Abstract
Purpose
This study aims to evaluate the cost-utility of intraoperative tranexamic acid (TXA) in adult spinal deformity (ASD) patients undergoing long posterior (≥ 5 vertebral levels) spinal fusion.
Methods
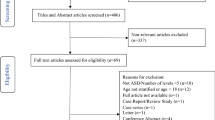
A decision-analysis model was built for a hypothetical 60-year-old adult patient with spinal deformity undergoing long posterior spinal fusion. A comprehensive review of the literature was performed to obtain event probabilities, costs and health utilities at each node. Health utilities were utilized to calculate Quality-Adjusted Life Years (QALYs). A base-case analysis was carried out to obtain the incremental cost and effectiveness of intraoperative TXA. Probabilistic sensitivity analysis was performed to evaluate uncertainty in our model and obtain mean incremental costs, effectiveness, and net monetary benefits. One-way sensitivity analyses were also performed to identify the variables with the most impact on our model.
Results
Use of intraoperative TXA was the favored strategy in 88% of the iterations. The mean incremental utility ratio for using intraoperative TXA demonstrated higher benefit and lower cost while being lower than the willingness-to-pay threshold set at $50,000 per quality adjusted life years. Use of intraoperative TXA was associated with a mean incremental net monetary benefit (INMB) of $3743 (95% CI 3492–3995). One-way sensitivity analysis reported cost of blood transfusions due to post-operative anemia to be a major driver of cost–utility analysis.
Conclusion
Use of intraoperative TXAs is a cost-effective strategy to reduce overall perioperative costs related to post-operative blood transfusions. Administration of intraoperative TXA should be considered for long fusions in ASD population when not explicitly contra-indicated due to patient factors.


Similar content being viewed by others
References
Schwab F, Dubey A, Gamez L et al (2005) Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine 30(9):1082–1085. https://doi.org/10.1097/01.brs.0000160842.43482.cd
Safaee MM, Ames CP, Smith JS (2020) Epidemiology and socioeconomic trends in adult spinal deformity care. Neurosurgery 87(1):25–32. https://doi.org/10.1093/neuros/nyz454
Smith JS, Lafage V, Shaffrey CI et al (2016) Outcomes of operative and nonoperative treatment for adult spinal deformity: a prospective, multicenter, propensity-matched cohort assessment with minimum 2-year follow-up. Neurosurgery 78(6):851–861. https://doi.org/10.1227/NEU.0000000000001116
Alvarado AM, Schatmeyer BA, Arnold PM (2021) Cost-effectiveness of adult spinal deformity surgery. Glob Spine J 11(1_suppl):73S-78S. https://doi.org/10.1177/2192568220964098
Elgafy H, Bransford RJ, McGuire RA, Dettori JR, Fischer D (2010) Blood loss in major spine surgery: are there effective measures to decrease massive hemorrhage in major spine fusion surgery? Spine 35(Supplement):S47–S56. https://doi.org/10.1097/BRS.0b013e3181d833f6
Puvanesarajah V, Rao SS, Hassanzadeh H, Kebaish KM (2018) Determinants of perioperative transfusion risk in patients with adult spinal deformity. J Neurosurg Spine 28(4):429–435. https://doi.org/10.3171/2017.10.SPINE17884
Patil CG, Santarelli J, Lad SP, Ho C, Tian W, Boakye M (2008) Inpatient complications, mortality, and discharge disposition after surgical correction of idiopathic scoliosis: a national perspective. Spine J 8(6):904–910. https://doi.org/10.1016/j.spinee.2008.02.002
Passias PG, Kummer N, Imbo B et al (2023) Improvements in outcomes and cost after adult spinal deformity corrective surgery between 2008 and 2019. Spine 48(3):189–195. https://doi.org/10.1097/BRS.0000000000004474
Raad M, Amin R, Jain A, Frank SM, Kebaish KM (2019) Multilevel arthrodesis for adult spinal deformity: when should we anticipate major blood loss? Spine Deform 7(1):141–145. https://doi.org/10.1016/j.jspd.2018.06.012
Choi HY, Hyun SJ, Kim KJ, Jahng TA, Kim HJ (2017) Effectiveness and safety of tranexamic acid in spinal deformity surgery. J Korean Neurosurg Soc 60(1):75–81. https://doi.org/10.3340/jkns.2016.0505.004
Pong RP, Leveque JCA, Edwards A et al (2018) Effect of tranexamic acid on blood loss, d-dimer, and fibrinogen kinetics in adult spinal deformity surgery. J Bone Jt Surg 100(9):758–764. https://doi.org/10.2106/JBJS.17.00860
Hariharan D, Mammi M, Daniels K et al (2019) The safety and efficacy of tranexamic acid in adult spinal deformity surgery: a systematic review and meta-analysis. Drugs 79(15):1679–1688. https://doi.org/10.1007/s40265-019-01185-y
