventions were applied according to the surgeon's preference. Ultrasound examination was performed on the reduced hips at (approximately) 3-week intervals and Pavlik harness was continued until sonographic stability was demonstrated on dynamic ultrasonography and the acetabulum returned to normal on ultrasonography.
Some patients were placed in a rigid abduction brace at the discretion of the treating surgeon. All other children were taken to the operating room for surgical reduction of the hip, either CR or OR. For hips where the Pavlik harness failed, we used an algorithmic approach to surgically reduction the hip. According to the hip arthrogram findings, all patients underwent CR with adductor tenotomy under anesthesia. If the reduction was considered acceptable and stable (according to the “safe zone” defined by Ramsey et al. [13] a spica cast was applied within the safe zone. Indications for open reduction included non-concentric, narrow safe zone. If there was (<20°) abduction or if excessive (>60°) abduction was required to keep the hip in reduction, open reduction was performed (in all cases) using an anterior approach in the same operating setting.
In the postoperative period, the hips were immobilized with a hip spica cast for at least 6 weeks. Hip position and development were then monitored using pelvic radiography every 4–6 months for the first 12 months and annually thereafter. Residual acetabular dysplasia was based on the acetabular index for age [14]. The diagnosis of AVN was made according to Salter's criteria [15]. The severity of AVN of the femoral head was assessed and classified as described by Kalamchi and MacEwen, and only grades 2 to 4 AVN were analyzed as significant [16].
Comparisons between index CR and index OR treatment were made to identify risk factors for patients requiring OR and CR. We evaluated the rates of residual dysplasia or AVN associated with different treatment modalities. All procedures performed for these complications were recorded.
Statistical Analysis
Parametric and non-parametric analyzes were performed. Descriptive and frequency statistics were used to describe the population with mean and standard deviation. Statistical analysis was performed using SPSS v.25 (IBM, Armonk, NY, USA). Statistical comparisons between patients undergoing OR and CR were made using an appropriately unpaired t-test, Chi-square test, or Fisher's exact test. The statistical significance of the risk factors was evaluated at the 0.05 level.
Results
One hundred and twenty-four (170 hip) consecutive infants with hip dislocation on both clinical and dynamic ultrasound evaluation were initially treated with a Pavlik harness and followed for at least 2 year over an 18-year period. Of these, 50 infants (66 hips, 38.8%) failed in Pavlik harness therapy. Figure 1 shows details of patient treatment modalities. The distribution of demographic characteristics of patients requiring intervention is detailed in Table 1. Twenty-three hips were reducible, but 43 were not, and intervention consisting of a rigid abduction brace, CR or OR was performed.
Nine infants (12 hips) were treated with rigid abduction braces. The abduction orthosis was successful in stabilizing 9 hips (6 patients); however, in 3 hips (3 patients), the abduction orthosis failed to stabilize/dislocate; Operative CR in 2 hips and operative OR in 1 hip were performed. Fifty-seven hips in the remaining 41 patients were successfully treated with either CR (48 hips) or OR (9 hips) (Table 2). Thirty-eight infants (51 hips) had index CR and subsequent Spica cast. Three hips failed CR and OR was performed via anterior approach and subsequent Spica casting (Table 2).
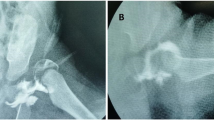
During the 6.72 ± 4.85 years follow-up of these patients, at least one complication developed in 12 hips of 10 patients, and 10 hips required additional surgical procedures (OR and/or reconstruction with femoral and/or pelvic osteotomy) (Figs. 2, 3). Complications in the CR and OR groups are detailed in Table 3.
The incidence of AVN after failed Pavlik harness therapy was 10.5% (6/57); 1.0% (1/104) after successful Pavlik harness therapy. In statistical evaluation, starting Pavlik harness treatment after 3 weeks increased the OR requirement (P = 0.028). Unilateral dislocation was also a risk factor for OR (P = 0.028) (Table 4). While an association was noted between OR and AVN (P = 0.025), we did not find any association between OR and other complications, including dysplasia and re-dislocation/subluxation (P = 0.257 and 0.508, respectively). There was a statistically significant correlation between OR due to existing complications and the need for additional surgery (P = 0.007) (Table 3). There was no significant relationship between AVN and unilaterality and age at initiation of Pavlik harness therapy (P = 0.624 and P = 0.376, respectively).
Discussion
This study comprised a large cohort of patients investigating initial Pavlik harness therapy in 124 consecutive infants (170 hips) with significant hip dislocation confirmed by sonographic examination at diagnosis. Our failure rate of 33.6% is among the lowest reported in the literature for the most severe form of DDH [10, 17,18,19]. The type of hip dislocation may also have affected this rate. In our series, 57 hip interventions were required in 44 patients.
