Abstract
Purpose
To determine the frequencies of various diseases associated with all types of early-onset scoliosis, both idiopathic and nonidiopathic.
Methods
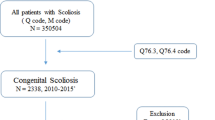
Retrospective collection of patients within a 21-year interval. Children under 10 years old presenting with scoliosis were included. Medical records were used to collect: identifier, date of birth, sex, diagnosis, follow-up, curve pattern, comorbidities, initial and final cobb angle. Different patient variables were tabulated with associated comorbidities for comparison.
Results
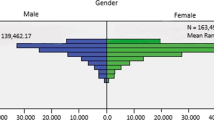
The cohort contained 469 patients, with 227(48.4%) males and 242(51.6%) females. Total comorbidities equaled 1051, where 190 were unique. Only 124(26.4%) patients had an isolated diagnosis of early-onset scoliosis, 79(16.8%) had a single comorbidity, and 266(56.7%) had multiple comorbidities. “Global developmental delay” was most commonly observed, 198(42.2%) times. The central nervous system was involved more often than other organ systems, seen in 394(54.4%) instances. Males had more comorbidities than females. Idiopathic patients had the least number of comorbidities, while neuromuscular patients had the most. Idiopathic types had more musculoskeletal conditions, while congenital types had more cardiovascular diseases. Curve sides did not affect distributions. Cases which progressed had more comorbidities, especially in the respiratory, digestive, and cardiovascular systems. Diseases that could affect either extremity or side, were more likely to be bilateral.
Conclusions
Early-onset scoliosis patients may present with complex comorbidities in multiple organ systems. The most commonly observed disease entities were: global developmental delay, developmental dysplasia of the hip, and epilepsy. Clinicians should be aware of the common associations, in order to screen for and begin appropriate investigations, referrals, and treatments in affected cases.
Level of evidence
Level III.
Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are not publicly available due to strict data privacy laws, but are available from the corresponding author on reasonable request.
References
Skaggs DL, Guillaume T, El-Hawary R et al (2015) Early onset scoliosis consensus statement, SRS Growing Spine Committee, 2015. Spine Deformity 3:107. https://doi.org/10.1016/j.jspd.2015.01.002
El-Hawary R, Akbarnia BA (2015) Early onset scoliosis—time for consensus. Spine Deformity 3:105–106. https://doi.org/10.1016/j.jspd.2015.01.003
Yang S, Andras LM, Redding GJ, Skaggs DL (2016) Early-onset scoliosis: a review of history, current treatment, and future directions. Pediatrics 137:e20150709. https://doi.org/10.1542/peds.2015-0709
Alkhalife YI, Padhye KP, El-Hawary R (2019) New technologies in pediatric spine surgery. Orthop Clin N Am 50:57–76. https://doi.org/10.1016/j.ocl.2018.08.014
Hughes MS, Swarup I, Makarewich CA et al (2020) Expert consensus for early onset scoliosis surgery. J Pediatr Orthop 40:e621–e628. https://doi.org/10.1097/BPO.0000000000001473
AlNouri M, Wada K, Kumagai G, et al (2022) The incidence and prevalence of early-onset scoliosis: a regional multicenter epidemiological study. Spine J 22(9):1540–1550. https://doi.org/10.1016/j.spinee.2022.03.016
Fernandes P, Weinstein SL (2007) Natural history of early onset scoliosis. J Bone Jt Surg Am 89(Suppl 1):21–33. https://doi.org/10.2106/JBJS.F.00754
McMaster MJ (1983) Infantile idiopathic scoliosis: can it be prevented? J Bone Jt Surg Br 65:612–617. https://doi.org/10.1302/0301-620X.65B5.6643567
Hooper G (1980) Congenital dislocation of the hip in infantile idiopathic scoliosis. J Bone Jt Surg Br Vol 62-B:447–449. https://doi.org/10.1302/0301-620X.62B4.7430221
Wynne-Davies R (1975) Infantile idiopathic scoliosis. Causative factors, particularly in the first six months of life. J Bone Jt Surg Br 57:138–141
Talmage MS, Nielson AN, Heflin JA et al (2020) Prevalence of hip dysplasia and associated conditions in children treated for idiopathic early-onset scoliosis-don’t just look at the spine. J Pediatr Orthop 40:e49–e52. https://doi.org/10.1097/BPO.0000000000001390
Lenke LG, Edwards CC, Bridwell KH (2003) The Lenke classification of adolescent idiopathic scoliosis: how it organizes curve patterns as a template to perform selective fusions of the spine. Spine (Phila Pa 1976) 28:S199–207. https://doi.org/10.1097/01.BRS.0000092216.16155.33
Isojima T, Kato N, Ito Y, et al (2016) Growth standard charts for Japanese children with mean and standard deviation (SD) values based on the year 2000 national survey. Clin Pediatr Endocrinol 25:71–76. https://doi.org/10.1297/cpe.25.71
Karol LA (2019) The natural history of early-onset scoliosis. J Pediatr Orthop 39:S38–S43. https://doi.org/10.1097/BPO.0000000000001351
Oestreich AE, Young LW, Young Poussaint T (1998) Scoliosis circa 2000: radiologic imaging perspective. I. Diagnosis and pretreatment evaluation. Skelet Radiol 27:591–605. https://doi.org/10.1007/s002560050445
Campbell RM, Smith MD, Mayes TC et al (2003) The characteristics of thoracic insufficiency syndrome associated with fused ribs and congenital scoliosis. J Bone Jt Surg Am 85:399–408. https://doi.org/10.2106/00004623-200303000-00001
Acknowledgements
The study would not have been possible without the help of Ms. Ami AlNouri Nishimori, who translated patient medical records from Japanese to English.
Funding
This study received funding from the Department of Orthopaedic Surgery and the Spine Group at Hirosaki University Graduate School of Medicine.
Author information
Authors and Affiliations
Contributions
MA: conception and design, acquisition and data, Analysis and interpretation of data, drafting of the manuscript, critical revision. KW: acquisition and data, critical revision, obtaining funding, administrative and technical support, supervision. GK: critical revision, obtaining funding, administrative and technical support, supervision. TA: critical revision, obtaining funding, administrative and technical support. YN: critical revision, administrative and technical support. TM: acquisition and data, administrative and technical support, supervision. RU: acquisition and data, administrative and technical support, supervision. MA: acquisition and data, administrative and technical support. YI: critical revision, obtaining funding, administrative and technical support, supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
Ethical approval (#2021211) was granted by the local ethics committee at Hirosaki University.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
AlNouri, M., Wada, K., Kumagai, G. et al. Diseases and comorbidities associated with early-onset scoliosis: a retrospective multicenter analysis. Spine Deform 11, 481–486 (2023). https://doi.org/10.1007/s43390-022-00613-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-022-00613-6