Lin JD, Lenke LG, Shillingford JN et al (2018) Safety of a high-dose tranexamic acid protocol in complex adult spinal deformity: analysis of 100 consecutive cases. Spine Deform 6(2):189–194. https://doi.org/10.1016/j.jspd.2017.08.007
Cheriyan T, Maier SP, Bianco K et al (2015) Efficacy of tranexamic acid on surgical bleeding in spine surgery: a meta-analysis. Spine J 15(4):752–761. https://doi.org/10.1016/j.spinee.2015.01.013
Raman T, Varlotta C, Vasquez-Montes D, Buckland AJ, Errico TJ (2019) The use of tranexamic acid in adult spinal deformity: is there an optimal dosing strategy? Spine J 19(10):1690–1697. https://doi.org/10.1016/j.spinee.2019.06.012
Raksakietisak M, Sathitkarnmanee B, Srisaen P et al (2015) Two doses of tranexamic acid reduce blood transfusion in complex spine surgery: a prospective randomized study. Spine 40(24):E1257–E1263. https://doi.org/10.1097/BRS.0000000000001063
Hollman C, Paulden M, Pechlivanoglou P, McCabe C (2017) A comparison of four software programs for implementing decision analytic cost-effectiveness models. Pharmacoeconomics 35(8):817–830. https://doi.org/10.1007/s40273-017-0510-8. (PMID: 28488257)
Mahmoudi M, Sobieraj DM (2013) The cost-effectiveness of oral direct factor Xa inhibitors compared with low-molecular-weight heparin for the prevention of venous thromboembolism prophylaxis in total hip or knee replacement surgery. Pharmacotherapy 33(12):1333–1340. https://doi.org/10.1002/phar.1269. (Epub 2013 Apr 26. PMID: 23625693)
Gómez-Outes A, Avendaño-Solá C, Terleira-Fernández AI, Vargas-Castrillón E (2014) Pharmacoeconomic evaluation of dabigatran, rivaroxaban and apixaban versus enoxaparin for the prevention of venous thromboembolism after total hip or knee replacement in Spain. Pharmacoeconomics 32(9):919–936. https://doi.org/10.1007/s40273-014-0175-5. (PMID: 24895235)
Ehresman J, Pennington Z, Schilling A et al (2020) Cost-benefit analysis of tranexamic acid and blood transfusion in elective lumbar spine surgery for degenerative pathologies. J Neurosurg Spine 33(2):177–185. https://doi.org/10.3171/2020.1.SPINE191464
Nabi V, Ayhan S, Yuksel S et al (2022) The effect of discharging patients with low hemoglobin levels on hospital readmission and quality of life after adult spinal deformity surgery. Asian Spine J 16(2):261–269. https://doi.org/10.31616/asj.2020.0629
Shander A, Hofmann A, Ozawa S, Theusinger OM, Gombotz H, Spahn DR (2010) Activity-based costs of blood transfusions in surgical patients at four hospitals. Transfusion (Paris) 50(4):753–765. https://doi.org/10.1111/j.1537-2995.2009.02518.x
Henry DA, Carless PA, Moxey AJ et al (2011) Anti-fibrinolytic use for minimising perioperative allogeneic blood transfusion. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD001886.pub3
McCormack PL (2012) Tranexamic acid: a review of its use in the treatment of hyperfibrinolysis. Drugs 72(5):585–617. https://doi.org/10.2165/11209070-000000000-00000
Vuylsteke A, Saravanan P, Gerrard C, Cafferty F (2006) The impact of administration of tranexamic acid in reducing the use of red blood cells and other blood products in cardiac surgery. BMC Anesthesiol 6(1):9. https://doi.org/10.1186/1471-2253-6-9
Gill JB, Chin Y, Levin A, Feng D (2008) The use of antifibrinolytic agents in spine surgery: a meta-analysis. J Bone Jt Surg Am 90(11):2399–2407. https://doi.org/10.2106/JBJS.G.01179
Wong J, El Beheiry H, Rampersaud YR et al (2008) Tranexamic acid reduces perioperative blood loss in adult patients having spinal fusion surgery. Anesth Analg 107(5):1479–1486. https://doi.org/10.1213/ane.0b013e3181831e44
Yang B, Li H, Wang D, He X, Zhang C, Yang P (2013) Systematic review and meta-analysis of perioperative intravenous tranexamic acid use in spinal surgery. PLoS ONE 8(2):e55436. https://doi.org/10.1371/journal.pone.0055436
Elwatidy S, Jamjoom Z, Elgamal E, Zakaria A, Turkistani A, El-Dawlatly A (2008) Efficacy and safety of prophylactic large dose of tranexamic acid in spine surgery: a prospective, randomized, double-blind, placebo-controlled study. Spine 33(24):2577–2580. https://doi.org/10.1097/BRS.0b013e318188b9c5
Wang M, Zheng XF, Jiang LS (2015) Efficacy and safety of antifibrinolytic agents in reducing perioperative blood loss and transfusion requirements in scoliosis surgery: a systematic review and meta-analysis. PLoS ONE 10(9):e0137886. https://doi.org/10.1371/journal.pone.0137886
Zhong J, Cao K, Wang B, Zhou X, Lin N, Lu H (2019) The perioperative efficacy and safety of tranexamic acid in adolescent idiopathic scoliosis. World Neurosurg 129:e726–e732. https://doi.org/10.1016/j.wneu.2019.05.261