Rigid abduction support in patients failing Pavlik harness therapy
Hedequist et al. [20] reported that 14 hips (13 Ortolani positive and 1 Barlow positive) were treated with rigid abduction orthosis after unsuccessful Pavlik harness therapy. Eleven of 14 hips were successfully treated, and the remaining three hips (2 patients) had successful CR. On the contrary, Abraham et al. [8] pavlik reported that all seven patients with dislocated/dislocated hips who failed Pavlik harness therapy also failed in the rigid abduction brace; of these patients, 4 had successful CR and 3 required OR. Novias et al. [11] Pavlik harness failed in 21 (26.9%) of 78 Ortolani hips, and 9 (42.9%) of them were treated with a rigid abduction brace, 4 of them CR and 8 of them OR. Similarly, Gornitzky et al. [21] reported a multicenter study of 38 patients (49 hips) who failed Pavlik harness therapy. Of these, 44.9% (22/49) were successfully treated with a rigid abduction brace. Similarly, the success rate of the abduction brace in our study was quite high with 75.0% (9/12). It failed in three of four reduced hips and one of eight reduced hips. However, a rigid abduction brace was not applied to all patients who failed Pavlik harness therapy.
Subsequent Treatment of Patients Failing Pavlik Harness Therapy
Arneill et al. [22] reported their cohort of 67 hips that had recently failed the Pavlik treatment. They were able to perform CR in 46 (68.7%) of 67 hips, of which 11 hips were reduced, giving them a successful CR percentage of 52.2% (35/67 hips). Aarvold et al. [10] reported that Pavlik harness therapy failed in 19 (39.6%) of 48 dislocated, irreducible hips that were subsequently successfully treated with CR (7 hips) or OR (12 hips). Two hips developed AVN—1 managed with CR and 1 managed with OR. In a similar cohort that included 166 hips of 154 patients, Talati et al. [9] reported nonoperative treatment failure in 81 hips of 68 patients. Overall, 34 (42.0%) of these hips required an operating room. Only Graf III and IV classification has been identified as an important determinant for OR need. These authors found that age and duration of orthotic treatment did not affect the choice of reduction technique [9]. In another study, the Pavlik harness failure rate was found to be 14.0% (30/215) for all DDH types, and the OR requirement was reported to be 26.7% [11]. In a study involving Ortolani-positive neonates, the authors found that the Pavlik harness failed to reduce and stabilize the hip 25.8% (8/31) of which 2 were treated with CR and 6 required OR. They also reported that AVN developed in the femoral head in 2 of 6 cases with OR. Gornitzky et al. [21]. of the failed Pavlik harness treatment cohort, 77.6% reported successful treatment using closed methods (44.9% rigid abduction brace and 32.7% CR), and 20.4% went to the operating room (Table 5). Senaran et al. [7] stated that only 2 (5.7%) of the 35 hips Pavlik failed needed surgery. Of the 44 patients in our cohort who required operating room, 38 (86.3%) had successful reduction with CR and 6 (13.7%) with OR. We attribute this success rate to the early age of reduction, but this must be carefully balanced with concerns about the effect of anesthesia on the developing brain.
Avascular Necrosis After Unsuccessful Pavlik Harness Therapy
After failure of Pavlik harness therapy, the incidence of AVN in cases with success with other treatment modalities ranges from 14.0 to 33.0% in most large series [6, 7, 20, 23]. Tiruveedhula et al. [6] reported that CR was required in 20 (54.1%) of 37 hips that failed Pavlik harness therapy, and OR was present in 17 of them at 10-year follow-up. They found the overall AVN rate to be 27.0% and stated that the reduction technique did not affect it. They reported that the risk of AVN was 4 times higher than in patients who presented late after unsuccessful Pavlik harness treatment and underwent surgical treatment alone [6]. In our study, although there was no significant difference between the CR and OR groups in terms of the duration of Pavlik harness use, we found that the AVN rate was significantly higher in the OR group, but the numbers in the OR group were very low. We attribute this to the fact that these are the hips most severely affected and cannot be closed. We found that the duration of use of Pavlik harness therapy did not affect the mode of reduction (P = 0.697), but treatment started after 3 weeks was a risk factor for OR (P = 0.028). Interestingly, unilateralism was also a risk factor for OR (P = 0.028), although this is probably related to sample size.
