Abstract
Background
Whilst access to cannabis-based medicinal products (CBMPs) has increased globally subject to relaxation of scheduling laws globally, one of the main barriers to appropriate patient access remains a paucity of high-quality evidence surrounding their clinical effects.
Discussion
Whilst randomised controlled trials (RCTs) remain the gold-standard for clinical evaluation, there are notable barriers to their implementation. Development of CBMPs requires novel approaches of evidence collection to address these challenges. Real world evidence (RWE) presents a solution to not only both provide immediate impact on clinical care, but also inform well-conducted RCTs. RWE is defined as evidence derived from health data sourced from non-interventional studies, registries, electronic health records and insurance data. Currently it is used mostly to monitor post-approval safety requirements allowing for long-term pharmacovigilance. However, RWE has the potential to be used in conjunction or as an extension to RCTs to both broaden and streamline the process of evidence generation.
Conclusion
Novel approaches of data collection and analysis will be integral to improving clinical evidence on CBMPs. RWE can be used in conjunction or as an extension to RCTs to increase the speed of evidence generation, as well as reduce costs. Currently, there is an abundance of potential data however, whilst a number of platforms now exist to capture real world data it is important the right tools and analysis are utilised to unlock potential insights from these.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Cannabis-based medicinal products (CBMPs) are a collective term to describe a preparation or other product that contains cannabis or its derivatives for medicinal use in humans [1]. There are significant barriers to the integration of CBMPs within treatment pathways including ongoing stigma, cost, education, complex pharmacology and a paucity of evidence to inform international and national guidelines [2, 3]. Limited evidence, does, however, support the role of CBMPs in conditions such as chronic pain, neurological disorders, and psychiatric disease [4]. There is also growing evidence of side effects and how the severity and incidence of side effects may differ between patients [4]. The quality of evidence, however, is often insufficient in the opinion of insurers, regulators, and guideline bodies [5].
The National Institute for Health and Care Excellence in the UK has only recommended licensed CBMPs for a limited range of indications [6]. Changes to scheduling as recommended by the World Health Organisation, and within individual countries, recognises the potential medicinal value of cannabis and removes barriers for clinical and research use [1, 7]. However, widespread stigma, complex pharmacology, funding, and challenges in sustaining adequate supply of consistent products continue to act as barriers for clinical research.
Randomised controlled trials (RCTs) are necessary and should continue to be the standard against which medical evidence is upheld. However, they are expensive, time consuming and subject to their own limitations [8]. Whilst these are awaited, there is a requirement to generate evidence of potential benefits and harms to inform policy and clinical practice.
Barriers to Controlled Clinical Trials for Medical Cannabis
RCTs are not infallible—they are expensive and time consuming. Globally $100 billion USD is spent on biomedical research [9]. In the UK, the National Institute for Health Research (NIHR) provides £80 million GBP in funding for clinical trials [10]. Yet, their narrow scope can lack ecological validity to real-world circumstances and therefore lack generalisability in more diverse populations. There are also specific barriers to conducting RCTs using CBMPs.
Complex Pharmacology
In addition to cannabidiol (CBD) and (−)-trans-Δ9-tetrahydrocannabinol (THC) there are over 140 cannabinoids, as well as flavonoids, terpenes, and other compounds within the flower of different cannabis plants [8]. These can each potentially affect the clinical outcomes observed between CBMPs due to their individual and collective effects [11]. The concentrations of each compound are influenced by the genetics and environment each plant is grown in producing a distinct chemical profile. The result of a clinical trial for one finished pharmaceutical product, therefore, cannot be extrapolated to all CBMPs, due to their heterogeneity. However, current evidence reviews often fail to account for this [12, 13].
The route of administration further affects the pharmacokinetics of CBMPs and the associated outcome of any trial. CBMPs can be administered sublingually, trans-dermally, via inhalation, or orally [14]. This subsequently affects the distribution, biotransformation and elimination of active compounds. Heat exposure and vaporisation of dried flower or extracted oils changes the underlying phytocannabinoid composition compared to the original unprocessed dry flowers, increasing the proportion of decarboxylated cannabinoids [15, 16]. Assessment of efficacy using RCTs in isolation will therefore ultimately fail to identify the most appropriate CBMP for each clinical scenario [17].
