Abstract
Background
The reduction and fixation of Medial humeral calcar is difficult in the treatment of elderly proximal humerus Neer 3 and 4-part fractures with a single lateral locking plate. Our study investigated the efficacy of an intramedullary calcar supporting plate combined with a lateral locking plate for the treatment of 3- and 4-part fractures of the proximal humerus in the elderly through a deltoid splitting approach.
Methods
From June 2022 to December 2022, we treated six elderly patients with Neer 3 and 4-part fractures using proximal humeral intramedullary calcar support plate in combination with lateral locking plate through a deltoid splitting approach. Follow-up time was 6–12 months. Assessment indicators included fracture union, quality of reduction, and complication rate. The Constant-Murley score was used to record shoulder function at 6 months postoperatively.
Results
All 6 patients showed fracture union and anatomic reduction. Constant-Murley score was 79.5 (70–90) at 6 months postoperatively. There was no incision non-healing, internal fixation failure, bone non-union or surgical site infection, secondary surgery, or death. Shoulder impingement occurred in 1 case.
Conclusion
Proximal humeral intramedullary calcar support plate combined with lateral locking plate fixation through a deltoid splitting approach can effectively maintain fracture reduction, prevent inversion collapse of humeral head and internal fixation failure, and provide satisfactory clinical results at an early stage.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Proximal humeral fractures (PHFs) are adults’ seventh most frequent fractures [1]. Several studies have shown that prevalence varies from 4 to 10% of all fractures [2]. A linear increase in the incidence is present in the elderly population (> 65 years) [3,4,5]. According to Neer classification, most nondisplaced proximal humerus fractures can be treated nonoperatively. However, displaced fractures require surgery. However, surgery is recommended for displaced and 3 or 4-part fractures. Commonly used surgical methods are closed reduction and intramedullary nailing (CRIF), open reduction and internal fixation (ORIF), hemiarthroplasty (HA) and reverse shoulder arthroplasty (RSA) [6]. Among them, the proximal humeral locking plate is widely used in the treatment of proximal humeral fractures. However, for unstable, varus-displaced complex fractures of the proximal humerus, especially for elderly Neer 3 and 4-part fractures, surgical fixation is still challenging, and there is still a high incidence of postoperative complications [7,8,9,10]. Several studies have reported that lack of medial support is a predictor of failure after surgical fixation of proximal humeral fractures [11,12,13]. The double-plate technique has been used to improve the quality and stability of the reduction of the medial humeral calcar [14,15,16]. But this method requires stripping of more soft tissues and the blood supply around the fracture is difficult to preserve. Wang et al. [17] used a combined axillary approach and an anterolateral approach for direct reduction and fixation of the medial and lateral humeral columns.
Treatment of proximal humerus fractures via the deltoid approach has the advantages of easy visualization of the greater tuberosity and preservation of the branches of the anterior circumflex humeral artery. Intramedullary plates are used clinically for some special types of fractures to better protect the surrounding blood supply without an additional incision [18,19,20,21]. In this study, we used intramedullary calcar support plates combined with lateral locking plates via the deltoid approach to treat six cases of elderly Neer 3 and 4-part fractures with a satisfactory short-term clinical outcome at a follow-up of 6–12 months.
Materials and Methods
All experimental procedures were approved by the Ethics Committee of Guangdong Orthopedic Hospital. All aspects of this cohort of cases were conducted in accordance with the current version of the Declaration of Helsinki, the guidelines established by the International Conference on the Harmonization of Standardized Clinical Practice, and Chinese laws. All participants signed an informed consent form before registration.
Inclusion criteria: 1. Age ≥ 60; 2. Neer 3 and 4-part closed fractures.
Exclusion criteria: 1. Neer 1 and 2-part closed fracture; 2. Open fractures; 3. Old fractures (≥ 3 weeks); 4. Pathologic fractures; 5. Polytrauma; 6. Fractures with blood vessels or nerves requiring repair; 7. With severe shoulder osteoarthritis; 8. With Large and massive rotator cuff tears.