Sankar et al. [4] included 78 patients younger than 12 months (87 hips), with a median age at first CR of 8 months. In 79 hips (91%), CR was initially successful, but 79 hips (8.9%) had hip redislocate and required OR. During the short-term follow-up (12–36 months), 8 out of 72 (11.1%) hips with successful CR reported acetabular and/or femoral osteotomy for residual dysplasia and 18 out of 72 AVN (25.0% hips). They found no relationship between the development of AVN and previous brace use and CR age [4]. In our study, which had a mean follow-up of 6.72 years, successful CR was achieved in 48 of 51 hips and additional surgery (femoral and/or pelvic osteotomy) was achieved in 6 hips (12.5%). On the other hand, four of six patients with OR initially underwent surgical intervention. Considering the difference in follow-up periods in this study [4], our AVN rate is relatively lower, at 10.5%.
Our data also show that dislocated hips in infants less than 6 months of age are less likely to fail CR [5.9% (3/51)] and require an operating room [15.8% (9/57)] at index surgery. Young age at CR (122.26 ± 72.36 days) in these patients likely contributed to the high success rate of CR. Infants with unilateral disease who were started on Pavlik harness therapy after 3 weeks of age were more likely to have OR. As in previous series, we did not find a significant relationship between Pavlik harness treatment time and the need for CR and OR [17, 24]. Liu et al. [25] stated that the use of the Pavlik harness in patients treated with CR/OR before 6 months significantly reduced the need for surgery, but had no effect on complications in the follow-up.
Due to the retrospective nature of this study, there are some limitations that prevent coherent decisions regarding the discontinuation of the Pavlik harness. However, Pavlik harness time is consistent with most large studies. Also, the mean follow-up is only 6.72 years, which would probably preclude us from getting a good idea of the true prevalence of AVN or proximal femoral growth disorders due to treatment factors. However, follow-up is sufficient so that we can catch more severe/clinically relevant AVN cases and assess the possibility of needing early reconstructive surgery for acetabular dysplasia. The uniformity of the cohort in terms of severity of ultrasound-documented hip dislocation and age less than 6 months at the initial evaluation prior to starting Pavlik therapy allows us to meaningfully compare the results of abduction support, CR, and OR.
Conclusion
Based on the available data, we recommend that families of infants <6 months of age with hip dislocation/unreducible who fail Pavlik harness therapy be consulted about the high success rate and low complications of closed therapy in the medium term.
References
Harding, M. G., Harcke, H. T., Bowen, J. R., Guille, J. T., & Glutting, J. (1997). Management of dislocated hips with Pavlik harness treatment and ultrasound monitoring. Journal of Pediatric Orthopedics, 17, 189–198.
Murray, T., Cooperman, D. R., Thompson, G. H., & Ballock, R. T. (2007). Closed reduction for treatment of developmental dysplasia of the hip in children. American Journal of Orthopedics (Belle Mead, N.J.), 36, 82–84.
Bache, C. E., Graham, H. K., Dickens, D. R., Donnan, L., Johnson, M. B., Nattrass, G., et al. (2008). Ligamentum teres tenodesis in medial approach open reduction for developmental dislocation of the hip. Journal of Pediatric Orthopedics, 28, 607–613.
Sankar, W. N., Gornitzky, A. L., Clarke, N. M. P., Herrera-Soto, J. A., Kelley, S. P., Matheney, T., et al. (2019). Closed reduction for developmental dysplasia of the hip: Early-term results from a prospective, multicenter cohort. Journal of Pediatric Orthopedics, 39, 111–118.
Li, Y., Xu, H., Li, J., Yu, L. J., Liu, Y. Z., Southern, E., et al. (2015). Early predictors of acetabular growth after closed reduction in late detected developmental dysplasia of the hip. Journal of Pediatric Orthopedics. Part B, 24, 35–39.
Tiruveedhula, M., Reading, I. C., & Clarke, N. M. (2015). Failed Pavlik harness treatment for DDH as a risk factor for avascular necrosis. Journal of Pediatric Orthopedics, 35, 140–143.
Senaran, H., Bowen, J. R., & Harcke, H. T. (2007). Avascular necrosis rate in early reduction after failed Pavlik harness treatment of developmental dysplasia of the hip. Journal of Pediatric Orthopedics, 27, 192–197.
Ibrahim, D. A., Skaggs, D. L., & Choi, P. D. (2013). Abduction bracing after Pavlik harness failure: An effective alternative to closed reduction and spica casting? Journal of Pediatric Orthopedics, 33, 536–539.
Talathi, N. S., Trionfo, A., Patel, N. M., Upasani, V. V., Matheney, T., Mulpuri, K., et al. (2020). Should I plan to open? Predicting the need for open reduction in the treatment of developmental dysplasia of the hip. Journal of Pediatric Orthopedics, 40, e329–e334.