Placebo-control
An appropriately blinded assessment against placebo or active therapy is the optimal design for RCTs. It has been difficult to identify a placebo that cannot be distinguished against an active CBMP according to absence of both vasoactive and psychoactive effects, as well as the typical aroma associated with cannabis [15]. This presents a challenge to adequate blinding.
Cost
Production methods and import costs mean that CBMPs are typically expensive, adding further to high research costs [18]. Research has therefore focused on compounds under patent as opposed to generic CBMPs where research outcomes fail to provide a similar return on investment for licensed producers and pharmaceutical companies. Historically, clinical trials on CBMPs were funded privately, which may be associated with potential reporting biases [19].
RCTs are possible with CBMPs; however, the above issues present legitimate challenges. In many chronic diseases there is a need for novel therapeutics and CBMPs are therefore being utilised based on best available evidence. Due to the challenges in developing CBMPs through a traditional drug development pipeline, the exploration of its utility should not be limited to traditional methods. It is important that we capture a suite of real-world evidence (RWE) to inform prescribing guidelines, regulations, and clinical trials. By leaning on RWE there is an opportunity to improve the quality and design of RCTs and clinical evidence in general, via a top-down approach [20].
Real World Evidence
RWE is defined as evidence derived from health data sourced from non-interventional studies, registries, electronic health records and insurance data as opposed to the highly controlled setting of RCTs [21]. There is an abundance of this unstructured data, however, the necessary frameworks and governance are needed for the application of this data [22]. It is currently used extensively to monitor post-approval pharmacovigilence [23]. There is clear evidence of benefit in using population-based data to detect safety events associated with specific medications to implement restrictions to reduce harm [21].
Consistent use of RWE to aid regulatory decision making is yet to be normalised, but the promise is apparent [21]. Recently, regulator-supported initiatives have highlighted the desire to incorporate RWE into licensing and guidelines, developing a framework which can incorporate its insights into decisions regarding safety and effectiveness [21, 22]. It is important that studies standardise their methodology according to those set out by regulatory authorities to ensure research has the greatest impact [21, 22]. Moreover, they should seek to directly address questions set out by governing bodies as areas where there is insufficient research [24].
Types of Real-World Evidence for Medical Cannabis
NHS England and NHS improvement published a review on the barriers to accessing CBMPs in the UK [3]. Their recommendations included the need for the collection of structured data, and the development of methods to further support the generation of new evidence, for patients who cannot enrol onto relevant RCTs.
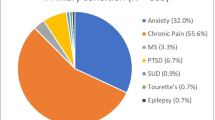
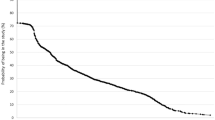
RWE is already being incorporated into the scientific literature on cannabis (Table 1). Early examples utilised state-level records to examine the effects of cannabis laws on opioid misuse. Subsequently there have been examples of online and self-administered survey tools analysing national outcomes. More recently there has been a focus on collecting evidence from clinical registries and databases with evidence generated from patient-reported outcome measures and long-term pharmacovigilance.
Comparison of Real-World Evidence and Controlled Clinical Trials
Between these study designs it is important to be aware of potential divergence in reported outcomes. RWE has broader inclusion criteria, accounting for factors like non-standard dosing, and is not limited by scope of disease, thereby improving ecological validity [25]. However, some studies have concluded there is little difference between results obtained via RCTs and observational studies [26]. RWE typically has longer patient follow-up and may consequently capture rare but important adverse effects that are not detected within RCTs. Pharmacovigilance is therefore widely accepted as one of the most important roles of RWE.
RWE can bring further clarity on questions that remain unanswered in RCTs. A recent study utilised anonymised surveys of patients with fibromyalgia who consumed cannabis flower [27]. In addition to reporting positive outcomes on depression and pain the study also reported negative aspects of cannabis consumption, for example driving under the influence (72% of patients) [27]. These are findings which are unlikely to be reported by patients in controlled clinical trials for fear of repercussions, or strict inclusion criteria. It can also be useful in collecting data in rare conditions whereby recruitment to RCTs can be limited by the need for defined trial sites.