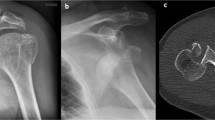
Data of patients with Neer 3 and 4-part fractures using proximal humeral intramedullary calcar support plate in combination with lateral locking plate through a deltoid splitting approach were analyzed retrospectively. All patients underwent a clinical examination to document their soft tissue condition and neurovascular status, particularly the axillary nerve. Radiologic evaluation included anteroposterior and lateral scapular X-rays of the shoulder, and fractures were classified according to the Neer classification. CT scans were performed on all patients for further evaluation of fractures. The basic data of these six cases are shown in Table 1. According to Neer classification, four cases were 3-part fractures, and two cases were 4-part fractures. All surgeries were performed by the Department of Shoulder and Elbow Surgery, The Third Affiliated Hospital of Southern Medical University.
Surgical Technique
Surgical methods: General anesthesia, beach chair lying position.
An anterolateral approach through the deltoid muscle. The incision was about 10 cm long. The anterior and middle bundles of the deltoid muscle were bluntly separated to expose the tuberosity fractures, and the vascular and nerve bundles composed of the axillary nerve and the posterior humeral circumflex artery and vein were separated and protected. The large and small tuberosities and attached tendonous tissues were fixed with pre-set sutures, and the lesser and greater tuberosities were retracted forward and backward, respectively to expose the medullary cavity between the humeral head and the greater and lesser tuberosities. Remove the humeral head, tuberosity and blood clots at the distal end of the fracture and the soft tissue embedded in the medullary cavity, and clearly reveal the fracture line of the medial calcar. The shape of the fracture line on the medial calcar side was observed, and the humeral head, and humeral shaft were anatomically reduced. A pre-bent 3-hole “T”-shaped locking plate was applied intramedullary to the calcar to fix the fractured end of the medial calcar. The medial calcar was well reset under X-ray fluoroscopy, the allogeneic freeze-dried femoral head was taken, trimmed into a bone block similar to the bone defect in the medullary cavity, and implanted in the proximal bone defect, and the large and small nodules were pulled with suture rings to reset the large and small nodules, Insert the 3-hole proximal humeral locking plate for temporary fixation. After the fluoroscopy is satisfactory, screws are driven to firmly fix the fracture fragments, and the large and small tuberosity fragments are firmly sutured to repair the rotator cuff tissue. The incision was flushed, a drainage tube was placed, the incision was closed, and the shoulder rest was abducted and fixed after the operation (Supplementary Fig. 2).
Postoperative Care and Follow-Ups
Postoperative X-ray examination of the shoulder. On the second day after the operation, the drainage tube was removed and the shoulder joint was passively moved with the assistance of the doctor. Isometric contraction exercises and elbow joint functional exercises were started within 1 week after the operation. Functional exercises were performed under the guidance of a rehabilitation specialist 2 weeks after the operation. Active activity training was started 1 month after the operation. After the postoperative review of the front and side of the shoulder, weight-bearing was allowed after the formation of the callus was observed.
We recorded the duration of surgery, the number of fluoroscopies, and blood loss. Patients were followed up every month postoperatively to record the complications (incisional complications, deep infection, screw penetration through the glenohumeral joint, shoulder impingement, internal fixation failure, avascular necrosis (AVN) of the humeral head, and reduction loss).
Radiographic Evaluation
Neer classification was determined from pre-operative radiographs. A fracture part is considered displaced if angulation exceeds 45°, or if the fracture is displaced by more than 1 cm [22]. Patients were followed up with postoperative X-rays to document the quality of fracture reduction, fracture union, and complications. Postoperative imaging evaluations were performed on shoulder X-rays, including fracture displacement distance and humeral neck-shaft angle (HNSA). Measurements were graded according to anatomic reduction, acceptable reduction and poor reduction [23] (Table 2). Grade Criteria: Overall anatomic reduction of fracture (all indicators reach anatomic reduction), approximate anatomic reduction (more than 1 parameter is non-anatomic, but no poor displacement), and fracture poor displacement group (1 or more parameters of poor displacement) [24,25,26].
