Abstract
Purpose
Early onset scoliosis (EOS) patient diversity makes outcome prediction challenging. Machine learning offers an innovative approach to analyze patient data and predict results, including LOS in pediatric spinal deformity surgery.
Methods
Children under 10 with EOS were chosen from the American College of Surgeon’s NSQIP database. Extended LOS, defined as over 5 days, was predicted using feature selection and machine learning in Python. The best model, determined by the area under the curve (AUC), was optimized and used to create a risk calculator for prolonged LOS.
Results
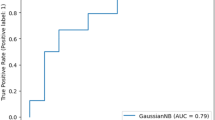
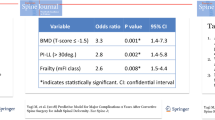
The study included 1587 patients, mostly young (average age: 6.94 ± 2.58 years), with 33.1% experiencing prolonged LOS (n = 526). Most patients were female (59.2%, n = 940), with an average BMI of 17.0 ± 8.7. Factors influencing LOS were operative time, age, BMI, ASA class, levels operated on, etiology, nutritional support, pulmonary and neurologic comorbidities. The gradient boosting model performed best with a test accuracy of 0.723, AUC of 0.630, and a Brier score of 0.189, leading to a patient-specific risk calculator for prolonged LOS.
Conclusions
Machine learning algorithms accurately predict extended LOS across a national patient cohort and characterize key preoperative drivers of increased LOS after PSIF in pediatric patients with EOS.



Similar content being viewed by others
References
AlNouri M, Wada K, Kumagai G et al (2023) Diseases and comorbidities associated with early-onset scoliosis: a retrospective multicenter analysis. Spine Deform 11(2):481–486. https://doi.org/10.1007/s43390-022-00613-6
Whitcomb WF, Lagu T, Krushell RJ et al (2015) Experience with designing and implementing a bundled payment program for total hip replacement. Jt Comm J Qual Patient Saf 41(9):406–413. https://doi.org/10.1016/s1553-7250(15)41052-9
Gulotta LV, Padgett DE, Sculco TP, Urban M, Lyman S, Nestor BJ (2011) Fast track THR: one hospital’s experience with a 2-day length of stay protocol for total hip replacement. HSS J 7(3):223–228. https://doi.org/10.1007/s11420-011-9207-2
Somani S, Di CJ, Kim JS et al (2017) ASA classification as a risk stratification tool in adult spinal deformity surgery: a study of 5805 patients. Glob Spine J 7(8):719–726. https://doi.org/10.1177/2192568217700106
Matsumoto H, Larson EL, Warren SI et al (2022) A clinical risk model for surgical site infection following pediatric spine deformity surgery. J Bone Jt Surg Am 104(4):364–375. https://doi.org/10.2106/JBJS.21.00751
Xue QL (2011) The frailty syndrome: definition and natural history. Clin Geriatr Med 27(1):1–15. https://doi.org/10.1016/j.cger.2010.08.009
Buta BJ, Walston JD, Godino JG et al (2016) Frailty assessment instruments: systematic characterization of the uses and contexts of highly-cited instruments. Ageing Res Rev 26:53–61. https://doi.org/10.1016/j.arr.2015.12.003
Fried LP, Tangen CM, Walston J et al (2001) Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56(3):M146–M156. https://doi.org/10.1093/gerona/56.3.m146
Searle SD, Mitnitski A, Gahbauer EA, Gill TM, Rockwood K (2008) A standard procedure for creating a frailty index. BMC Geriatr 8:24. https://doi.org/10.1186/1471-2318-8-24
Schuijt HJ, Morin ML, Allen E, Weaver MJ (2021) Does the frailty index predict discharge disposition and length of stay at the hospital and rehabilitation facilities? Injury 52(6):1384–1389. https://doi.org/10.1016/j.injury.2021.01.004
Cheung A, Haas B, Ringer TJ, McFarlan A, Wong CL (2017) Canadian study of health and aging clinical frailty scale: does it predict adverse outcomes among geriatric trauma patients? J Am Coll Surg 225(5):658−665e3. https://doi.org/10.1016/j.jamcollsurg.2017.08.008
Miller EK, Neuman BJ, Jain A et al (2017) An assessment of frailty as a tool for risk stratification in adult spinal deformity surgery. Neurosurg Focus 43(6):E3. https://doi.org/10.3171/2017.10.FOCUS17472
Yagi M, Michikawa T, Hosogane N et al (2019) The 5-item modified frailty index is predictive of severe adverse events in patients undergoing surgery for adult spinal deformity. Spine (Phila Pa 1976) 44(18):E1083–E1091. https://doi.org/10.1097/BRS.0000000000003063
Cloyd C, Moffett BS, Bernhardt MB, Monico EM, Patel N, Hanson D (2018) Efficacy of liposomal bupivacaine in pediatric patients undergoing spine surgery. Paediatr Anaesth 28(11):982–986. https://doi.org/10.1111/pan.13482
Fletcher ND, Andras LM, Lazarus DE et al (2017) Use of a novel pathway for early discharge was associated with a 48% shorter length of stay after posterior spinal fusion for adolescent idiopathic scoliosis. J Pediatr Orthop 37(2):92–97. https://doi.org/10.1097/BPO.0000000000000601
Laverdière C, Georgiopoulos M, Ames CP et al (2022) Adult spinal deformity surgery and frailty: a systematic review. Glob Spine J 12(4):689–699. https://doi.org/10.1177/21925682211004250