RWE can improve the efficiency of clinical trials by generating hypotheses, refining eligibility criteria, and exploring drug development tools. Registries can be used to form an infrastructure to conduct a clinical trial, lowering costs whilst maintaining high evidence quality [28]. In supplemented single arm trials the controls are derived from RWE-data sets, providing the opportunity for patient centric study designs. RCTs can also be augmented with real-world data to increase the size of the control group to increase the power of the study. These study designs are particularly useful for rare diseases where participant recruitment is challenging [29].
Limitations of Real-World Evidence
RWE, however, does have limits to its utility. There is variation in the quality and provenance of the data stored in electronic medical records [5]. Furthermore, insurance records typically use coding specific for reimbursement purposes and may not provide all clinically relevant information. RWE can require complex statistical expertise to deduce valid conclusions.
Another limitation is the lack of randomisation, controlled variables and internal validity. This can make it more difficult to derive causative mechanisms behind clinical outcomes. However, this is also one of the strengths of these studies, allowing for generalisability to true clinical practice [22]. Treatment assignment based on the physician as opposed to randomisation, creates selection bias and more specifically stigma biases. RCTs, therefore, are still necessary to establish a strong causal relationship between medication and outcomes [30].
Conclusion
CBMPs are a complex range of pharmaceuticals which pose challenges to traditional pathways of drug development and translation. Development of CBMPs requires novel approaches of evidence collection to address these challenges. RWE can be used in conjunction or as an extension to RCTs to both broaden and streamline the process of evidence generation. Currently, there is an abundance of potential data, however, it is important the right tools and analysis are utilised to unlock potential insights from these.
Availability of Data and Materials
Not Applicable.
Abbreviations
- CBD:
-
Cannabidiol
- CBMPS:
-
Cannabis-based medicinal products
- FDA:
-
Food and Drug Administration
- NHS:
-
National Health Service
- NIHR:
-
National Institute for Health Research
- RCTs:
-
Randomised Controlled Trials
- RWE:
-
Real world evidence
- SATs:
-
Supplemented single arm trials
- THC (−):
-
Trans-Δ9-tetrahydrocannabinol
References
Case P. The NICE guideline on medicinal Cannabis: keeping Pandora’s box shut tight? Med Law Rev. 2020;28(2):401–11.
Alexander SPH. Barriers to the wider adoption of medicinal Cannabis. Br J Pain. 2020;14(2):122–32. https://doi.org/10.1177/2049463720922884.
Barriers to accessing cannabis-based products for medicinal use on NHS prescription Findings and Recommendations; 8 August 2019.
Allan GM, Finley CR, Ton J, Perry D, Ramji J, Crawford K, Lindblad AJ, Korownyk C, Kolber MR. Systematic review of systematic reviews for medical cannabinoids: pain, nausea and vomiting, spasticity, and harms. Can Fam Phys. 2018;64(2):e78-94.
Camm AJ, Fox KAA. Strengths and weaknesses of ‘real-world’ studies involving non-vitamin K antagonist oral anticoagulants. Open Heart. 2018;5(1):e000788. https://doi.org/10.1136/openhrt-2018-000788.
Chang-Douglass S, Mulvihill C, Pilling S. Cannabis-based medicinal products: summary of NICE guidance. BMJ. 2020;21:369.
Pahuja E, Santosh KT, Harshitha N, et al. Diploma in primary care psychiatry: do primary care doctors need training in cannabis use disorder module? J Fam Med Prim Care. 2021;10(3):1086.
McPartland J, Russo E. Cannabis and cannabis extracts: greater than the sum of their parts? J Cannabis Ther. 2001;1:103–32. https://doi.org/10.1300/J175v01n03_08.
Chalmers I, Glasziou P. Avoidable waste in the production and reporting of research evidence. The Lancet. 2009;374(9683):86–9.