Shoulder Function Score
The Constant-Murley Score (CMS) [27] is a multi-item functional scale assessing pain (15 scores), activities of daily living (ADL, 20 scores), range of motion (ROM, 40 scores) and strength of the affected shoulder (25 scores). Its score ranges from 0 to 100 points, representing the worst and best shoulder function, respectively.
Results
Six cases (5 females, 1 male; average age 70.8 years (60–80 years); 4 cases of right shoulder and 2 cases of left shoulder) with medial cortical defect were treated using intramedullary calcar support plate fixation and minimally invasive lateral locking plate fixation through a deltoid splitting approach. According to Neer classification, there were 4 of 3-part fracture and 2 of 4-part fracture. Quality of reduction, fracture union, complications and functional scores were recorded. The average postoperative hospitalization was 7.5 days (5–12 days) and average operative time was 151.7 min (130–190 min) (Table 1).
Postoperative follow-up ranged from 6 to 12 months. Anatomic reduction was achieved in all six patients. Shoulder impingement occurred in one patient who was performed subacromial injection therapy after fracture union. The average Constant-Murley score of at the final follow-up was 79.5 scores (70–90) (Table 3).
Discussion
Various surgical methods are available for the treatment of proximal humeral fractures, including percutaneous pin fixation, plate fixation, intramedullary nail fixation, and joint replacement. Treating Neer 3 and 4-part fractures of the proximal humerus in the elderly is challenging [6]. Some studies have shown that non-anatomic reduction, lack of medial support in proximal humeral fractures treated with plates, and disruption of blood supply at the fracture site are predictive factors for fixation failure [28,29,30]. Satisfactory reduction and support of the medial aspect of the proximal humerus reduce the risk of postoperative varus displacement, humeral head subsidence, and loss of neck-shaft angle [31,32,33,34,35]. Therefore, achieving a satisfactory reduction and fixation of the medial calcar of the proximal humerus plays a crucial role in the surgical management of proximal humeral comminuted fractures.
We used the approach through the anterior and middle bundles of the split deltoid muscle to achieve reduction and internal fixation of the fracture. In a cadaveric study, Gardner et al. [36, 37] reported that the anterior circumflex vessel courses directly in line with the deltopectoral approach. They confirmed that the surgical approach through the anterior deltoid raphe preserves both the anterior and posterior vascular supply to the humeral head. Rouleau et al. [38] suggested that the deltoid splitting approach offers full exposure of the lateral proximal humerus and has less impact on the anterior humeral circumflex artery. Bhayana et al. [39] believed that the deltoid splitting approach has advantages in achieving reduction and protecting the blood supply at the fracture site in Neer 3 and 4-part fractures of the proximal humerus involving the greater tuberosity. In this research, the displaced greater tuberosity provided a natural corridor for exposing the medial proximal humerus. When the deltoid splitting approach was used, the fracture can be clearly visualized by retracting the greater and lesser tuberosity posteriorly and anteriorly respectively, after the blood clots were removed. The intramedullary calcar support plate could be easily fixed under direct vision. After that, the connection between the humeral stem and the humeral head has been substantially stabilized, and the reduction of the fracture with a bone graft and a greater tuberosity becomes much easier, thereby minimizing the separation of the surrounding soft tissues. In our study, anatomic reduction was achieved in all six cases. Schnetzke et al. [40] demonstrated that anatomic reduction with a locked plate significantly improved the clinical outcome of unstable and displaced proximal humeral fractures involving the anatomic neck (10 of 30 patients with anatomic reduction). Habib et al. [41] reported that an overall anatomic or near-anatomic fracture reduction rate is 79.4% (27/34). Based on our experience, after the medial calcar of proximal humerus is reducted and fixed under a straight view using the intramedullary calcar support plate, the reduction of the humeral head can be effectively maintained. Then, reduction and fixation of the greater and lesser tuberosities can be easily performed, which reduces the surgical difficulty and improves the quality of fracture reduction in Neer 3and 4-part fractures.