Leven DM, Lee NJ, Kothari P et al (2016) Frailty index is a significant predictor of complications and mortality after surgery for adult spinal deformity. Spine (Phila Pa 1976) 41(23):E1394–E1401. https://doi.org/10.1097/BRS.0000000000001886
Stone K, Zwiggelaar R, Jones P, Mac PN (2022) A systematic review of the prediction of hospital length of stay: towards a unified framework. PLOS Digit Heal 1(4):e0000017. https://doi.org/10.1371/journal.pdig.0000017
Krell RW, Girotti ME, Dimick JB (2014) Extended length of stay after surgery: complications, inefficient practice, or sick patients? JAMA Surg 149(8):815–820. https://doi.org/10.1001/jamasurg.2014.629
Hornung AL, Hornung CM, Mallow GM et al (2022) Artificial intelligence in spine care: current applications and future utility. Eur Spine J 31(8):2057–2081. https://doi.org/10.1007/s00586-022-07176-0
Ames CP, Smith JS, Pellisé F et al (2019) Artificial intelligence based hierarchical clustering of patient types and intervention categories in adult spinal deformity surgery: towards a new classification scheme that predicts quality and value. Spine (Phila Pa 1976) 44(13):915–926. https://doi.org/10.1097/BRS.0000000000002974
Joshi RS, Haddad AF, Lau D, Ames CP (2019) Artificial intelligence for adult spinal deformity. Neurospine 16(4):686–694. https://doi.org/10.14245/ns.1938414.207
Huber FA, Stutz S, Vittoria de Martini I et al (2019) Qualitative versus quantitative lumbar spinal stenosis grading by machine learning supported texture analysis-experience from the LSOS study cohort. Eur J Radiol 114:45–50. https://doi.org/10.1016/j.ejrad.2019.02.023
Meyer A, Zverinski D, Pfahringer B et al (2018) Machine learning for real-time prediction of complications in critical care: a retrospective study. Lancet Respir Med 6(12):905–914. https://doi.org/10.1016/S2213-2600(18)30300-X
Gowd AK, Agarwalla A, Amin NH et al (2019) Construct validation of machine learning in the prediction of short-term postoperative complications following total shoulder arthroplasty. J Shoulder Elb Surg 28(12):e410–e421. https://doi.org/10.1016/j.jse.2019.05.017
Awan SE, Bennamoun M, Sohel F, Sanfilippo FM, Dwivedi G (2019) Machine learning-based prediction of heart failure readmission or death: implications of choosing the right model and the right metrics. ESC Hear Fail 6(2):428–435. https://doi.org/10.1002/ehf2.12419
McGirt MJ, Sivaganesan A, Asher AL, Devin CJ (2015) Prediction model for outcome after low-back surgery: individualized likelihood of complication, hospital readmission, return to work, and 12-month improvement in functional disability. Neurosurg Focus 39(6):E13. https://doi.org/10.3171/2015.8.FOCUS15338
FACS org (2023) Hospital and facilities. https://www.facs.org/hospital-and-facilities/?searchTerm=&institution=NsqipHospital&page=1. Accessed 18 Apr 2024
Kattan MW, Gerds TA (2018) The index of prediction accuracy: an intuitive measure useful for evaluating risk prediction models. Diagn Progn Res 2:7. https://doi.org/10.1186/s41512-018-0029-2
Gerds TA, Cai T, Schumacher M (2008) The performance of risk prediction models. Biom J 50(4):457–479. https://doi.org/10.1002/bimj.200810443
Rachoin JS, Aplin KS, Gandhi S, Kupersmith E, Cerceo E (2020) Impact of length of stay on readmission in hospitalized patients. Cureus 12(9):e10669. https://doi.org/10.7759/cureus.10669
Zhang AS, Veeramani A, Quinn MS, Alsoof D, Kuris EO, Daniels AH (2021) Machine learning prediction of length of stay in adult spinal deformity patients undergoing posterior spine fusion surgery. J Clin Med. https://doi.org/10.3390/jcm10184074
Basques BA, Bohl DD, Golinvaux NS, Smith BG, Grauer JN (2015) Patient factors are associated with poor short-term outcomes after posterior fusion for adolescent idiopathic scoliosis. Clin Orthop Relat Res 473(1):286–294. https://doi.org/10.1007/s11999-014-3911-4
Elsamadicy AA, Koo AB, Kundishora AJ et al (2019) Impact of patient and hospital-level risk factors on extended length of stay following spinal fusion for adolescent idiopathic scoliosis. J Neurosurg Pediatr. https://doi.org/10.3171/2019.5.PEDS19161
Upasani VV, Caltoum C, Petcharaporn M et al (2008) Does obesity affect surgical outcomes in adolescent idiopathic scoliosis? Spine (Phila Pa 1976) 33(3):295–300. https://doi.org/10.1097/BRS.0b013e3181624573
Gruskay JA, Fu M, Bohl DD, Webb ML, Grauer JN (2015) Factors affecting length of stay after elective posterior lumbar spine surgery: a multivariate analysis. Spine J 15(6):1188–1195. https://doi.org/10.1016/j.spinee.2013.10.022
Kobayashi K, Ando K, Kato F et al (2019) Predictors of prolonged length of stay after lumbar interbody fusion: a multicenter study. Glob Spine J 9(5):466–472. https://doi.org/10.1177/2192568218800054
Hajian-Tilaki K (2013) Receiver operating characteristic (ROC) curve analysis for medical diagnostic test evaluation. Casp J Intern Med 4(2):627–635
Siddique SM, Tipton K, Leas B et al (2021) Interventions to reduce hospital length of stay in high-risk populations: a systematic review. JAMA Netw Open 4(9):e2125846. https://doi.org/10.1001/jamanetworkopen.2021.25846