The Misuse of Drugs (Amendments) (Cannabis and Licence Fees) (England, Wales and Scotland) Regulations 2018. Queen’s Printer of Acts of Parliament.
Lee T. Cannabis Metabolomics: Comparison of Cannabis Products and Effect of Vaporization. 2019. https://doi.org/10.20381/ruor-23949.
Whiting PF, Wolff RF, Deshpande S, et al. Cannabinoids for medical use: a systematic review and meta-analysis. JAMA. 2015;313(24):2456–73.
Aviram J, Samuelly-Leichtag G. Efficacy of Cannabis-based medicines for pain management: a systematic review and meta-analysis of randomized controlled trials. Pain Physician. 2017;20(6):E755–96.
MacCallum CA, Russo EB. Practical considerations in medical Cannabis administration and dosing. Eur J Intern Med. 2018;1(49):12–9.
Pauli CS, Conroy M, vanden Heuvel BD, et al. Cannabidiol Drugs Clinical Trial Outcomes and adverse effects. Front Pharmacol. 2020;11:63. https://doi.org/10.3389/fphar.2020.00063.
Andre CM, Hausman J-F, Guerriero G. Cannabis sativa: the plant of the thousand and one molecules. Front Plant Sci. 2016;7:19. https://doi.org/10.3389/fpls.2016.00019.
GMP Question and Answers. 2015. [Online] World Health Organisation. https://www.who.int/medicines/areas/quality_safety/quality_assurance/gmp/en/#:~:text=Good%20manufacturing%20practice%20(GMP)%20is,through%20testing%20the%20final%20product. Accessed 10 Aug 2020.
Kilmer B, Burgdorf J. 6. Insights about cannabis production and distribution costs in the EU. Further insights into aspects of the EU illicit drugs market. 2013:33.
Dreyer NA, Hall M, Christian JB. Modernizing regulatory evidence with trials and real-world studies. Ther Innov Regul Sci. 2020. https://doi.org/10.1007/s43441-020-00131-5.
Real world evidence. FORUM Programme. The Academy of Medical Sciences and the Association of the British Pharmaceutical Industry. 2016. https://www.england.nhs.uk/publication/barriers-to-accessing-cannabis-based-products-for-medicinal-use-on-nhs-prescription/.
Baumfeld Andre E, Reynolds R, Caubel P, et al. Trial designs using real-world data: the changing landscape of the regulatory approval process. Pharmacoepidemiol Drug Saf. 2019. https://doi.org/10.1002/pds.4932.
Framework for FDA’s Real-World Evidence Program. 2018. www.fda.gov.
Ehrenstein V, Hernandez RK, Ulrichsen SP, et al. Rosiglitazone use and post-discontinuation glycaemic control in two European countries, 2000–2010. BMJ Open. 2013;3(9):e003424. https://doi.org/10.1136/bmjopen-2013-003424.
England NH. Barriers to accessing cannabis-based products for medicinal use on NHS prescription. August 2019.
Jeynes-Ellis A. Guidance Demonstrating Value with Real World Data: A Practical Guide. 2011. https://www.abpi.org.uk/media/1591/2011-06-13-abpi-guidance-demonstrating-value-with-real-world-data.pdf.
Anglemyer A, Horvath HT, Bero L. Healthcare outcomes assessed with observational study designs compared with those assessed in randomized trials. Cochrane Database Syst Rev. 2014. https://doi.org/10.1002/14651858.MR000034.pub2.
Habib G, Avisar I. The consumption of Cannabis by fibromyalgia patients in Israel. Pain Res Treat. 2018;2018:1–5.
Mikita JS, Mitchel J, Gatto NM, et al. Determining the suitability of registries for embedding clinical trials in the United States: a project of the clinical trials transformation initiative. Ther Innov Regul Sci. 2020. https://doi.org/10.1007/s43441-020-00185-5.
Gray CM, Grimson F, Layton D, et al. A framework for methodological choice and evidence assessment for studies using external comparators from real-world data. Drug Safety. Adis. 2020;43(7):623–33. https://doi.org/10.1007/s40264-020-00944-1.