All six patients showed fracture union and satisfactory reduction during follow-up. To make the humeral head well-supported and to minimize its collapse, allografts were performed after the placement of intramedullary calcar support plates, which were freeze-dried humeral heads. From a biomechanical perspective, the intramedullary calcar support plate, allograft, and lateral locking plate were used together to stabilize and support the proximal humeral fractures effectively. Some studies have used large autogenous/allogeneic fibular grafts to treat complex proximal humeral fractures [32, 42, 43], reducing postoperative reduction loss and increasing the fracture union rate compared to the control group. Our results are consistent with these studies. The average Constant-Murley score at the final follow-up was 79.5 scores (range from 70 to 90).
Attempts have also been made to make fixation of proximal humerus fractures more stable and to allow patients early functional shoulder exercise. Shen et al. [33] used calcar screws to provide angular stability and maintain humeral head reduction, with an average Constant-Murley score of 80.25. Knierzinger et al. [44] have used angular stable plates and additional screw-tip cement augmentation to increase the stability of the internal fixation complex, with an average Constant-Murley score of 76 ± 15 at 1 year postoperatively, significantly reducing the internal fixation failure rate. Warnhoff et al. [15] used a double-plate technique, with a one-third tubular plate placed in front of the lesser tuberosity to maintain support of the medial humeral head, resulting in a Constant-Murley score of 77 ± 17. Wang et al. [16] added a support plate at the humeral tuberosity through the axillary approach and implanted an outer locking plate through the deltoid splitting approach, achieving a Constant-Murley score of 82.8. The scores in our study were similar to those studies above (Figs. 1, 2).
Typical case 1. A 73-year-old woman sustained an unstable proximal humerus fracture (Neer 3-part) from a fall. The pre-operative X-ray and CT scan showed severe displacement of proximal humerus (A, B); The medial supporting plate was used (C); An allogenic allograft was inserted in the bony defect (D); Protection of the axillary nerve (E); Intraoperative X-ray (F, G); Closure of the lateral approach (H). Radiographs 1 month after surgery (I, J); Radiographs 6 months after surgery (K, L)
Typical case 2. An 80-year-old female patient suffered from right shoulder pain and limited mobility for 3 h due to a fall. The pre-operative X-ray and CT scan showed severe displacement of proximal humerus (A, B); The medial supporting plate was used (C); An allogenic allograft was inserted in the bony defect (D); Protection of the axillary nerve(E); Intraoperative X-ray (F, G)
Limitations
There are still several limitations in our study. First, this method is only applicable to Neer 3 and four-part fractures with clear displacement of the greater tuberosity, as it requires implantation of the intramedullary calcar support plate. Second, this is a retrospective study with a small number of cases and short follow-ups, which may not be sufficient to accurately assess the surgical long-term efficacy. Third, the biomechanical characteristics of the intramedullary calcar support plate have not been fully investigated. Therefore, we need to include more cases and perform further biomechanical studies, and design more scientific prospective controlled studies.
Conclusion
Proximal humeral intramedullary calcar support plate combined with lateral locking plate fixation through a deltoid splitting approach can effectively maintain proximal humeral fracture reduction, and prevent inversion collapse and internal fixation failure, and the early clinical results are satisfactory. This may be a novel method for the elderly Neer 3 and 4-part fractures.
Data Availability
Not applicable.
References
Iglesias-Rodríguez, S., Domínguez-Prado, D. M., García-Reza, A., Fernández-Fernández, D., Pérez-Alfonso, E., García-Piñeiro, J., et al. (2021). Epidemiology of proximal humerus fractures. Journal of Orthopaedic Surgery and Research, 16, 402.
Passaretti, D., Candela, V., Sessa, P., & Gumina, S. (2017). Epidemiology of proximal humeral fractures: A detailed survey of 711 patients in a metropolitan area. Journal of Shoulder and Elbow Surgery, 26, 2117–2124.