Li G, Sun TW, Luo G, Zhang C (2017) Efficacy of antifibrinolytic agents on surgical bleeding and transfusion requirements in spine surgery: a meta-analysis. Eur Spine J 26(1):140–154. https://doi.org/10.1007/s00586-016-4792-x
Yuan QM, Zhao ZH, Xu BS (2017) Efficacy and safety of tranexamic acid in reducing blood loss in scoliosis surgery: a systematic review and meta-analysis. Eur Spine J 26(1):131–139. https://doi.org/10.1007/s00586-016-4899-0
McNicol ED, Tzortzopoulou A, Schumann R, Carr DB, Kalra A (2016) Antifibrinolytic agents for reducing blood loss in scoliosis surgery in children. Cochrane Anaesthesia Group, ed. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD006883.pub3
Xu D, Ren Z, Chen X et al (2017) The further exploration of hidden blood loss in posterior lumbar fusion surgery. Orthop Traumatol Surg Res 103(4):527–530. https://doi.org/10.1016/j.otsr.2017.01.011
Demos HA, Lin ZX, Barfield WR, Wilson SH, Robertson DC, Pellegrini VD (2017) Process improvement project using tranexamic acid is cost-effective in reducing blood loss and transfusions after total hip and total knee arthroplasty. J Arthroplasty 32(8):2375–2380. https://doi.org/10.1016/j.arth.2017.02.068
Alshryda S, Mason J, Sarda P et al (2013) Topical (intra-articular) tranexamic acid reduces blood loss and transfusion rates following total hip replacement: a randomized controlled trial (TRANX-H). J Bone Jt Surg 95(21):1969–1974. https://doi.org/10.2106/JBJS.L.00908
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
MAC-R and BS: (1) made substantial contributions to the conception or design of the work, (2) drafted the work or revised it critically for important intellectual content, (3) approved the version to be published, (4) agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. JAS-A and BS: (1) made substantial contributions to the conception or design of the work, (2) drafted the work or revised it critically for important intellectual content, (3) approved the version to be published, (4) agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. GIN-F and BS: (1) made substantial contributions to the conception or design of the work, (2) drafted the work or revised it critically for important intellectual content, (3) approved the version to be published, (4) agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. GB and BS: (1) made substantial contributions to the conception or design of the work, (2) drafted the work or revised it critically for important intellectual content, (3) approved the version to be published, (4) agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. AC and BS: (1) made substantial contributions to the conception or design of the work, (2) drafted the work or revised it critically for important intellectual content, (3) approved the version to be published, (4) agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. MR and MD: (1) made substantial contributions to the conception or design of the work, (2) drafted the work or revised it critically for important intellectual content, (3) approved the version to be published, (4) agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. SMF and MD: (1) made substantial contributions to the conception or design of the work, (2) revised the work critically for important intellectual content, (3) approved the version to be published, (4) agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. FNM and MD: (1) made substantial contributions to the conception or design of the work, (2) revised the work critically for important intellectual content, (3) approved the version to be published, (4) agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. AJ, MD, and MBA: (1) made substantial contributions to the conception or design of the work, (2) drafted the work or revised it critically for important intellectual content, (3) approved the version to be published, (4) agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval
This study was exempt from institutional review board approval as it was an analysis of publicly available data.
Consent
N/A.
Data
N/A.
Materials and/or code availability
N/A.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cartagena-Reyes, M.A., Silva-Aponte, J.A., Nazario-Ferrer, G.I. et al. The cost–utility of intraoperative tranexamic acid in adult spinal deformity patients undergoing long posterior spinal fusion. Spine Deform 12, 587–593 (2024). https://doi.org/10.1007/s43390-023-00818-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-023-00818-3