Funding
No extra funding for this project.
Author information
Authors and Affiliations
Contributions
Michael W. Fields: made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data, or the creation of new software used in the work, drafted the work or revised it critically for important intellectual content, approved of the version to be published, agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Jay Zaifman: made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data, or the creation of new software used in the work, drafted the work or revised it critically for important intellectual content, approved of the version to be published, agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Matan S. Malka: made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data, or the creation of new software used in the work, drafted the work or revised it critically for important intellectual content, approved of the version to be published, agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Nathan J. Lee: made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data, or the creation of new software used in the work, drafted the work or revised it critically for important intellectual content, approved of the version to be published, agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Christina C. Rymond: made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data, or the creation of new software used in the work, drafted the work or revised it critically for important intellectual content, approved of the version to be published, agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Matthew E. Simhon: made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data, or the creation of new software used in the work, drafted the work or revised it critically for important intellectual content, approved of the version to be published, agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Theodore Quan: made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data, or the creation of new software used in the work, drafted the work or revised it critically for important intellectual content, approved of the version to be published, agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Benjamin D. Roye: made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data, or the creation of new software used in the work, drafted the work or revised it critically for important intellectual content, approved of the version to be published, agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Michael G. Vitale: made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data, or the creation of new software used in the work, drafted the work or revised it critically for important intellectual content, approved of the version to be published, agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
MWF has no conflicts of interest to disclose. JZ has no conflicts of interest to disclose. NJL has no conflicts of interest to disclose. CCR has no conflicts of interest to disclose. MSM has no conflicts of interest to disclose. MES has no conflicts of interest to disclose. TQ has no conflicts of interest to disclose. BDR has received grants from the Pediatric Orthopaedic Society of North America and the Orthopedic Science Research Foundation. MGV has received grants from the Pediatric Orthopaedic Society of North America, Orthopedic Science Research Foundation, Pediatric Spine Foundation, and Setting Scoliosis Straight Foundation and royalties from Biomet. He is a paid consultant for Stryker, Biomet, and NuVasive. MGV is on the Board of Directors of the Pediatric Spine Foundation, Pediatric Spine Study Group, and C4K. He is a former president of the Pediatric Orthopaedic Society of North America and is a Board Member, and Chair Emeritus of the International Pediatric Orthopaedic Symposium.
Ethical approval
This study did not require Columbia University Institutional Review Board review since our study used a public database. The database was created in accordance with the ethical standards of the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
This study qualifies for a waiver of consent because it is a database study. It does not require patient participation, as all data has already been collected during routine clinical care. There is no potential to adversely affect the rights or welfare of subjects since this is a database study.
Permission to reproduce copyrighted materials
No copyrighted materials or patient information is included in this manuscript submission.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fields, M.W., Zaifman, J., Malka, M.S. et al. Utilizing a comprehensive machine learning approach to identify patients at high risk for extended length of stay following spinal deformity surgery in pediatric patients with early onset scoliosis. Spine Deform (2024). https://doi.org/10.1007/s43390-024-00889-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s43390-024-00889-w