Bell, J. E., Leung, B. C., Spratt, K. F., Koval, K. J., Weinstein, J. D., Goodman, D. C., et al. (2011). Trends and variation in incidence, surgical treatment, and repeat surgery of proximal humeral fractures in the elderly. Journal of Bone and Joint Surgery American, 93, 121–131.
Kannus, P., Palvanen, M., Niemi, S., Sievänen, H., & Parkkari, J. (2009). Rate of proximal humeral fractures in older Finnish women between 1970 and 2007. Bone, 44, 656–659.
Palvanen, M., Kannus, P., Niemi, S., & Parkkari, J. (2006). Update in the epidemiology of proximal humeral fractures. Clinical Orthopaedics and Related Research, 442, 87–92.
Maier, D., Jaeger, M., Izadpanah, K., Strohm, P. C., & Suedkamp, N. P. (2014). Proximal humeral fracture treatment in adults. Journal of Bone and Joint Surgery, 96, 251–261.
Samborski, S. A., Haws, B. E., Karnyski, S., Soles, G., Gorczyca, J. T., Nicandri, G., et al. (2022). Outcomes for type C proximal humerus fractures in the adult population: Comparison of nonoperative treatment, locked plate fixation, and reverse shoulder arthroplasty. JSES International, 6, 755–762.
Konrad, G., Bayer, J., Hepp, P., Voigt, C., Oestern, H., Kääb, M., et al. (2010). Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. Journal of Bone and Joint Surgery, 92, 85–95.
Katthagen, J. C., Huber, M., Grabowski, S., Ellwein, A., Jensen, G., & Lill, H. (2017). Failure and revision rates of proximal humeral fracture treatment with the use of a standardized treatment algorithm at a level-1 trauma center. Journal of Orthopaedics and Traumatology, 18, 265–274.
Robinson, C. M., Stirling, P., Goudie, E. B., MacDonald, D. J., & Strelzow, J. A. (2019). Complications and long-term outcomes of open reduction and plate fixation of proximal humeral fractures. Journal of Bone and Joint Surgery American, 101, 2129–2139.
Lin, S. J., Tsai, Y. H., Yang, T. Y., Shen, S. H., Huang, K. C., & Lee, M. S. (2015). Medial calcar support and radiographic outcomes of plate fixation for proximal humeral fractures. BioMed Research International, 2015, 170283.
Krappinger, D., Bizzotto, N., Riedmann, S., Kammerlander, C., Hengg, C., & Kralinger, F. S. (2011). Predicting failure after surgical fixation of proximal humerus fractures. Injury, 42, 1283–1288.
Jung, W. B., Moon, E. S., Kim, S. K., Kovacevic, D., & Kim, M. S. (2013). Does medial support decrease major complications of unstable proximal humerus fractures treated with locking plate? BMC Musculoskeletal Disorders, 14, 102.
Michel, P. A., Raschke, M. J., Katthagen, J. C., Schliemann, B., Reißberg, I., & Riesenbeck, O. (2023). Double plating for complex proximal humeral fractures: clinical and radiological outcomes. Journal of Clinical Medicine, 12(2), 696.
Warnhoff, M., Jensen, G., Dey, H. R., Theruvath, P., Lill, H., & Ellwein, A. (2021). Double plating—surgical technique and good clinical results in complex and highly unstable proximal humeral fractures. Injury, 52, 2285–2291.
Wang, F., Wang, Y., Dong, J., He, Y., Li, L., Liu, F., et al. (2021). A novel surgical approach and technique and short-term clinical efficacy for the treatment of proximal humerus fractures with the combined use of medial anatomical locking plate fixation and minimally invasive lateral locking plate fixation. Journal of Orthopaedic Surgery and Research, 16, 29.
Wang, Q., Sheng, N., Rui, B., & Chen, Y. (2020). The neck-shaft angle is the key factor for the positioning of calcar screw when treating proximal humeral fractures with a locking plate. The Bone & Joint Journal, 102-B, 1629–1635.