Kim H-S, Kim JH. Proceed with caution when using real world data and real world evidence. J Korean Med Sci. 2019;34(4):e28–e28. https://doi.org/10.3346/jkms.2019.34.e28.
Ware M, Adams H, Guy G. The medicinal use of cannabis in the UK: results of a nationwide survey. Int J Clin Pract. 2004;59(3):291–5.
Sexton M, Cuttler C, Finnell J, et al. A cross-sectional survey of medical Cannabis users: patterns of use and perceived efficacy. Cannabis Cannabinoid Res. 2016;1(1):131–8.
Lucas P, Walsh Z. Medical cannabis access, use, and substitution for prescription opioids and other substances: a survey of authorized medical cannabis patients. Int J Drug Policy. 2017;42:30–5.
Lintzeris N, Mills L, Suraev A, et al. Medical cannabis use in the Australian community following introduction of legal access: the 2018–2019 Online Cross-Sectional Cannabis as Medicine Survey (CAMS-18). Harm Reduct J. 2020;17:1–2.
Bachhuber M, Saloner B, Cunningham C, et al. Medical Cannabis laws and opioid analgesic overdose mortality in the United States, 1999–2010. JAMA Intern Med. 2014;174(10):1668.
Piper B, Desrosiers C, Fisher H, et al. A new tool to tackle the opioid epidemic: description, utility, and results from the Maine diversion alert program. Pharmacother: J Hum Pharmacol Drug Therapy. 2017;37(7):791–8.
Vigil J, Stith S, Adams I, et al. Associations between medical cannabis and prescription opioid use in chronic pain patients: a preliminary cohort study. PLoS ONE. 2017;12(11):e0187795.
Bonn-Miller M, Boden M, Bucossi M, et al. Self-reported cannabis use characteristics, patterns and helpfulness among medical cannabis users. Am J Drug Alcohol Abuse. 2013;40(1):23–30.
Gulbransen G, Xu W, Arroll B. Cannabidiol prescription in clinical practice: an audit on the first 400 patients in New Zealand. BJGP Open. 2020;4(1):bjgpopen20X101010.
Rapin L, Gamaoun R, El Hage C, et al. Cannabidiol use and effectiveness: real-world evidence from a Canadian medical cannabis clinic. J Cannabis Res. 2021;3(1):1–10.
Ueberall M, Essner U, Mueller-Schwefe G. Effectiveness and tolerability of THC:CBD oromucosal spray as add-on measure in patients with severe chronic pain: analysis of 12-week open-label real-world data provided by the German Pain e-Registry. J Pain Res. 2019;12:1577–604.
Mahabir V, Merchant J, Smith C, et al. Medical cannabis use in the United States: a retrospective database study. J Cannabis Res. 2020;2(1):1–13.
World First: Launch of Quebec Registry for Users of Medical Cannabis. 2015. https://registrecannabisquebec.com/en. Accessed 10 Aug 2020.
Avicanna Announces Participation in a Medical Cannabis Real-World Evidence (MC-RWE) Clinical Study Led by the University Health Network in Partnership with Medical Cannabis by ShoppersTM Inc. using its Rho PhytoTM Advanced Medical Cannabis Formulary of Products - Avicanna | A Leader in Biopharmaceutical Advancements in Cannabis. https://www.avicanna.com/avicanna-announces-participation-in-a-medical-cannabis-real-world-evidence-mc-rwe-clinical-study-led-by-the-university-health-network-in-partnership-with-medical-cannabis-by-shoppers-inc-u/. Accessed 3 Oct 2020.
Medical Cannabis Put to Test in First Ever Real-World Evidence Clinical Trial Led by UHN. https://medicalxpress.com/news/2020-07-medical-cannabis-real-world-evidence-clinical.html. Accessed 3 Oct 2020.
MC-RWE Study Protocol Title: Real-World Evidence in Patient-Reported Outcomes for Medical Cannabis: A Prospective Observational study. https://clinicaltrials.gov/ct2/show/NCT04526093.