Aarvold, A., Schaeffer, E. K., Kelley, S., Clarke, N. M. P., Herrera-Soto, J. A., Price, C. T., et al. (2019). Management of irreducible hip dislocations in infants with developmental dysplasia of the hip diagnosed below 6 months of age. Journal of Pediatric Orthopedics, 39, e39–e43.
Novais, E. N., Kestel, L. A., Carry, P. M., & Meyers, M. L. (2016). Higher Pavlik harness treatment failure is seen in Graf type IV Ortolani-positive hips in males. Clinical Orthopaedics and Related Research, 474, 1847–1854.
Harcke, H. T., & Grissom, L. E. (1990). Performing dynamic sonography of the infant hip. AJR American Journal of Roentgenology, 155, 837–844.
Ramsey, P. L., Lasser, S., & MacEwen, G. D. (1976). Congenital dislocation of the hip. Use of the Pavlik harness in the child during the first six months of life. The Journal of Bone & Joint Surgery American, 58, 1000–1004.
Tönnis, D. (1976). Normal values of the hip joint for the evaluation of X-rays in children and adults. Clinical Orthopaedics and Related Research, 119, 39–47.
Salter, R. B., Kostuik, J., & Dallas, S. (1969). Avascular necrosis of the femoral head as a complication of treatment for congenital dislocation of the hip in young children: A clinical and experimental investigation. Canadian Journal of Surgery, 12, 44–61.
Kalamchi, A., & MacEwen, G. D. (1980). Avascular necrosis following treatment of congenital dislocation of the hip. Journal of Bone and Joint Surgery. American Volume, 62, 876–888.
Viere, R. G., Birch, J. G., Herring, J. A., Roach, J. W., & Johnston, C. E. (1990). Use of the Pavlik harness in congenital dislocation of the hip. An analysis of failures of treatment. The Journal of Bone & Joint Surgery American, 72, 238–244.
Atalar, H., Sayli, U., Yavuz, O. Y., Uraş, I., & Dogruel, H. (2007). Indicators of successful use of the Pavlik harness in infants with developmental dysplasia of the hip. International Orthopaedics, 31, 145–150.
Lerman, J. A., Emans, J. B., Millis, M. B., Share, J., Zurakowski, D., & Kasser, J. R. (2001). Early failure of Pavlik harness treatment for developmental hip dysplasia: Clinical and ultrasound predictors. Journal of Pediatric Orthopedics, 21, 348–353.
Hedequist, D., Kasser, J., & Emans, J. (2003). Use of an abduction brace for developmental dysplasia of the hip after failure of Pavlik harness use. Journal of Pediatric Orthopedics, 23, 175–177.
Gornitzky, A. L., Schaeffer, E. K., Price, C. T., Sankar, W. N., International Hip Dysplasia Institute. (2018). International Hip Dysplasia Institute Pavlik harness disease revisited: Does prolonged treatment of a dislocated hip in a harness adversely affect the α angle? Journal of Pediatric Orthopaedics, 38, 297–304.
Arneill, M., Cosgrove, A., & Robinson, E. (2021). Should closed reduction of the dislocated hip be attempted after failed Pavlik harness treatment in developmental dysplasia of the hip? Bone & Joint Open, 2, 584–588.
Inoue, T., Naito, M., & Nomiyama, H. (2001). Treatment of developmental dysplasia of the hip with the Pavlik harness: Factors for predicting unsuccessful reduction. Journal of Pediatric Orthopedics. Part B, 10, 186–191.
Jones, G. T., Schoenecker, P. L., & Dias, L. S. (1992). Developmental hip dysplasia potentiated by inappropriate use of the Pavlik harness. Journal of Pediatric Orthopedics, 12, 722–726.
Liu, Y., Kan, L., Sun, J., & Zhang, Y. (2022). Impact of failed Pavlik harness treatment on the outcomes following closed or open reduction in developmental dysplasia of the hip. Indian Journal of Orthopaedics, 56, 1634–1639.
Funding
None declared.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
None declared.
Ethics Committee Approval
Ethical committee approval was received from Office of Human Subjects Protection,
Informed Consent
All patients gave their consent and the study was approved by the Hospital’s ethics committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Imerci, A., Thacker, M.M. & Bowen, J.R. Failure of Pavlik Harness Treatment in Infants Under 6 Months Old with Dislocated Hips: Short- and Intermediate-Term Results of Subsequent Treatment Modalities. JOIO 58, 1288–1296 (2024). https://doi.org/10.1007/s43465-024-01162-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-024-01162-y