Mast, J., Jakob, R., & Ganz, R. (1989). Planning and reduction technique in fracture surgery. Springer.
Russell, G. J., & Pearsall, A. W. (2002). Intramedullary plate fixation of a distal humerus fracture: A case report. Journal of Orthopaedic Trauma, 16, 353–356.
Zhang, J., Liang, J., Wang, J., & Tang, X. (2023). Fixation of the comminuted distal-femur fracture with intramedullary and extramedullary plates: A rare case report. Asian Journal of Surgery, 46(6), 2479–2480.
Gardenbroek, T. J., Oud, S., Formijne Jonkers, H. A., & Goslings, J. C. (2021). Supporting the medial hinge in proximal humerus fractures with an intramedullary plate. Trauma Case Reports, 33, 100474.
Neer, C. N. (1970). Displaced proximal humeral fractures. I. Classification and evaluation. Journal of Bone and Joint Surgery American, 52, 1077–1089.
Schnetzke, M., Bockmeyer, J., Porschke, F., Studier-Fischer, S., Grützner, P. A., & Guehring, T. (2016). Quality of reduction influences outcome after locked-plate fixation of proximal humeral type-C fractures. Journal of Bone and Joint Surgery American, 98, 1777–1785.
Solberg, B. D., Moon, C. N., Franco, D. P., & Paiement, G. D. (2009). Locked plating of 3- and 4-part proximal humerus fractures in older patients: The effect of initial fracture pattern on outcome. Journal of Orthopaedic Trauma, 23, 113–119.
Agudelo, J., Schürmann, M., Stahel, P., Helwig, P., Morgan, S. J., Zechel, W., et al. (2007). Analysis of efficacy and failure in proximal humerus fractures treated with locking plates. Journal of Orthopaedic Trauma, 21, 676–681.
Jung, S. W., Shim, S. B., Kim, H. M., Lee, J. H., & Lim, H. S. (2015). Factors that influence reduction loss in proximal humerus fracture surgery. Journal of Orthopaedic Trauma, 29, 276–282.
Constant, C. R., & Murley, A. H. (1987). A clinical method of functional assessment of the shoulder. Clinical Orthopaedics and Related Research, 214, 160–164.
Clement, N. D., Duckworth, A. D., McQueen, M. M., & Court-Brown, C. M. (2014). The outcome of proximal humeral fractures in the elderly: predictors of mortality and function. Bone Joint J, 96-B, 970–977.
Hardeman, F., Bollars, P., Donnelly, M., Bellemans, J., & Nijs, S. (2012). Predictive factors for functional outcome and failure in angular stable osteosynthesis of the proximal humerus. Injury, 43, 153–158.
Gardner, M. J., Weil, Y., Barker, J. U., Kelly, B. T., Helfet, D. L., & Lorich, D. G. (2007). The importance of medial support in locked plating of proximal humerus fractures. Journal of Orthopaedic Trauma, 21, 185–191.
Chen, H., Zhu, Z., Li, J., Chang, Z., & Tang, P. (2020). Finite element analysis of an intramedulary anatomical strut for proximal humeral fractures with disrupted medial column instability: A cohort study. International Journal of Surgery, 73, 50–56.
Wang, Q., Sheng, N., Huang, J. T., Zhu, H., Tuerxun, M., Ruan, Z., et al. (2023). Effect of fibular allograft augmentation in medial column comminuted proximal humeral fractures: a randomized controlled trial. Journal of Bone and Joint Surgery American, 105, 302–311.
Ponce, B. A., Thompson, K. J., Raghava, P., Eberhardt, A. W., Tate, J. P., Volgas, D. A., et al. (2013). The role of medial comminution and calcar restoration in varus collapse of proximal humeral fractures treated with locking plates. Journal of Bone and Joint Surgery American, 95, e113(1-7).