UK Medical Cannabis Registry. [Online] Sapphire Medical Clinics. https://www.ukmedicalcannabisregistry.com/. Accessed 10 Aug 2020.
Erridge S, Salazar O, Kawka M, et al. An initial analysis of the UK Medical Cannabis Registry: Outcomes analysis of first 129 patients. Neuropsychopharmacology Reports. 2021.
Project Twenty21. https://drugscience.org.uk/project-twenty21/.
Project Twenty21 - drugscience.org.uk. https://drugscience.org.uk/project-twenty21/?gclid=CjwKCAjwh7H7BRBBEiwAPXjadsqEtPkvN38hujNnOiaqtJcGVD8uoUE7UTZjNaF9UipdheIoaH6LAxoCTVAQAvD_BwE. Accessed 1 Oct 2020.
Emerald Clinics. https://www.emeraldclinics.com.au/. Accessed 1 Oct 2020.
Emerald Clinics: Co-creating Evidence with Medical Cannabis Patients. https://www.healtheuropa.eu/emerald-clinics-co-creating-evidence-with-medical-cannabis-patients/98569/. Accessed 1 Oct 2020.
Emyria Capitalises on Cann Group Collaboration to Progress EMD-003 CBD Medicine for Mental Health [Internet]. Proactiveinvestors UK. 2021. https://www.proactiveinvestors.com.au/companies/news/952675/emyria-capitalises-on-cann-group-collaboration-to-progress-emd-003-cbd-medicine-for-mental-health-952675.html. Accessed 5 July 2021.
Medical Cannabis - Minnesota Department of Health [Internet]. Health.state.mn.us. 2021. https://www.health.state.mn.us/people/cannabis/. Accessed 5 July 2021.
BfArM - Homepage - Cannabis [Internet]. Bfarm.de. 2021. https://www.bfarm.de/SharedDocs/Glossareintraege/DE/C/Cannabis.html. Accessed 5 July 2021.
Inc. S. CB2 Insights Launches Industry’s First Medical Cannabis Insights Dashboard for All Medical Cannabis Stakeholders [Internet]. GlobeNewswire News Room. 2021. https://www.globenewswire.com/news-release/2020/03/30/2008219/0/en/CB2-Insights-Launches-Industry-s-First-Medical-Cannabis-Insights-Dashboard-for-All-Medical-Cannabis-Stakeholders.html. Accessed 5 July 2021.
Federspiel G. The Danish Medicinal Cannabis Pilot Programme [Internet]. Gorrissen Federspiel. 2021. https://gorrissenfederspiel.com/en/knowledge/news/the-danish-medicinal-cannabis-pilot-programme. Accessed 5 July 2021.
Freeman T, Morgan C, Hindocha C. Strengthening the evidence for medicinal cannabis and cannabinoids. BMJ. 2019. https://doi.org/10.1136/bmj.l5871.
France Takes Further Steps Regarding Medical Cannabis - ECA Academy [Internet]. Gmp-compliance.org. 2021. https://www.gmp-compliance.org/gmp-news/france-takes-further-steps-regarding-medical-cannabis. Accessed 5 July 2021.
Medical Cannabis Access Programme [Internet]. Hpra.ie. 2021. http://www.hpra.ie/homepage/controlled-substances/controlled-substances/medical-cannabis-access-programme. Accessed 5 July 2021.
Acknowledgements
Not Applicable.
Funding
Not Applicable.
Author information
Authors and Affiliations
Contributions
RB and SE prepared the manuscript. OS, NM, DC, BP, MS read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interest
SE: Sapphire Medical Clinics. DC: Medical Lead Centre for Medicinal Cannabis. BP: Chief Scientific Officer at Emmac Life Sciences. MHS: Sapphire Medical Clinics Managing Director and Research lead at Emmac Life Sciences.
Ethical Approval
Not Applicable.
Consent for Publication
Not Applicable.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Banerjee, R., Erridge, S., Salazar, O. et al. Real World Evidence in Medical Cannabis Research. Ther Innov Regul Sci 56, 8–14 (2022). https://doi.org/10.1007/s43441-021-00346-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43441-021-00346-0