Shen, P., Zhu, Y., Zhu, L., Li, X., & Xu, Y. (2019). Effects of medial support screws on locking plating of proximal humerus fractures in elderly patients: A retrospective study. Annals of Translational Medicine, 7, 560–560.
Shin, W. C., Kang, S., Son, S. M., Seo, J. S., & Choi, M. H. (2022). High bone union rate using a locking plate for proximal humeral fractures in patients older than 70 years: Importance of the medial column. European Journal of Trauma and Emergency Surgery, 48, 2937–2942.
Gardner, M. J., Griffith, M. H., Dines, J. S., & Lorich, D. G. (2004). A minimally invasive approach for plate fixation of the proximal humerus. Bulletin/Hospital for Joint Diseases, 62, 18–23.
Gardner, M. J., Voos, J. E., Wanich, T., Helfet, D. L., & Lorich, D. G. (2006). Vascular implications of minimally invasive plating of proximal humerus fractures. Journal of Orthopaedic Trauma, 20, 602–607.
Rouleau, D. M., Balg, F., Benoit, B., Leduc, S., Malo, M., Vézina, F., et al. (2020). Deltopectoral vs. deltoid split approach for proximal HUmerus fracture fixation with locking plate: a prospective RAndomized study (HURA). Journal of Shoulder and Elbow Surgery, 29, 2190–2199.
Bhayana, H., Chouhan, D. K., Aggarwal, S., Prakash, M., Patel, S., Arora, C., et al. (2022). Outcomes of plate osteosynthesis for displaced 3-part and 4-part proximal humerus fractures with deltopectoral vs. deltoid split approach. European Journal of Trauma and Emergency Surgery, 48, 4559–4567.
Schnetzke, M., Bockmeyer, J., Loew, M., Studier-Fischer, S., Grützner, P. A., & Guehring, T. (2018). Rate of avascular necrosis after fracture dislocations of the proximal humerus: Timing of surgery. Obere Extremitat, 13, 273–278.
Habib, N., Fornaciari, P., Thuerig, G., Maniglio, M., Tannast, M., & Vial, P. (2021). Hinge plate technique for osteosynthesis of comminuted proximal humeral fractures. Injury, 52, 2292–2299.
Chow, R. M. M., Begum, F. B., Beaupre, L. A. P., Carey, J. P. P., Adeeb, S. P., & Bouliane, M. J. M. (2012). Proximal humeral fracture fixation: Locking plate construct ± intramedullary fibular allograft. Journal of Shoulder and Elbow Surgery, 21, 894–901.
Bilgin, S. S. (2012). Reconstruction of proximal humeral defects with shoulder arthrodesis using free vascularized fibular graft. The Journal of Bone & Joint Surgery, 94, e94.
Knierzinger, D., Crepaz-Eger, U., Hengg, C., & Kralinger, F. (2020). Does cement augmentation of the screws in angular stable plating for proximal humerus fractures influence the radiological outcome: A retrospective assessment. Archives of Orthopaedic and Trauma Surgery, 140, 1413–1421.
Acknowledgements
We are deeply grateful to all of the research staff, and this study would not be possible without their active participation and generous assistance.
Funding
No funding resources.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Surgical procedures, data collection and analysis were performed by YW, LZ, and CL. The first draft of the manuscript was written by YW and all authors actively participated in the preparation and revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
All authors declare that they have no conflict of interest.
Ethics Approval and Consent to Participate
The medical ethical committee of the Third Affiliated Hospital of Southern Medical University granted research ethics approval (Number:2023-Lunshen-037; Date: 29.June.2023). We obtained informed consent from each patient before any testing was performed.
Consent for Publication
Not applicable.
Informed Consent
For this type of study informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, Y., Zhao, L., Liu, C. et al. Application of Intramedullary Calcar Support Plate and Lateral Locking Plate in Elderly Patients with Neer 3 and 4-Part Fractures of Proximal Humerus Through a Deltoid Splitting Approach. JOIO 58, 362–370 (2024). https://doi.org/10.1007/s43465-024-01098-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-024-01098-3